Understanding the Mechanistic Foundations of Ozempic in Weight Management
Ozempic, an injectable glucagon-like peptide-1 (GLP-1) receptor agonist, has emerged as a groundbreaking pharmaceutical agent in medical weight loss, primarily due to its multifaceted metabolic effects. By modulating appetite regulation and enhancing glycemic control, it facilitates significant fat mass reduction. Its pharmacodynamics include delayed gastric emptying and central appetite suppression, mechanisms vital for sustainable weight loss trajectories.
Week-by-Week Physiological Adaptations: Mapping Ozempic’s Impact on Fat Loss
Initial weeks of Ozempic administration typically reveal appetite diminution alongside modest weight decrements, predominantly from adipose tissue reduction. Clinical data suggest that from weeks 1 to 4, patients experience a measurable shift in energy balance, often corroborated by decreased caloric intake and improved insulin sensitivity. Progressing into weeks 5 through 8, enhanced lipolysis and metabolic rate stabilization become apparent, underpinning accelerated fat mass loss.
What are the optimal clinical strategies to maximize Ozempic’s efficacy while managing side effects?
Optimizing Ozempic’s therapeutic potential requires a clinician-guided approach emphasizing individualized dosage titration coupled with adjunct lifestyle modifications. Mitigating adverse effects such as nausea and gastrointestinal discomfort involves gradual dose escalation and patient education. Integrating dietary adjustments and physical activity amplifies fat loss outcomes and supports metabolic health. For detailed protocols, consult authoritative resources such as physician-prescribed Ozempic expert tips.
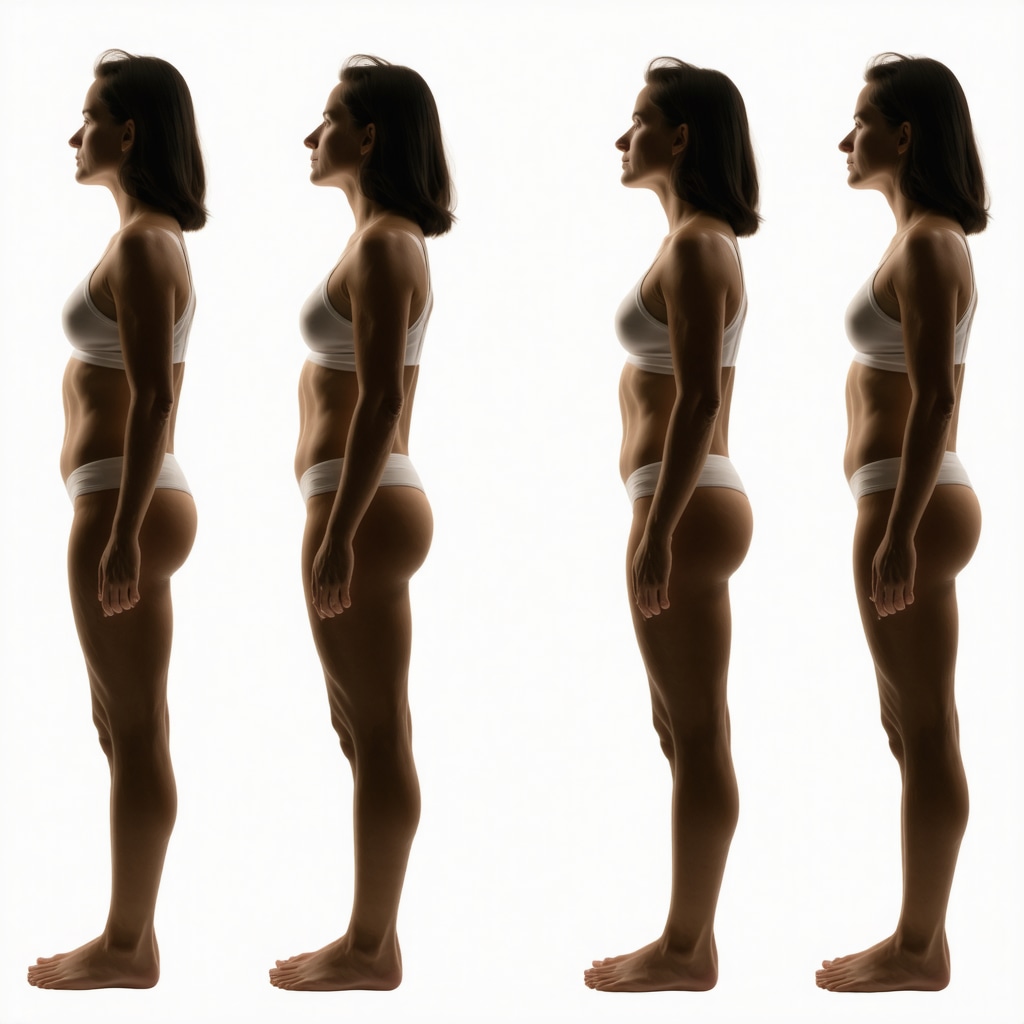
Interpreting Before and After Transformations: Objective Metrics and Patient Experience
Quantitative assessment of fat loss transformation under Ozempic therapy mandates precise tracking of body composition metrics over time. Advanced imaging and bioimpedance techniques reveal reductions in visceral and subcutaneous fat deposits, correlating with improved metabolic biomarkers. Patient-reported outcomes further illuminate enhanced quality of life and psychological benefits, underscoring the holistic impact of GLP-1 based interventions.
Integrating Ozempic with Comprehensive Weight Loss Programs: Beyond Pharmacotherapy
While Ozempic’s pharmacological action is pivotal, its integration within multidisciplinary weight management programs ensures long-term efficacy. Structured nutritional counseling, behavioral therapy, and supervised physical activity synergize with Ozempic to potentiate fat loss and mitigate weight regain. Such integrative approaches align with evidence-based guidelines from leading endocrinology and obesity research institutions.
Expert Guidance for Patients Considering Ozempic: Navigating Treatment Pathways
Prospective candidates for Ozempic therapy should seek care from certified medical weight loss clinics specializing in GLP-1 receptor agonists. Proper selection of providers ensures adherence to safety protocols and personalized treatment plans. Explore our comprehensive guide on choosing the right Ozempic specialist to optimize outcomes and minimize risks.
Enhancing Patient Outcomes Through Real-World Success Stories and Data Analytics
Patient transformations documented on platforms like Ozempic before and after real patient transformations provide invaluable experiential insights, illustrating typical progress patterns and variability. Leveraging such data supports clinicians in setting realistic expectations and customizing interventions.
Interested in advanced weight loss strategies? Explore our expert-curated content on prescription weight loss with Ozempic to deepen your understanding and share your professional insights.
For authoritative clinical guidelines and research data on GLP-1 receptor agonists in obesity management, refer to the recent comprehensive review published by the National Institutes of Health (NIH), detailing mechanistic pathways and therapeutic outcomes.
Personalizing Ozempic Therapy: The Role of Genetic and Metabolic Profiling
Emerging research highlights the potential benefits of tailoring Ozempic treatment regimens based on individual genetic markers and metabolic profiles. Variations in GLP-1 receptor expression and differences in insulin sensitivity may influence patient responsiveness to semaglutide, the active compound in Ozempic. By integrating pharmacogenomics and metabolic phenotyping, clinicians can optimize dosing schedules, enhance efficacy, and reduce adverse effects, paving the way for precision medicine approaches in obesity management.
Addressing Therapeutic Challenges: Managing Tachyphylaxis and Weight Regain
One clinical challenge observed with prolonged Ozempic use is tachyphylaxis, where patients experience diminishing appetite suppression and plateauing weight loss after initial success. Understanding the underlying mechanisms—such as receptor downregulation or adaptive metabolic changes—is critical for devising strategies to sustain fat loss. Combination therapies, including adjunctive medications or intermittent dosing schedules, are currently under investigation to mitigate these effects and support long-term weight management.
How can advanced monitoring techniques transform clinical management of Ozempic therapy for optimal fat loss?
Advanced monitoring, such as continuous glucose monitoring (CGM) and body composition analysis using dual-energy X-ray absorptiometry (DEXA), allows for real-time assessment of metabolic responses and fat distribution changes. These tools empower clinicians to make informed adjustments to treatment plans and engage patients through tangible progress visualization. Incorporating digital health platforms for symptom tracking and adherence support further enhances clinical outcomes.
Clinicians aiming to integrate these advanced monitoring strategies can explore detailed protocols in resources like our doctor supervised Ozempic treatments guide, ensuring safety and maximizing therapeutic success.
Exploring Ozempic Beyond Weight Loss: Cardiometabolic Benefits and Emerging Indications
Beyond its weight reduction capabilities, Ozempic exhibits cardioprotective effects, including reductions in blood pressure, lipid profile improvements, and decreased incidence of cardiovascular events in high-risk populations. These benefits are mediated through both direct and indirect mechanisms related to improved insulin sensitivity and anti-inflammatory pathways. Ongoing clinical trials are investigating Ozempic’s potential roles in managing non-alcoholic fatty liver disease (NAFLD) and polycystic ovary syndrome (PCOS), expanding its therapeutic horizon.
Integrating Patient-Centered Communication in Ozempic Adoption
Effective communication strategies that address patient concerns about side effects, injection techniques, and realistic expectations are paramount for adherence. Shared decision-making models foster patient engagement and empower individuals to actively participate in their weight loss journey. Providers should emphasize the importance of combining pharmacotherapy with lifestyle modifications for durable results.
For more on managing side effects and optimizing patient outcomes, visit our comprehensive resource on navigating Ozempic side effects in weight loss programs.
Authoritative guidance on the evolving role of GLP-1 receptor agonists in obesity and metabolic disorder management is available from the American Heart Association Journal, providing comprehensive evidence supporting Ozempic’s multi-system benefits.
Engage with Us: Share Your Experiences or Questions About Advanced Ozempic Therapy
We invite healthcare professionals and patients alike to contribute their insights or inquiries in the comments section below. Sharing real-world experiences enriches the community and fosters continuous learning. To further explore evidence-based approaches, consider reading our in-depth article on Ozempic vs Wegovy: Which GLP-1 Drug Wins in 2025.
Decoding Pharmacokinetic Variability: Implications for Personalized Ozempic Dosing
Pharmacokinetic variability in semaglutide metabolism significantly influences therapeutic outcomes and tolerability profiles among diverse patient populations. Factors such as hepatic function, renal clearance, and concomitant medications can alter drug bioavailability, necessitating tailored dosing regimens. Recent pharmacogenomic studies have identified polymorphisms in genes encoding for drug transporters and metabolizing enzymes, which may predict differential exposure to Ozempic, thereby guiding clinicians in precision dosing strategies to optimize fat loss efficacy while minimizing adverse events.
Harnessing Digital Therapeutics and AI-Powered Monitoring to Enhance Ozempic Treatment Compliance
Integrating digital health platforms equipped with artificial intelligence algorithms offers transformative potential in managing Ozempic therapy. These platforms enable continuous patient engagement through real-time symptom tracking, adherence reminders, and behavioral nudges tailored to individual response patterns. Machine learning models can analyze biometric data streams—such as activity levels, glucose trends, and appetite cues—to predict suboptimal responses or emergent side effects, allowing proactive clinical interventions. This convergence of pharmacotherapy and digital therapeutics heralds a new paradigm in sustainable weight management.
What novel biomarkers are emerging to predict and monitor patient responsiveness to Ozempic in clinical practice?
Emerging biomarker research focuses on metabolic, inflammatory, and gut microbiome signatures that correlate with Ozempic responsiveness. Circulating levels of fibroblast growth factor 21 (FGF21), adiponectin, and specific cytokine profiles provide insights into metabolic adaptations during therapy. Moreover, gut microbial diversity and composition have been implicated in modulating GLP-1 receptor agonist efficacy. Longitudinal monitoring of these biomarkers presents an opportunity to refine patient selection and dynamically adjust treatment plans, enhancing personalized medicine in obesity care. For comprehensive biomarker validation studies, see the detailed meta-analysis published in Nature Metabolism.
Addressing Long-Term Sustainability: Psychological and Behavioral Dimensions in Ozempic-Assisted Weight Loss
The psychological landscape of weight loss under Ozempic therapy encompasses complex behavioral adaptations, motivation shifts, and identity reformation. Sustained fat loss requires addressing cognitive-emotional factors such as reward sensitivity, food cravings, and body image perception. Incorporating cognitive-behavioral therapy (CBT) and motivational interviewing alongside pharmacotherapy enhances patient resilience against relapse and supports maintenance of lifestyle modifications. This biopsychosocial approach acknowledges that Ozempic’s pharmacodynamics are potentiated by complementary behavioral health strategies.
Future Horizons: Investigating Combination Therapies and Novel GLP-1 Receptor Agonist Formulations
Current research is exploring synergistic combinations of Ozempic with other metabolic agents, such as sodium-glucose cotransporter 2 (SGLT2) inhibitors and amylin analogs, to amplify fat loss and counteract tachyphylaxis. Additionally, next-generation GLP-1 receptor agonists with enhanced receptor selectivity and longer half-lives are in development, promising improved efficacy and dosing convenience. These innovations aim to broaden therapeutic windows and individualize patient care further, addressing unmet needs in obesity management.
Understanding these advancements requires staying abreast of evolving clinical trial data and mechanistic studies—resources expertly curated in our ongoing updates on advanced Ozempic therapies and combination strategies.
Unraveling Pharmacogenomic Influences on Semaglutide Metabolism and Patient Response Variability
Recent advances in pharmacogenomics illuminate how genetic polymorphisms in drug-metabolizing enzymes and transporters critically modulate semaglutide’s pharmacokinetics and pharmacodynamics. Variants in CYP450 isoenzymes and organic anion-transporting polypeptides (OATPs) can alter systemic exposure to Ozempic, necessitating genotype-informed dosing algorithms to optimize therapeutic windows. These insights empower clinicians to transcend empirical titration, fostering truly individualized regimens that balance maximal adipose tissue reduction with minimized adverse events.
Harnessing Artificial Intelligence and Digital Therapeutics for Dynamic Treatment Optimization
Integrating AI-driven digital health platforms revolutionizes clinical oversight by enabling continuous, granular monitoring of patient adherence, glycemic trends, and behavioral patterns. Machine learning models synthesize multi-parametric data, including activity levels, caloric intake, and biomarker fluctuations, to predict suboptimal responses or emergent gastrointestinal side effects early. This proactive approach facilitates timely intervention adjustments, enhances patient engagement through personalized feedback loops, and ultimately augments fat loss efficacy beyond static treatment paradigms.
What novel biomarkers and digital metrics are proving pivotal in real-time monitoring and prognostication of Ozempic responsiveness?
Cutting-edge research identifies a constellation of biomarkers—circulating fibroblast growth factor 21 (FGF21), adiponectin, inflammatory cytokines, and gut microbiome signatures—that correlate strongly with individual response trajectories to GLP-1 receptor agonists. Concurrently, digital phenotyping through wearable sensors captures behavioral and physiological metrics such as heart rate variability, sleep quality, and glucose excursions. The fusion of these biological and digital data streams fosters predictive analytics frameworks that refine patient stratification and enable dynamic, precision-based treatment modifications. For an exhaustive meta-analysis on these biomarkers, consult the Nature Metabolism publication.
Implementing Integrated Behavioral Interventions to Sustain Long-Term Weight Loss
Pharmacological efficacy of Ozempic synergizes with psychologically informed behavioral strategies targeting reward pathways, craving modulation, and self-efficacy reinforcement. Embedding cognitive-behavioral therapy (CBT) and motivational interviewing within treatment protocols addresses neurobehavioral adaptations that often precipitate weight regain. These integrative approaches reconfigure patient identity and bolster adherence, underpinning durable fat mass reduction and improved metabolic health.
Exploring Emerging Combination Regimens and Next-Generation GLP-1 Analogues
Ongoing clinical trials investigate the synergistic potential of Ozempic co-administered with agents such as SGLT2 inhibitors and amylin mimetics to counteract tachyphylaxis and potentiate lipolytic pathways. Concurrently, novel GLP-1 receptor agonists with enhanced receptor selectivity, prolonged half-lives, and optimized pharmacokinetic profiles promise improved dosing convenience and therapeutic efficacy. These innovations herald a new era in tailored obesity management, expanding the armamentarium against metabolic disorders.
Engage with Expert Insights and Elevate Your Clinical Practice
Delve deeper into these transformative developments by exploring our curated repository of advanced Ozempic therapies and combination strategies at advanced Ozempic therapies and combination strategies. Harness these expert insights to refine your clinical protocols and enhance patient outcomes in the evolving landscape of precision weight loss.
Expert Insights & Advanced Considerations
Precision Dosing: The Pharmacogenomic Frontier
Emerging evidence underscores the critical role of pharmacogenomics in optimizing Ozempic therapy. Genetic polymorphisms affecting CYP450 enzymes and drug transporters can significantly alter semaglutide metabolism, necessitating personalized dosing algorithms. Integrating genotype-informed adjustments promises to enhance fat loss efficacy while minimizing adverse events, moving beyond traditional titration paradigms.
Leveraging AI and Digital Therapeutics for Dynamic Treatment Optimization
Artificial intelligence-powered platforms facilitate continuous, real-time monitoring of metabolic and behavioral metrics during Ozempic therapy. By synthesizing biometric data such as glucose trends, activity levels, and patient-reported outcomes, clinicians can anticipate suboptimal responses and side effects, enabling proactive intervention. This digital integration enhances adherence and amplifies sustainable fat reduction.
Synergistic Combination Therapies to Overcome Tachyphylaxis
Combining Ozempic with agents like SGLT2 inhibitors or amylin analogs is a promising strategy to counteract tachyphylaxis and plateauing weight loss. Such regimens aim to potentiate lipolytic pathways and maintain appetite suppression. Ongoing clinical trials are refining these approaches, foreshadowing a new era of multi-modal pharmacotherapy for obesity management.
Behavioral and Psychological Integration for Long-Term Success
Pharmacological effects of Ozempic are potentiated when paired with cognitive-behavioral therapy (CBT) and motivational interviewing. Addressing neurobehavioral factors such as reward sensitivity and craving modulation is essential for preventing relapse and sustaining fat loss. This biopsychosocial model epitomizes the future of comprehensive weight management.
Emerging Biomarkers and Digital Phenotyping in Personalized Care
Novel biomarkers including fibroblast growth factor 21 (FGF21), adiponectin, inflammatory cytokines, and gut microbiome profiles are proving invaluable for predicting and monitoring Ozempic responsiveness. When combined with digital phenotyping metrics like heart rate variability and sleep patterns, they enable precision medicine approaches that dynamically adapt treatment to individual patient trajectories.
Curated Expert Resources
- Nature Metabolism Meta-Analysis on GLP-1 Biomarkers: Provides comprehensive validation of metabolic and inflammatory markers linked to GLP-1 efficacy, essential for researchers and clinicians aiming to personalize Ozempic dosing (Nature Metabolism).
- NIH Review on GLP-1 Therapeutics in Obesity: An authoritative overview of mechanistic pathways and clinical outcomes associated with semaglutide use in weight management (National Institutes of Health).
- American Heart Association Journal: Offers in-depth analyses on cardiometabolic benefits of Ozempic, providing critical insights beyond weight loss (AHA Journal).
- Advanced Ozempic Therapy Protocols: Detailed clinical guidelines and monitoring strategies for physician-supervised treatments enhancing safety and efficacy (Doctor Supervised Ozempic Treatments Guide).
- Real-World Patient Transformations: Empirical data and patient experiences illustrating typical fat loss trajectories and outcomes (Ozempic Before and After Transformations).
Final Expert Perspective
Decades of research culminate in a nuanced understanding that maximizing Ozempic’s potential for medical weight loss transcends mere pharmacology. The intersection of pharmacogenomics, AI-powered monitoring, combination pharmacotherapy, and integrated behavioral strategies defines the cutting edge of obesity care. These multidimensional approaches not only enhance fat loss efficacy but also address long-term sustainability and patient-centered outcomes. For clinicians and patients committed to evidence-based, precision-guided weight management, engaging deeply with these advanced insights is essential. Explore further expert content such as our comparative analysis on Ozempic vs Wegovy and consider professional consultation pathways outlined in our doctor supervised Ozempic treatments guide to optimize your therapeutic journey.