Integrating Ozempic into Physician-Led Fat Loss Protocols: Clinical Perspectives
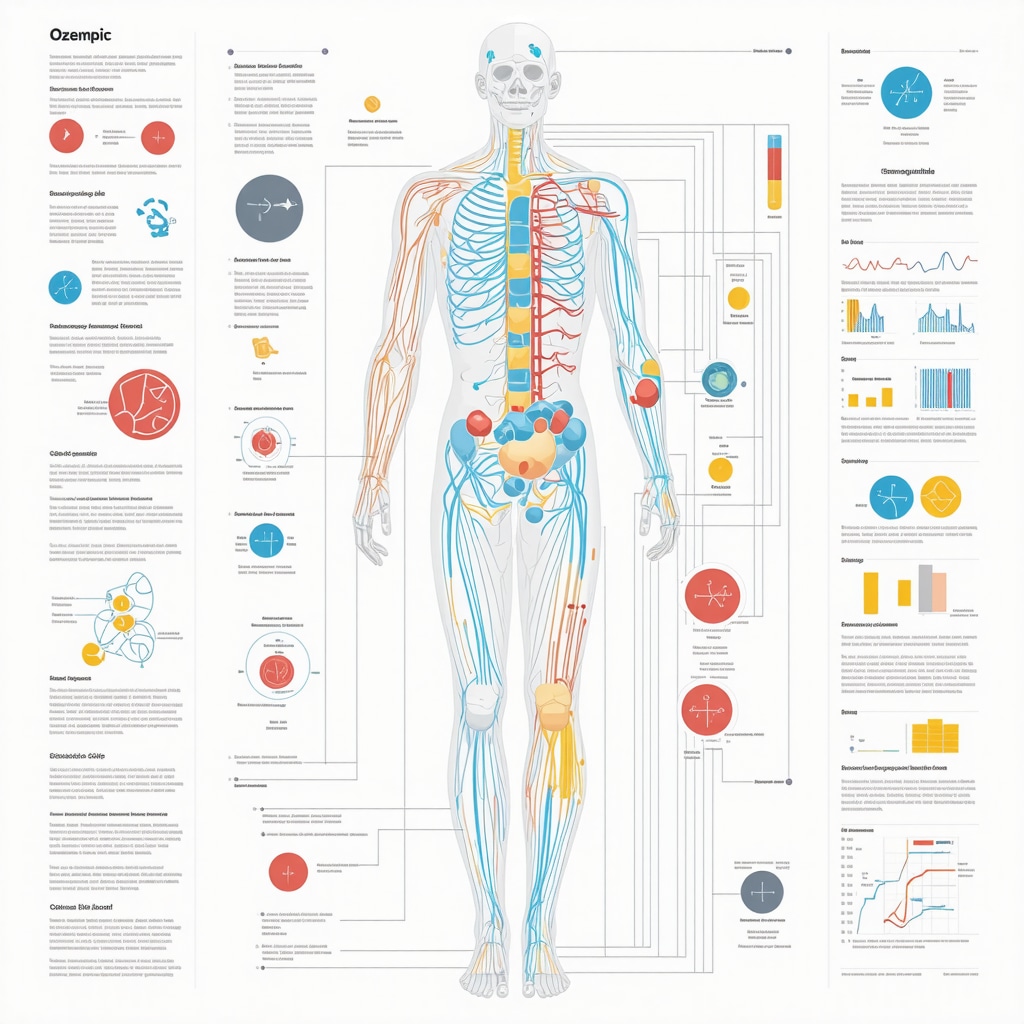
Ozempic (semaglutide) has emerged as a groundbreaking glucagon-like peptide-1 (GLP-1) receptor agonist with dual utility in glycemic control and weight management. Physician-prescribed Ozempic is increasingly recognized for its efficacy in facilitating sustained fat loss when administered under rigorous medical supervision, aligning with evidence-based protocols. This paradigm shift underscores the necessity of detailed understanding of its pharmacodynamics, dosing strategies, and safety profiles for optimal therapeutic outcomes.
Mechanistic Insights: How Ozempic Facilitates Fat Reduction Beyond Glycemic Control
At the molecular level, Ozempic enhances insulin secretion, suppresses glucagon release, and delays gastric emptying, culminating in appetite modulation and caloric intake reduction. These mechanisms translate into significant fat mass decrement in overweight and obese patients, a benefit substantiated by randomized controlled trials published in journals such as The New England Journal of Medicine. However, the fat loss trajectory is contingent on individualized titration and concomitant lifestyle interventions.
Optimizing Safety: Physician-Directed Dosing and Monitoring Protocols
Safe use of Ozempic mandates a physician-supervised regimen starting with low-dose initiation (e.g., 0.25 mg weekly) to mitigate gastrointestinal adverse effects, escalating gradually to maintenance doses typically ranging from 0.5 to 1 mg weekly. Continuous monitoring for side effects such as nausea, pancreatitis risk, and rare thyroid C-cell tumors is critical. This vigilance is integral to maximizing fat loss efficacy while safeguarding patient health, as emphasized in clinical guidelines and expert consensus documents.
What Are the Most Effective Strategies for Managing Ozempic Side Effects While Ensuring Sustained Fat Loss?
Clinicians often deploy multifaceted strategies, including dose titration, patient education on symptom management, and integration of nutritional counseling, to address common side effects like nausea and hypoglycemia. Peer-reviewed studies and clinical experience suggest that adherence to these safety practices significantly enhances patient retention and weight loss success. For comprehensive management approaches, see detailed protocols at physician-prescribed Ozempic side effect management.
Contextualizing Ozempic Within the Spectrum of GLP-1 Weight Loss Therapies
Ozempic’s unique molecular profile and dosing convenience distinguish it among GLP-1 receptor agonists, offering a compelling balance of efficacy and tolerability. Comparative analyses with agents like Wegovy and other GLP-1 analogs reveal nuanced differences in fat loss kinetics and side effect spectra, informing personalized medicine approaches in obesity treatment. For an in-depth comparative review, refer to the expert analysis at Ozempic vs Wegovy: Which GLP-1 Drug Wins in 2025.
Advancing Patient Outcomes: The Role of Physician Supervision in Sustainable Weight Management
Physician oversight ensures dynamic adjustment of Ozempic therapy tailored to patient response, comorbidities, and lifestyle factors. This approach not only amplifies fat loss outcomes but also mitigates risks associated with unsupervised use, including prescription misuse and inadequate follow-up. The integration of telehealth models further enhances accessibility and safety monitoring, as discussed in Telehealth Ozempic Prescriptions: A New Era in Weight Control.
Explore advanced clinical insights and share your professional experience with physician-guided Ozempic regimens to contribute to evolving best practices in medical weight management.
Personalizing Ozempic Therapy: Tailoring Dosage and Lifestyle Integration
While Ozempic’s pharmacological action is well-established, its optimal use requires nuanced personalization to align with individual metabolic profiles, lifestyle habits, and weight loss goals. Physicians are encouraged to incorporate detailed patient assessments, including baseline body composition analysis, comorbidity evaluation, and psychological readiness, to design bespoke titration schedules. This personalization is especially critical in balancing efficacy with tolerability, as some patients may require slower dose escalations or adjunctive behavioral interventions to sustain compliance and maximize fat reduction.
Integrating Ozempic with structured nutritional and physical activity plans enhances outcomes. Evidence suggests that combining GLP-1 agonist therapy with tailored dietary modifications—such as reduced caloric intake with a focus on macronutrient balance—and incremental exercise regimens synergistically amplifies fat loss and improves metabolic health markers.
Mitigating Long-Term Risks: Vigilance in Chronic Ozempic Administration
Given the potential for chronic use of Ozempic in weight management, long-term safety monitoring is paramount. Physicians must vigilantly screen for rare but serious adverse events, including pancreatitis and thyroid neoplasms, through periodic biochemical testing and clinical evaluation. Furthermore, emerging data indicate the importance of monitoring gastrointestinal function and nutrient absorption, as delayed gastric emptying may impact micronutrient status over extended periods.
How Can Clinicians Leverage Emerging Biomarkers to Optimize Ozempic Efficacy and Safety?
The frontier of personalized medicine in obesity treatment includes the use of biomarkers such as GLP-1 receptor expression levels, insulin sensitivity indices, and gut microbiome profiles to predict and monitor patient response to Ozempic. Harnessing these biomarkers can inform dynamic treatment adjustments, identify early signs of adverse effects, and enhance the precision of therapeutic interventions. Recent studies published in Frontiers in Endocrinology illustrate promising correlations between biomarker patterns and clinical outcomes, underscoring their potential in refining treatment paradigms.
Integrating Telehealth and Remote Monitoring: Expanding Access and Enhancing Compliance
Telemedicine platforms now enable continuous physician oversight of Ozempic therapy, facilitating regular virtual consultations, side effect management, and dosage adjustments. Remote monitoring tools, including digital scales, glucose meters, and patient-reported outcome measures, empower clinicians to track progress in real-time and promptly address emerging issues. This model aligns with modern healthcare delivery trends, improving patient engagement and adherence while maintaining safety standards.
For clinicians and patients interested in leveraging telehealth for weight loss, detailed guidance is available at Telehealth Ozempic Prescriptions: A New Era in Weight Control.
Engage with us: share your experiences or insights on physician-led Ozempic programs in the comments, and explore further expert resources to elevate your clinical practice.
Leveraging Pharmacogenomics for Tailored Ozempic Therapy in Complex Patient Profiles
As precision medicine advances, pharmacogenomic insights are becoming indispensable in optimizing Ozempic therapy for fat loss. Genetic variations affecting GLP-1 receptor sensitivity, drug metabolism enzymes like CYP450 isoforms, and appetite-regulating neuropeptides can significantly influence therapeutic efficacy and side effect susceptibility. Understanding these polymorphisms allows clinicians to anticipate variable patient responses, customize dosing regimens, and mitigate adverse events preemptively.
For instance, patients harboring certain GLP1R gene variants may experience attenuated appetite suppression, necessitating adjunctive behavioral interventions or alternative pharmacotherapies. Conversely, polymorphisms in genes related to gastrointestinal motility might predict heightened risk of nausea, guiding more conservative dose escalation. Integrating pharmacogenomic testing into clinical workflows exemplifies the cutting-edge approach to maximizing Ozempic’s fat loss potential while minimizing patient burden.
Harnessing the Gut-Brain Axis: Novel Insights into Ozempic’s Multifaceted Role in Energy Homeostasis
Beyond classic GLP-1 mediated pathways, Ozempic exerts complex modulatory effects on the gut-brain axis, influencing neuroendocrine circuits that regulate satiety, reward, and energy expenditure. Recent neuroimaging studies reveal that semaglutide attenuates activity in brain regions associated with hedonic eating, such as the hypothalamus and amygdala, thereby reducing cravings and caloric intake independently of peripheral insulin effects.
Moreover, Ozempic’s influence on vagal nerve signaling and enteroendocrine hormone release contributes to improved metabolic flexibility and increased lipolysis. These multifactorial effects underscore the necessity of integrating neuro-metabolic perspectives into treatment planning, encouraging clinicians to adopt holistic strategies that encompass behavioral therapy alongside pharmacological intervention.
How Does Ozempic Impact Long-Term Neuroplasticity Related to Appetite Control and Weight Regulation?
Emerging evidence suggests that chronic semaglutide administration may induce durable changes in neural circuits governing appetite and energy balance, potentially resetting pathological eating behaviors. Animal models demonstrate enhanced synaptic plasticity and altered neurotransmitter receptor expression in hypothalamic nuclei after prolonged GLP-1 receptor agonist exposure. Translating these findings clinically, sustained Ozempic therapy could facilitate lasting behavioral modification, reducing relapse rates post-treatment cessation.
However, longitudinal human studies remain limited, necessitating further research to elucidate the extent and clinical significance of such neuroplastic adaptations. Clinicians should remain vigilant for changes in mood or cognition during extended therapy and consider multidisciplinary collaboration with neuropsychiatric specialists when appropriate.
Integrating Continuous Glucose Monitoring (CGM) and Digital Health Tools to Refine Ozempic Regimens
The advent of continuous glucose monitoring technology offers unprecedented granularity in assessing metabolic responses to Ozempic, especially in patients with concomitant diabetes or prediabetes. Real-time glucose data enable dynamic titration of dosage to optimize glycemic and weight outcomes while reducing hypoglycemia risk. Furthermore, integrating CGM with smartphone applications facilitates patient engagement, adherence tracking, and early detection of adverse effects.
Complementing CGM, digital health platforms incorporating artificial intelligence algorithms can analyze behavioral patterns, dietary intake, and physical activity levels to provide personalized feedback and motivation. These tools bridge the gap between clinic visits, fostering continuous support and reinforcing lifestyle modifications essential for sustained fat loss.
For a comprehensive overview of technological innovations augmenting Ozempic therapy, consult the detailed synthesis at Digital Health Integration in Ozempic Weight Management.
Ethical Considerations and Health Equity in Physician-Prescribed Ozempic Therapy
While Ozempic offers remarkable benefits, equitable access remains a critical concern. Socioeconomic disparities, insurance coverage limitations, and geographic barriers may restrict availability for underserved populations. Physicians must advocate for inclusive policies and consider cost-effective adjunctive strategies to ensure broader therapeutic reach.
Additionally, ethical prescribing mandates thorough patient education regarding potential side effects, realistic expectations, and the importance of adherence. Shared decision-making frameworks empower patients, fostering trust and optimizing outcomes. Ongoing clinician training in cultural competence and communication skills is essential to address diverse patient needs effectively.
Engaging with multidisciplinary teams, including dietitians, behavioral therapists, and community health workers, can mitigate structural obstacles and enhance holistic care delivery.
Discover more about the intersection of personalized medicine and technology in optimizing Ozempic therapy by exploring our advanced clinical resources and contributing your insights.
Pharmacogenomic Tailoring: Unlocking Genetic Influences on Ozempic Responsiveness
Incorporating pharmacogenomics into Ozempic administration transcends traditional dosing paradigms, enabling clinicians to decipher polymorphic variations in genes such as GLP1R and cytochrome P450 enzymes that modulate semaglutide metabolism and receptor sensitivity. This genomic insight facilitates stratified patient selection, optimizing therapeutic index while preemptively identifying individuals prone to suboptimal appetite suppression or heightened adverse effects like gastrointestinal intolerance. Emerging genotyping platforms integrated within clinical workflows bolster this personalized approach, ensuring precision in titration and adjunctive therapy integration.
Neuro-Metabolic Synergy: Decoding the Gut-Brain Axis Modulation by Semaglutide
Beyond peripheral endocrinology, Ozempic orchestrates intricate neuro-metabolic interactions via modulation of hypothalamic and limbic circuitry that govern satiety and reward. Functional MRI studies corroborate diminished activation in hedonic eating centers, aligning with clinically observed reductions in cravings and caloric intake. Concurrently, semaglutide’s influence on vagal afferents and enteroendocrine feedback loops potentiates metabolic flexibility and lipolysis, elucidating a multifaceted mechanism underpinning sustained fat loss. These insights advocate for integrated therapeutic regimens marrying pharmacotherapy with cognitive-behavioral strategies to consolidate neuroplastic adaptations.
How Can Integration of Biomarkers and Digital Health Enhance Individualized Ozempic Regimens?
Advanced clinical practice increasingly leverages biomarker analytics, including GLP-1 receptor density assays, insulin sensitivity indices, and gut microbiome composition, to forecast and monitor patient-specific responses to Ozempic. Coupled with continuous glucose monitoring (CGM) and AI-driven digital health platforms, these data streams enable dynamic, responsive dose adjustments and behavioral reinforcement, mitigating adverse events and optimizing weight loss trajectories. This precision medicine framework fosters real-time clinician-patient collaboration, enhancing adherence and therapeutic efficacy.
Ethical Imperatives and Equity in Access: Bridging Gaps in Physician-Prescribed Ozempic Utilization
While Ozempic epitomizes a therapeutic breakthrough, equitable dissemination remains challenged by socioeconomic and systemic barriers. Physicians must advocate for policy reforms and deploy culturally competent communication to mitigate disparities in treatment accessibility. Integrating multidisciplinary support networks, including telemedicine and community health initiatives, can democratize access and uphold ethical standards in obesity management. Such strategies ensure that the transformative potential of semaglutide-based therapies benefits diverse populations without exacerbating health inequities.
For clinicians and researchers poised to elevate their practice, delve deeper into these advanced pharmacogenomic and neuro-metabolic paradigms to refine Ozempic protocols and foster sustainable fat loss outcomes. Engage with our expert community to exchange insights and propel innovation in obesity therapeutics.
Expert Insights & Advanced Considerations
Pharmacogenomic Profiling as a Cornerstone for Personalized Ozempic Therapy
Integrating pharmacogenomic data into Ozempic prescribing protocols enables clinicians to tailor treatment based on individual genetic variations affecting GLP-1 receptor sensitivity and semaglutide metabolism. This precision approach mitigates adverse effects and enhances therapeutic efficacy, fostering more predictable fat loss outcomes in complex patient cohorts.
Neuro-Metabolic Modulation: Beyond Peripheral Appetite Suppression
Semaglutide’s impact on the gut-brain axis involves attenuation of hedonic eating centers and modulation of vagal afferents, which contributes to sustained appetite control and improved metabolic flexibility. Recognizing these neuroplastic effects encourages coupling pharmacotherapy with behavioral interventions to consolidate lasting weight regulation.
Leveraging Continuous Glucose Monitoring and Digital Health for Dynamic Dose Adjustment
Utilizing CGM data alongside AI-powered digital platforms offers a granular, real-time view of metabolic responses to Ozempic, facilitating individualized dosing and timely management of side effects. This integration promotes adherence and optimizes fat loss trajectories through proactive, data-driven clinical decisions.
Ethical Imperatives and Strategies to Bridge Access Disparities
Advocating for equitable access to Ozempic involves addressing socioeconomic barriers through culturally competent communication and multidisciplinary support frameworks. Telehealth and community health initiatives are vital tools to democratize treatment availability without compromising safety or efficacy.
Synergistic Protocols: Combining Ozempic with Lifestyle and Behavioral Therapies
Maximizing fat loss efficacy demands comprehensive protocols integrating Ozempic therapy with individualized nutritional planning and cognitive-behavioral strategies. This holistic approach harnesses semaglutide’s multifaceted mechanisms while promoting sustainable lifestyle modifications.
Curated Expert Resources
- New England Journal of Medicine (NEJM): Seminal randomized controlled trials on semaglutide’s efficacy and safety provide rigorous clinical evidence foundational to physician-prescribed Ozempic programs (NEJM Semaglutide RCT).
- Frontiers in Endocrinology: Cutting-edge research on biomarkers and neuroendocrine mechanisms underpinning Ozempic’s therapeutic action, critical for advanced clinical applications (Frontiers Biomarker Insights).
- WeightLossSuppliers.com Physician Guides: Comprehensive protocols and expert tips for safely navigating side effects, dosing strategies, and telehealth integration enhance clinical practice (Managing Ozempic Side Effects).
- Digital Health Integration in Weight Management: Resources on leveraging CGM and AI for optimizing Ozempic regimens provide actionable insights for contemporary practice (Digital Health and Ozempic).
- Comparative Analyses of GLP-1 Therapies: In-depth reviews such as Ozempic vs Wegovy facilitate informed therapeutic choices and personalized patient care.
Final Expert Perspective
Physician-prescribed Ozempic represents a sophisticated convergence of pharmacology, genomics, neurobiology, and digital health innovation in the pursuit of sustainable fat loss. Its multifaceted mechanisms necessitate a precision medicine framework that embraces individualized dosing, biomarker integration, and holistic lifestyle support. Concurrently, ethical stewardship and equitable access remain paramount to fully realize its transformative potential across diverse populations.
Clinicians and researchers are encouraged to deepen their mastery through advanced resources and engage with expert communities to refine protocols continuously. Explore the nuances of comparative GLP-1 therapies in Ozempic vs Wegovy: Which GLP-1 Drug Wins in 2025 and discover comprehensive strategies for side effect management at Managing Ozempic Side Effects. Your active participation enriches the evolving landscape of medical weight loss and elevates patient outcomes globally.


I found this detailed review of physician-guided Ozempic use incredibly insightful, especially the emphasis on personalized dosing strategies and safety protocols. Incorporating biomarker analysis and telehealth tools seems like the future of weight management, making treatments more precise and accessible. In my experience working with patients, one of the biggest challenges is balancing efficacy with tolerability, particularly managing side effects like nausea without compromising fat loss goals. Do you think as pharmacogenomics becomes more integrated into practice, we might see a shift towards even more tailored therapies that account for genetic differences early on? I’m curious about anyone’s thoughts on how realistic it is to implement this in routine clinical settings within the next few years, especially considering access and cost barriers.