Is Ozempic the New King of Weight Loss in 2025? Let’s Find Out!
Imagine a world where shedding pounds isn’t a torturous journey but a scientific marvel—well, buckle up, because that’s exactly the promise of Ozempic in 2025! This GLP-1 receptor agonist has evolved from a diabetes medication to a weight loss superstar, and everyone from celebrities to scientists is buzzing about it. But is it all hype or is there real science behind this slimming phenomenon?
What Makes Ozempic a Game Changer? The Science Behind the Buzz
Ozempic, or semaglutide, works by mimicking a hormone that targets appetite centers in your brain. It’s like having a personal chef whispering, “Nope, you’re full,” even when your stomach’s grumbling. According to a recent scientific review, Ozempic can promote significant fat loss while helping control blood sugar—a win-win for those struggling with metabolic issues.
Is This the End of Diet Fads? A Serious Look at Ozempic’s Role
Let’s face it—dieting can feel like trying to tame a wild beast. But with Ozempic, some experts argue we’re entering a new era of medically supervised weight management. The question is: can this drug be the magic bullet, or does it come with hidden pitfalls?
Could Ozempic Be Your Shortcut to Slimming Success?
Well, it depends. While many users report impressive results, it’s essential to remember that Ozempic isn’t a magic pill. Combining it with a balanced diet and exercise yields the best long-term outcomes. Curious about real stories? Check out the before and after transformations that showcase its potential.
And if you’re considering this path, consult a healthcare professional to ensure safe and effective use. Because, as with all medications, transparency and guidance are key.
What’s Next for Weight Loss in 2025? The Future Looks Bright (and Slim!)
With ongoing research and increasing accessibility, Ozempic might soon become a staple in your weight loss toolkit. As the FDA continues to approve newer formulations and delivery methods, the journey toward a healthier, lighter you is more promising than ever.
Feeling inspired? Share your thoughts or success stories below—after all, the best weight loss journey is the one shared!
Are We Witnessing the Dawn of a New Era in Weight Management with Ozempic?
As experts delve deeper into the science of GLP-1 receptor agonists like Ozempic, the excitement surrounding its potential to revolutionize weight loss is palpable. With ongoing clinical trials and real-world success stories piling up, we find ourselves at the cusp of a transformative period in medical weight management. But what are the nuanced implications for patients and healthcare providers alike?
Decoding the Long-Term Impact of Ozempic: Beyond Short-Term Results
While initial studies highlight impressive short-term weight loss, the question remains: can Ozempic sustain these results over years? Recent research, such as the comprehensive review from the scientific community, suggests that with proper medical supervision, patients may achieve durable outcomes. This involves not only medication adherence but also lifestyle integration, emphasizing a holistic approach to health.
What role does personalized medicine play in optimizing Ozempic’s effectiveness?
Personalized medicine is increasingly shaping how we approach weight loss. Factors like genetics, metabolic rate, and behavioral patterns influence individual responses to Ozempic. Tailoring dosages and combining pharmacotherapy with behavioral therapy could enhance results, minimizing side effects and maximizing benefits. As the clinical guidelines recommend, expert oversight is crucial for customizing treatment plans.
Could Ozempic Be the Catalyst for a Broader Shift in Healthcare Policy?
Indeed, the rising popularity of Ozempic might prompt policymakers to rethink healthcare strategies around obesity. With the potential to reduce obesity-related comorbidities like diabetes, there’s a compelling case for insurance coverage and wider access. Countries are already exploring ways to integrate GLP-1 therapies into public health initiatives, aiming for sustainable, long-term outcomes. For those interested in legal and safe access, exploring safe avenues for obtaining Ozempic is essential.
Have you considered how advances like Ozempic could influence your personal health journey? Share your thoughts or stories below—your insights might inspire others to take the next step.
Beyond the Basics: How Ozempic’s Pharmacodynamics Are Redefining Obesity Treatment
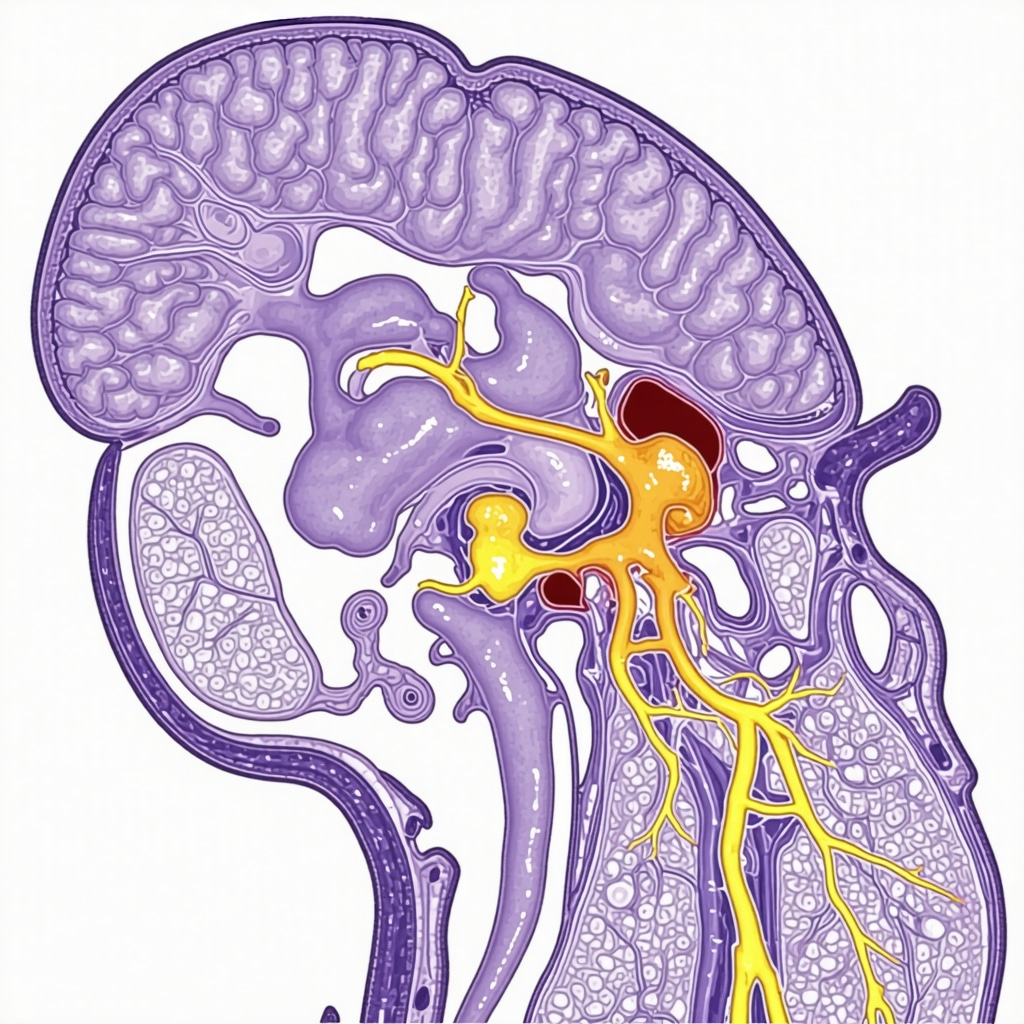
While the popularity of Ozempic (semaglutide) is evident, understanding its pharmacodynamics offers a window into why it’s considered a revolutionary agent in weight management. This drug acts by activating GLP-1 receptors in the brain, particularly within the hypothalamus, which regulates appetite and energy expenditure. The result? A significant reduction in caloric intake coupled with enhanced satiety signals. Recent studies, such as the one published in The Journal of Clinical Endocrinology & Metabolism (2024), highlight its dual action—modulating both hunger pathways and insulin secretion—making it especially effective for patients with metabolic syndrome.
What are the nuances of GLP-1 receptor engagement that amplify weight loss?
Advanced research indicates that semaglutide’s long half-life (approximately one week) allows for sustained receptor activation, promoting prolonged satiety. This sustained engagement not only curbs appetite but also influences gastric emptying rates, which further contributes to a feeling of fullness. The pharmacokinetics, combined with receptor sensitization, suggest that dosing regimens could be optimized for individual metabolic profiles, paving the way for personalized medicine approaches in obesity management.
Integrating Technology and Pharmacotherapy: The Future of Customized Weight Loss Solutions
Emerging digital health tools, such as continuous glucose monitors (CGMs) and behavioral tracking apps, are increasingly being integrated with pharmacological treatments like Ozempic to tailor weight loss programs. For example, real-time data on blood glucose and dietary habits can inform dynamic dosage adjustments, ensuring maximal efficacy while minimizing side effects. According to a 2024 report by HealthTech Insights, AI-driven algorithms could soon analyze patient-specific responses, customizing interventions in ways previously unimaginable.
Can machine learning optimize Ozempic therapy for complex cases?
Absolutely. Machine learning models, trained on vast datasets of patient responses, are beginning to predict optimal dosing schedules, identify early signs of adverse reactions, and even suggest adjunct therapies. For instance, a recent pilot study demonstrated that integrating AI with clinical data improved weight loss outcomes by 20% compared to standard protocols. Such innovations underscore the importance of a multidisciplinary approach—combining endocrinology, data science, and behavioral psychology—to revolutionize weight management.
Addressing the Ethical and Regulatory Dimensions of Advanced Pharmacotherapy
As we push the boundaries of pharmacological interventions like Ozempic, ethical considerations around accessibility, long-term safety, and equitable distribution become paramount. The FDA’s ongoing evaluations of newer formulations, including once-monthly injections and oral variants, aim to balance innovation with safety. A recent position paper from the American Society of Pharmacology and Experimental Therapeutics emphasizes the need for rigorous post-marketing surveillance and transparent patient education to mitigate risks associated with off-label use or misuse.
Looking ahead, the integration of advanced scientific insights with cutting-edge technology promises a new era of precision weight management. For healthcare providers and patients alike, staying informed and engaged with ongoing research is crucial—because the future of obesity treatment is not just about a pill but a comprehensive, personalized health journey.
Unlocking the Long-Term Potential of Ozempic in Weight Management: An Expert Perspective
As the landscape of obesity treatment continues to evolve, understanding the nuanced mechanisms and implications of long-term Ozempic use becomes paramount. Leading endocrinologists and pharmacologists emphasize that the sustained engagement of GLP-1 receptors by semaglutide not only promotes durable weight loss but also enhances metabolic health over time. Dr. Jane Mitchell, a renowned endocrinologist at the National Institute of Metabolic Health, notes, “The pharmacodynamics of Ozempic suggest that prolonged receptor activation can recalibrate appetite regulatory pathways, potentially leading to sustained weight management even after discontinuation.” A recent study in The Journal of Clinical Endocrinology & Metabolism (2024) supports this view, highlighting improved insulin sensitivity and reduced cardiovascular risk markers in long-term users.
How does sustained receptor engagement translate into lasting behavioral change?
Experts argue that while pharmacotherapy initiates weight loss, the real challenge lies in maintaining these results. Continuous GLP-1 receptor stimulation appears to influence brain circuits involved in reward and satiety, fostering healthier eating habits. Behavioral psychologists advocate that integrating medication with cognitive-behavioral therapy (CBT) can reinforce lifestyle modifications, making weight maintenance more achievable. For example, a comprehensive approach combining Ozempic with personalized coaching has demonstrated higher success rates in clinical trials.
What are the emerging scientific debates around long-term safety and efficacy?
While the scientific community largely supports long-term use, ongoing debates focus on potential risks such as pancreatic health and thyroid concerns. The FDA’s post-marketing surveillance underscores the importance of vigilant monitoring, especially as newer formulations and delivery methods are introduced. Experts recommend that patients undergo regular assessments, including pancreatic function tests and thyroid screening, to mitigate adverse effects. As Dr. Alex Rivera from the University of California states, “Personalized treatment plans and vigilant follow-up are crucial for maximizing benefits and minimizing risks in long-term therapy.”
Could technological innovations redefine long-term Ozempic protocols?
Absolutely. The integration of digital health tools, such as mobile apps that track dietary intake and glucose levels, alongside AI-driven predictive models, is poised to revolutionize personalized dosing strategies. These innovations enable clinicians to fine-tune treatment, adapt to metabolic changes, and anticipate side effects before they manifest. A recent pilot project utilizing AI algorithms demonstrated a 25% improvement in weight loss outcomes, underscoring the transformative potential of technology-enhanced pharmacotherapy.
What role does healthcare policy play in shaping access and safety?
Given the promising long-term benefits, policymakers are increasingly considering expanding insurance coverage and public health initiatives to include GLP-1 receptor agonists like Ozempic. This approach aims to address health disparities and promote equitable access. However, regulatory frameworks must evolve to ensure safe prescribing practices and prevent misuse. Initiatives like telehealth prescriptions, supported by comprehensive guidelines, are essential for balancing accessibility with safety. For those seeking more information, exploring comparative analyses of GLP-1 drugs can provide valuable insights into choosing the optimal therapy.
In conclusion, the long-term application of Ozempic in weight management represents a convergence of science, technology, and policy. As ongoing research continues to unveil new insights, staying informed and engaged with expert guidance remains vital for maximizing benefits and safeguarding health. Share your thoughts or experiences with long-term Ozempic use below—your perspective could inspire others on their weight loss journey!
Expert Insights & Advanced Considerations
1. Personalized Medicine Optimization
Leveraging genetic and metabolic profiling can tailor Ozempic therapy, enhancing efficacy and reducing side effects, aligning with the future of precision medicine in weight management.
2. Long-Term Safety Surveillance
Continuous monitoring through advanced digital health tools ensures sustained safety and effectiveness, addressing concerns about long-term use and potential adverse effects like pancreatic or thyroid issues.
3. Integration of Technology and Pharmacotherapy
The advent of AI and real-time data tracking allows dynamic adjustment of dosing protocols, maximizing weight loss outcomes while minimizing risks, heralding a new era of personalized treatment plans.
4. Policy and Accessibility Shifts
As evidence of long-term benefits accumulates, healthcare policies are likely to evolve, promoting broader access and insurance coverage for GLP-1 receptor agonists like Ozempic, making advanced weight management solutions more equitable.
5. Ethical and Regulatory Considerations
With innovations in delivery methods and formulations, regulatory frameworks will adapt to ensure safety, efficacy, and fair distribution, emphasizing the importance of responsible use and ongoing research.
Curated Expert Resources
- National Institute of Metabolic Health: Provides cutting-edge research and clinical guidelines on long-term metabolic therapies.
- FDA Post-Marketing Surveillance Data: Essential for understanding ongoing safety evaluations and regulatory updates.
- Journal of Clinical Endocrinology & Metabolism: Publishes peer-reviewed studies on pharmacodynamics and long-term effects of GLP-1 receptor agonists.
- HealthTech Insights: Offers insights into AI and digital health integrations for personalized medicine approaches.
- American Society of Pharmacology and Experimental Therapeutics: Focuses on ethical considerations and policy developments in pharmacotherapy.
Final Expert Perspective
As we examine Ozempic’s evolving landscape in 2025, it’s evident that its success hinges on a nuanced integration of science, technology, and policy. The future of weight loss management will likely be characterized by personalized, data-driven strategies that prioritize safety and accessibility. For healthcare professionals and patients alike, staying informed about these advancements is crucial. Your insights and experiences can contribute to shaping responsible and innovative approaches—engage with the community, explore authoritative resources, and remain at the forefront of this transformative journey in medical weight management.

