Why Injection Technique Isn’t Just a Needle Point
Imagine this: you’ve got your Ozempic pen in hand, ready to embark on that medical weight loss journey you’ve been contemplating. But wait — the way you jab that little wonder device under your skin could make all the difference between a smooth ride and a bumpy one. Doctor-supervised Ozempic treatments aren’t just about handing over a prescription; they’re about mastering the injection techniques that optimize effectiveness and minimize discomfort.
Injecting Confidence: What Your Doctor Wants You to Know
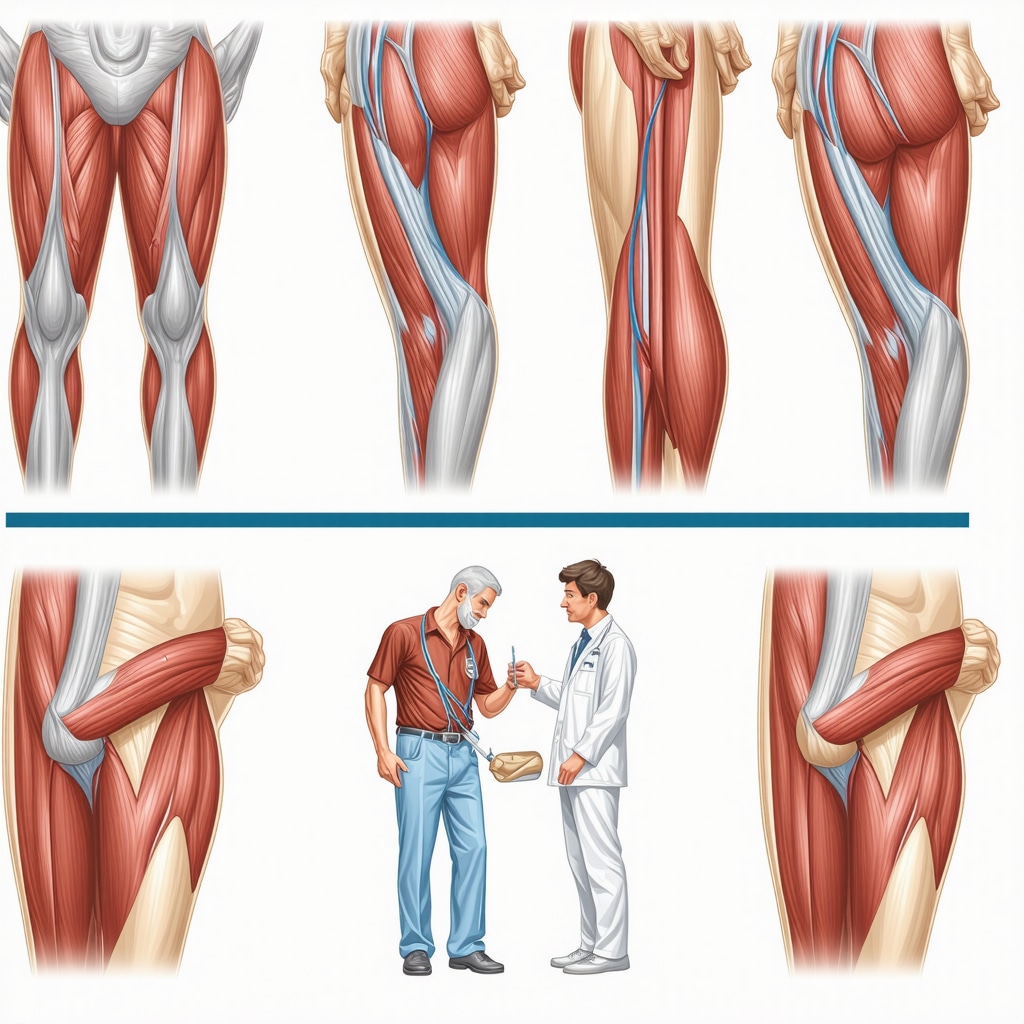
Let’s face it, the idea of self-injecting a medication can be intimidating. Yet, with professional guidance, the process becomes empowering. Doctors emphasize rotating injection sites — usually the abdomen, thigh, or upper arm — to avoid skin irritation or lumps. The injection itself is quick: a subcutaneous shot, meaning it goes just below the skin’s surface, not into the muscle. Proper technique means holding the needle in place for a few seconds to ensure full dose delivery, then disposing of the pen needle safely.
Is There a ‘Right’ Way to Inject Ozempic, or Is It Just Personal Preference?
Excellent question! While the basics are consistent, subtle nuances in injection technique can vary based on patient body type, comfort, and even the season—yes, you heard right. For example, colder weather might make skin less pliable, so warming the pen in your hand beforehand can ease the process. Moreover, doctors often tailor advice on needle angle and site selection to fit your lifestyle and physical condition, underscoring the value of doctor-supervised Ozempic treatments over DIY approaches.
Injecting Safety: Avoiding Common Pitfalls
Injecting Ozempic with finesse is not just about comfort—it’s about safety. Improper injection can lead to bruising, infection, or inconsistent dosing, jeopardizing your weight loss goals. That’s why supervision and education from healthcare providers are crucial. They coach you on hygiene, needle disposal, and recognizing signs that might indicate injection site reactions. For those wanting a deep dive into injection safety, the doctor-supervised Ozempic treatments injection safety guidelines provide a treasure trove of expert tips.
Why Trusting the Process Makes All the Difference
In this age of digital health trends, it’s tempting to skip the doctor’s office and jump straight to self-medication. But the nuances of injectable weight loss drugs like Ozempic demand expert oversight. The FDA-approved medication, backed by clinical research and expert consensus, shines brightest when combined with physician guidance. According to a review published in The New England Journal of Medicine, proper administration and monitoring significantly enhance both safety and treatment outcomes.
Ready to take charge with confidence? Share your injection stories or questions below — your experience might just help someone else navigate their Ozempic journey. And if you’re curious how Ozempic stacks up against similar GLP-1 drugs, check out our insightful Ozempic vs. Wegovy comparison for a deeper dive.
Harnessing the Power of Personalized Injection Techniques
While basic injection protocols are indispensable, expert clinicians recognize that individual patient factors can influence the effectiveness of Ozempic administration. Factors such as skin thickness, fat distribution, and even daily activity levels contribute to determining optimal injection sites and angles. Customized injection strategies, developed through physician supervision, not only enhance comfort but can also improve drug absorption and consistency, which ultimately supports sustained weight loss results. This personalized approach is a cornerstone of successful doctor-supervised Ozempic treatments.
Navigating Injection Challenges: From Site Reactions to Dose Adjustments
Even with perfect technique, some patients may experience localized skin reactions or discomfort. These can often be mitigated through simple adjustments, such as alternating injection sites more frequently or altering needle angles. Importantly, patient feedback during regular monitoring sessions allows healthcare providers to tailor dosage increments and manage side effects proactively. This dynamic process ensures that weight loss progression is not derailed by avoidable setbacks. For comprehensive strategies on managing these challenges, see our detailed guide on navigating Ozempic side effects.
How Does Physician-Guided Injection Technique Impact Long-Term Weight Loss Outcomes?
This question probes the critical link between expert oversight and sustainable fat loss. Research demonstrates that patients receiving thorough injection education and ongoing clinical support exhibit higher adherence rates and better weight loss maintenance compared to those self-administering without supervision. The reason lies in the nuanced adjustments experts make—whether refining injection sites, managing side effects, or coordinating Ozempic use with lifestyle interventions such as diet and exercise. This holistic, patient-centered care model is supported by leading endocrinology experts, including those contributing to authoritative sources like the National Institutes of Health.
Engaging with a knowledgeable healthcare provider enables you to navigate complexities and optimize treatment efficacy with confidence. Share your experiences or questions about injection techniques below to support our community’s journey. For those exploring comprehensive weight loss strategies, don’t miss our expert insights on combining Ozempic with fitness plans for amplified results.
Decoding the Science Behind Injection Site Selection: Beyond Surface-Level Choices
While it might seem that choosing an injection site is merely a matter of convenience or comfort, the science tells a far more nuanced story. The pharmacokinetics of Ozempic are influenced by subcutaneous tissue characteristics, including blood flow, fat layer thickness, and local enzymatic activity. For instance, abdominal injections generally provide more consistent absorption due to richer vascularization compared to thigh or arm sites. However, individual variability demands personalized site rotation schedules to mitigate risks such as lipohypertrophy or localized fibrosis, which can impair drug uptake. In clinical practice, advanced imaging techniques like ultrasound can be employed to assess subcutaneous tissue depth, allowing physicians to tailor needle length and angle optimally for each patient.
What Are the Biomechanical and Physiological Factors That Affect Ozempic Absorption at Different Injection Sites?
Understanding the interplay between biomechanics and physiology is crucial for mastering injection technique. Subcutaneous tissue thickness varies with age, sex, BMI, and even hydration status, influencing both the diffusion rate and bioavailability of semaglutide. A study published in Diabetes Care highlights that injections administered in areas with optimal adipose tissue thickness yield more reliable plasma concentration profiles, reducing fluctuations that can affect efficacy and side effects. Furthermore, mechanical stress and repetitive injections in the same area may alter local tissue perfusion, underscoring the importance of site rotation and patient education.
These insights emphasize why physician-guided injection protocols incorporate patient-specific assessments rather than relying on one-size-fits-all approaches. By leveraging detailed anatomical knowledge and patient feedback, healthcare providers can formulate dynamic injection plans that enhance both drug delivery and patient comfort.
Integrating Technology into Injection Training: Virtual Reality and AI-Driven Feedback
The digital revolution is reshaping how patients learn and perfect injection techniques. Cutting-edge virtual reality (VR) platforms now simulate the injection process, allowing patients to practice in a risk-free environment with real-time, AI-generated feedback on needle angle, depth, and site selection. Such immersive training tools have demonstrated improved confidence and reduced anxiety, translating into fewer injection errors and enhanced adherence.
Moreover, emerging smart injection pens equipped with sensors and Bluetooth connectivity provide clinicians with detailed usage data, including injection timing, dosage accuracy, and site rotation patterns. This data-driven approach enables personalized coaching and early intervention if suboptimal techniques are detected, fostering a proactive rather than reactive treatment model. The integration of these technologies aligns with the precision medicine paradigm, optimizing outcomes through tailored, data-informed strategies.
Managing Complex Cases: Injection Strategies for Patients with Variable Skin Conditions or Comorbidities
Patients presenting with dermatological conditions such as psoriasis, eczema, or scarring pose unique challenges for Ozempic administration. Injecting into compromised skin can exacerbate irritation or impair absorption. Expert clinicians often recommend alternative sites or adjusting needle length and angle to bypass affected areas, ensuring both safety and efficacy. Additionally, comorbidities like lipodystrophy or edema necessitate careful site selection and frequent monitoring.
In such complex scenarios, interdisciplinary collaboration becomes paramount. Dermatologists, endocrinologists, and diabetes educators work synergistically to develop comprehensive injection protocols. This multidisciplinary approach exemplifies the advanced level of care that distinguishes doctor-supervised Ozempic treatments from unsupervised regimens.
Can Advanced Injection Techniques Mitigate Side Effects in Patients with Complicated Skin Profiles?
Indeed, specialized injection strategies can significantly reduce adverse reactions in sensitive patients. Techniques such as micro-rotations within a single anatomical site, pre-injection skin preparation with barrier creams, or the use of ultra-fine needles have been shown to decrease local inflammation and discomfort. According to a recent clinical review in Journal of the American Academy of Dermatology, these tailored interventions contribute to sustained treatment adherence and better clinical outcomes.
Patients facing these challenges should engage in open dialogue with their healthcare team to explore personalized solutions. Remember, mastering injection technique is a dynamic, evolving process—your feedback is invaluable in refining your treatment plan.
Curious about how to elevate your injection routine or integrate emerging technologies into your Ozempic journey? Dive deeper with our expert-led resources and share your questions with our community. Together, we can unlock the full potential of doctor-supervised Ozempic treatments for transformative, sustained weight loss.
Elevating Your Ozempic Injection Routine with Expert Precision
Beyond the basic injection steps lies a realm of advanced techniques that can significantly enhance the efficacy and comfort of your Ozempic treatment. Expert clinicians emphasize that injection is not a mere mechanical act but a personalized intervention tuned to your unique physiology. This includes fine-tuning needle insertion angle, depth, and site rotation frequency based on individual tissue characteristics and lifestyle factors. For example, patients with higher BMI might benefit from longer needles and abdominal sites with ample subcutaneous fat, whereas leaner individuals may require shallower angles to avoid intramuscular delivery.
How Can Tailored Injection Schedules and Techniques Optimize Ozempic Absorption Over Time?
Injection timing and site selection are dynamic components of a successful treatment plan. Clinical evidence indicates that systematically rotating injection sites not only prevents lipohypertrophy but also sustains consistent semaglutide plasma levels, which are vital for maintaining steady appetite suppression and glycemic control. Moreover, spacing injections in a pattern that aligns with your daily routines can improve adherence and reduce injection-related anxiety. Emerging research, such as findings published in Diabetes Care, underscores how pharmacokinetic profiles vary with injection site and technique, reinforcing the need for physician-led customization.
These nuanced adjustments are best managed within doctor-supervised Ozempic treatment programs, where continuous monitoring allows for iterative refinements that optimize both drug absorption and patient comfort. This iterative process is supported by robust clinical frameworks detailed in doctor-supervised Ozempic treatments, which emphasize education, feedback, and personalized care.
Leveraging Data and Patient Feedback: The Future of Injection Technique Optimization
As we move towards precision medicine, integrating patient-reported outcomes and smart device data is revolutionizing injection technique management. Smart pens that track injection time, dosage, and angle provide clinicians with actionable insights to preempt suboptimal dosing or adverse site reactions. This data-driven approach fosters a proactive model of care, where physician intervention is timely and tailored, enhancing long-term adherence and weight loss outcomes. Patients encouraged to maintain detailed injection logs and symptom diaries become active partners in their treatment journey, enabling a feedback loop that continuously refines their protocol.
Psychological and Behavioral Aspects: Building Confidence and Reducing Injection-Related Anxiety
Injection technique mastery isn’t solely a physical skill but also a psychological journey. Many patients initially experience apprehension or discomfort, which can undermine adherence. Comprehensive doctor-supervised programs incorporate behavioral coaching, relaxation techniques, and gradual exposure strategies to build injection confidence. These interventions have been linked to improved patient satisfaction and sustained use, critical factors for long-term weight loss success.
What Role Does Ongoing Physician Support Play in Maintaining Injection Technique and Treatment Motivation?
Ongoing physician engagement is pivotal not just for technical guidance but also for motivational reinforcement. Regular follow-ups provide opportunities to troubleshoot technique challenges, adjust dosing, and celebrate progress, fostering a therapeutic alliance that enhances patient commitment. According to recent guidelines from leading endocrinology societies, continuous education and support markedly improve persistence with injectable therapies like Ozempic, thereby amplifying clinical benefits (doctor-supervised Ozempic treatments tips).
Whether you are just starting or refining your Ozempic routine, engaging with a knowledgeable healthcare provider can transform injections from a source of anxiety into an empowering act of self-care. We invite you to share your questions or success stories in the comments below — your insights could be the inspiration someone else needs on their weight loss journey. For those intrigued by how Ozempic compares to other GLP-1 options, explore our detailed Ozempic vs. Wegovy comparison to inform your path forward.

Expert Insights & Advanced Considerations
Precision Injection Technique Elevates Therapeutic Outcomes Beyond Basic Protocols
Clinicians with extensive experience emphasize that mastering injection technique is not a one-and-done skill. Instead, it requires continuous refinement tailored to individual physiology and treatment response. Factors such as needle gauge, insertion angle, and site-specific tissue characteristics dynamically influence semaglutide bioavailability. Thus, iterative physician-guided adjustments enhance both efficacy and patient comfort over time, optimizing long-term weight loss trajectories.
Integrating Real-Time Data Enhances Personalized Injection Protocols
The advent of smart injection devices providing detailed usage analytics revolutionizes clinical oversight. Physicians can monitor adherence patterns, injection timing, and site rotation remotely, enabling proactive interventions before adverse effects or dosing errors occur. This data-driven approach aligns with precision medicine paradigms, transforming Ozempic administration from a static regimen into a responsive, patient-centered process.
Psychobehavioral Support is Crucial for Sustained Injection Adherence
Beyond anatomical and pharmacokinetic factors, psychological barriers such as injection anxiety significantly impact treatment persistence. Doctor-supervised programs integrating behavioral coaching techniques—including relaxation training and motivational interviewing—have demonstrated improvements in patient confidence, reducing dropout rates and fostering consistent use essential for weight loss success.
Multidisciplinary Collaboration Optimizes Care in Complex Patient Profiles
Patients with dermatological comorbidities or metabolic complications benefit from collaborative care models. Coordinated efforts among endocrinologists, dermatologists, and diabetes educators enable tailored injection strategies that minimize adverse skin reactions and maximize drug absorption. This comprehensive approach exemplifies the advanced care standard in supervised Ozempic treatments.
Dynamic Injection Site Rotation Prevents Tissue Complications and Maintains Pharmacokinetic Consistency
Regularly altering injection sites mitigates risks such as lipohypertrophy and localized fibrosis, which can compromise semaglutide uptake. Physician-guided rotation schedules, informed by anatomical assessment and patient feedback, maintain steady plasma drug levels, essential for sustained appetite regulation and metabolic control.
Curated Expert Resources
1. National Institutes of Health (NIH) – Semaglutide Pharmacokinetics and Clinical Guidelines
This authoritative source provides detailed insights into the pharmacological profiles of GLP-1 receptor agonists, including semaglutide, underpinning evidence-based injection practices.
2. The New England Journal of Medicine – Clinical Reviews on Injectable Weight Loss Therapies
Offers peer-reviewed analyses on the safety, efficacy, and administration techniques of Ozempic, valuable for clinicians seeking in-depth understanding.
3. Journal of the American Academy of Dermatology – Dermatologic Management in Injection Therapy
Specializes in addressing skin-related challenges in injection regimens, guiding multidisciplinary approaches for patients with complex dermatologic conditions.
4. Diabetes Care – Pharmacokinetics of Subcutaneous Semaglutide
Provides research-backed data on how injection site and technique influence semaglutide absorption, critical for personalized treatment planning.
5. WeightLossUppliers.com – Doctor-Supervised Ozempic Treatments Injection Best Practices
A comprehensive, clinician-endorsed resource offering practical guidance on injection technique optimization and patient education tailored for sustained weight loss success.
Final Expert Perspective
Unlocking the full potential of doctor-supervised Ozempic treatments hinges on a multifaceted approach that transcends mere needle insertion. It demands an integration of precision pharmacology, cutting-edge technology, behavioral science, and multidisciplinary collaboration. Tailoring injection techniques to individual patient profiles ensures consistent drug delivery, minimizes adverse effects, and supports sustained weight loss outcomes. Embracing these advanced considerations transforms Ozempic use from a routine procedure into a dynamic, patient-centered therapeutic strategy.
We encourage healthcare professionals and patients alike to engage deeply with these insights, share experiences, and explore related resources such as our guide on doctor-supervised Ozempic treatments and the Ozempic vs. Wegovy comparison. For personalized support or to discuss advanced injection protocols, visit our contact page—your journey toward optimized weight management deserves expert partnership.


This article provides a comprehensive overview of the critical importance of proper injection techniques for Ozempic. I agree that personalized strategies, guided by a healthcare provider, can significantly enhance both comfort and efficacy. From personal experience, rotating injection sites has helped me avoid lumps and skin irritation, making the process less daunting. The mention of advanced technologies like AI feedback and smart pens is exciting—it could really take patient education to the next level.
One question I have is about dealing with injection site reactions, especially for those with sensitive skin or dermatologic issues. Has anyone found specific techniques or products that effectively reduce irritation? It would be helpful to hear about practical tips or personal remedies that others have used successfully. Also, do you think virtual reality training could help new patients build confidence before their first injection? This seems like a promising area to explore for improving adherence and overall treatment experience.