Revolutionizing Weight Loss: The Rise of Prescription Options
In the evolving landscape of weight management, prescription medications have emerged as powerful allies. Among them, Ozempic stands out, not just as a diabetes medication but increasingly recognized for its remarkable impact on weight loss. This shift invites a closer examination of how Ozempic fits into the broader array of prescription weight loss options and what makes it a preferred choice for many patients and clinicians alike.
Decoding Ozempic: More Than Just a Diabetes Drug
Ozempic, or semaglutide, is a glucagon-like peptide-1 (GLP-1) receptor agonist originally designed to improve glycemic control in type 2 diabetes. However, its ability to promote satiety and reduce appetite has led to its adoption in medical weight loss programs. Unlike traditional weight loss drugs that primarily focus on metabolic rate or fat absorption, Ozempic works by mimicking gut hormones that regulate hunger, offering a nuanced approach to appetite management.
How Does Ozempic Compare to Other Weight Loss Prescriptions?
When contrasting Ozempic with other FDA-approved weight loss medications such as phentermine or orlistat, several distinctions emerge. One critical advantage is its dual effect on blood sugar control and weight reduction, making it particularly beneficial for patients with comorbid conditions like diabetes or prediabetes. Furthermore, clinical trials have demonstrated significant and sustained weight loss with Ozempic, often exceeding 10% of body weight over several months, which is notable compared to other therapies.
What Should Patients Know Before Starting Ozempic for Weight Loss?
Embarking on a weight loss journey with Ozempic requires informed medical supervision. Side effects such as nausea, gastrointestinal discomfort, or potential rare risks like pancreatitis necessitate thorough discussion with healthcare providers. Additionally, dosage titration and lifestyle modifications complement the medication’s effectiveness, emphasizing that Ozempic is part of a comprehensive treatment plan rather than a standalone solution.
Expert Insights: Integrating Ozempic into Personalized Weight Management Plans
Clinicians today are tailoring weight loss protocols to individual patient profiles, where Ozempic plays a strategic role. Case scenarios reveal that patients combining Ozempic with structured dietary adjustments and physical activity experience more sustainable outcomes. The drug’s mechanism, targeting appetite regulation centrally and peripherally, aligns well with behavioral interventions, enhancing adherence and long-term success.
How Does Ozempic Fit Into the Future of Prescription Weight Loss?
As research progresses, Ozempic is anticipated to maintain a central role in weight management, especially with emerging evidence supporting its efficacy in diverse populations and longer-term safety. Its integration into telehealth models has further broadened access, allowing more patients to benefit under physician supervision. For those seeking comprehensive insights, resources like the detailed exploration of Ozempic’s role in prescription weight loss offer invaluable guidance.
Ready to explore how Ozempic could transform your weight loss strategy? Connect with expert providers today and discover personalized programs designed to maximize your health outcomes.
For authoritative, peer-reviewed information on semaglutide’s effectiveness and safety, the New England Journal of Medicine’s landmark STEP trials provide comprehensive clinical evidence supporting its use in weight management.
My Journey With Ozempic: Embracing a New Chapter in Weight Management
After reading extensively and consulting with my healthcare provider, I decided to try Ozempic as part of my weight loss journey. The initial weeks were a learning curve—as my body adjusted, I experienced mild nausea, which my doctor had prepared me for. What surprised me most was how my appetite changed; the cravings that once dictated my snacking habits began to fade. This shift wasn’t just physical but emotional too, as I regained a sense of control over my eating patterns.
How Can We Stay Motivated When Weight Loss Plateaus Occur?
This question is one I often ask myself during my journey. Weight loss isn’t linear, and there will be moments when the scale stalls. What helped me was focusing on non-scale victories—improved energy levels, better sleep, and the simple joy of fitting comfortably into clothes I hadn’t worn in years. Celebrating these milestones keeps the motivation alive, even when progress seems slow. It’s also crucial to communicate openly with your healthcare provider during these times to adjust your plan if needed.
Personalizing Your Ozempic Experience: Beyond the Medication
One key realization is that Ozempic is most effective when combined with lifestyle changes. For me, this meant adopting a balanced diet rich in whole foods and incorporating regular physical activity tailored to my preferences. I found that even light exercise, like daily walks, amplified the medication’s benefits and improved my mood. It’s about crafting a sustainable routine that fits your life rather than forcing drastic changes.
Interestingly, a review published by the Mayo Clinic highlights that combining GLP-1 receptor agonists like Ozempic with behavioral interventions significantly enhances weight loss outcomes. This reinforces the importance of a holistic approach rather than relying solely on medication.
Finding Trusted Medical Support for Your Ozempic Journey
Trust and expertise are paramount when navigating prescription weight loss options. I recommend seeking out medical weight loss clinics that offer doctor-supervised Ozempic treatments. These programs provide tailored dosage adjustments and ongoing monitoring, ensuring safety and maximizing results. Avoid the pitfalls of unverified online sources and always prioritize your health by consulting licensed providers.
If you’re curious about real-life transformations, exploring Ozempic before and after stories can offer inspiration and realistic expectations.
Have You Experienced or Considered Using Prescription Weight Loss Medications Like Ozempic?
Weight loss journeys are deeply personal, and each path is unique. If you’ve tried Ozempic or other prescription options, I’d love to hear about your experiences and insights. Sharing our stories can create a supportive community where we learn from each other. Feel free to leave a comment below or connect through related discussions on expert weight loss forums.
Harnessing Pharmacogenomics: Tailoring Ozempic Therapy to Genetic Profiles
Recent advances in pharmacogenomics have opened a frontier in personalized medicine, presenting opportunities to optimize Ozempic efficacy by aligning treatment with an individual’s genetic makeup. Variations in genes encoding GLP-1 receptors, metabolic enzymes, and appetite-regulating pathways can influence response to semaglutide, potentially explaining interpatient variability in weight loss outcomes. Integrating genetic screening into clinical protocols might allow for refined patient selection and dosage customization, minimizing adverse effects and maximizing therapeutic benefit.
Such an approach requires collaboration across specialties, involving endocrinologists, geneticists, and clinical pharmacologists to interpret genomic data and translate it into actionable treatment plans. Although still in its nascent stages, this precision medicine paradigm represents a cutting-edge evolution beyond the traditional ‘one-size-fits-all’ prescribing model.
Optimizing Behavioral Synergies: Neurocognitive Mechanisms Underpinning Appetite Regulation with Ozempic
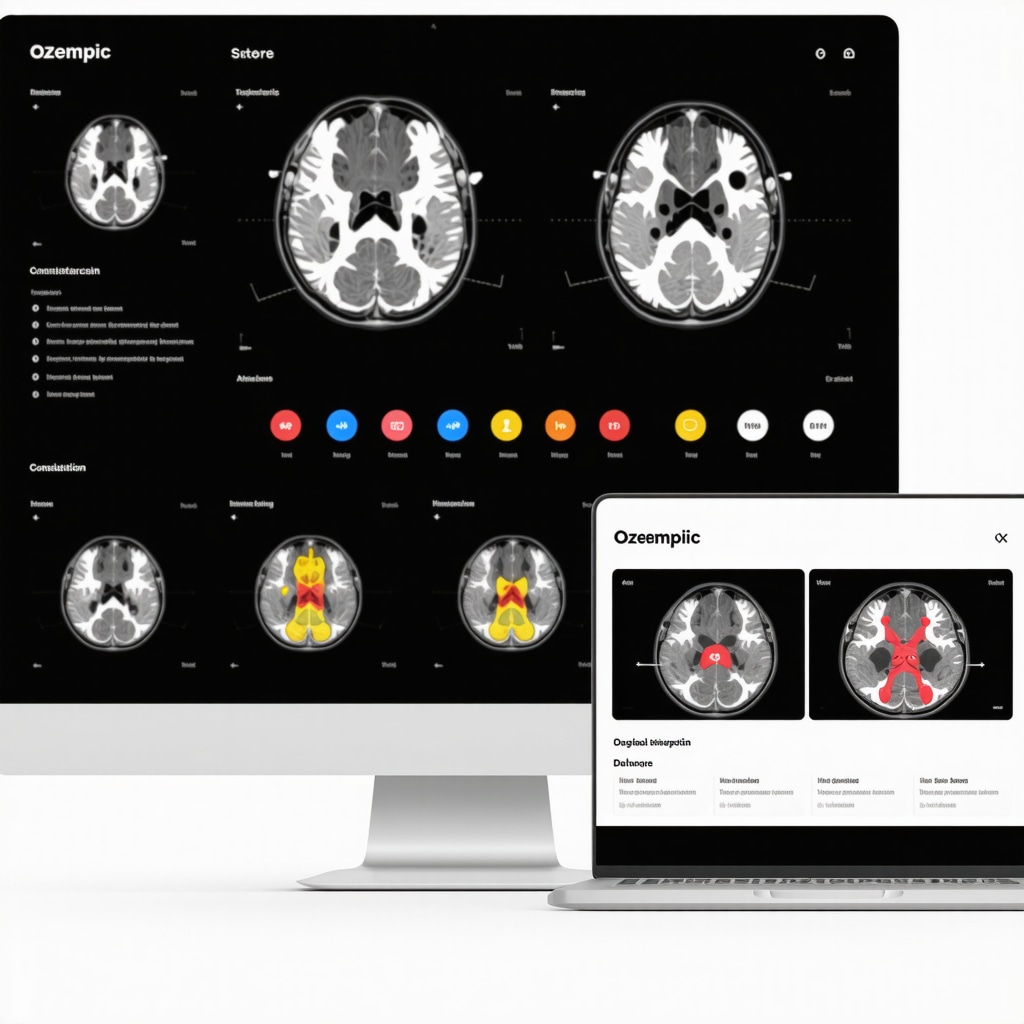
Ozempic’s appetite-suppressing effects are not solely peripheral but also involve central nervous system pathways. Neuroimaging studies reveal that semaglutide modulates activity within the hypothalamus and reward-related circuits, attenuating the hedonic drive to consume calorie-dense foods. Understanding these neurocognitive mechanisms enables clinicians to design complementary behavioral interventions that reinforce medication effects.
For instance, cognitive-behavioral therapy (CBT) focusing on impulse control and mindful eating can synergize with Ozempic-induced satiety signals, fostering sustainable dietary habits. Additionally, emerging evidence suggests that tailoring meal timing and macronutrient composition to circadian rhythms may enhance GLP-1 receptor agonist effectiveness, a frontier warranting further exploration.
What Are the Long-Term Cardiometabolic Benefits of Ozempic Beyond Weight Loss?
Beyond its established role in weight reduction, Ozempic demonstrates significant cardiometabolic advantages. The landmark SUSTAIN and STEP trials documented improvements in blood pressure, lipid profiles, and inflammatory markers, translating into reduced cardiovascular event risk in high-risk populations. These multifaceted benefits position Ozempic as a valuable agent in managing obesity-related comorbidities, especially in patients with type 2 diabetes or metabolic syndrome.
However, sustained benefits require adherence and ongoing monitoring. Clinicians should integrate regular cardiovascular assessments and metabolic panel evaluations into long-term management plans to optimize outcomes and promptly address emerging concerns.
Bridging Access Gaps: Telemedicine and Digital Health Innovations for Ozempic Management
Telehealth platforms have revolutionized access to specialist care, particularly for prescription weight loss therapies like Ozempic. Remote monitoring technologies, including continuous glucose monitors and digital adherence trackers, enable real-time data sharing, facilitating proactive dose adjustments and side effect management.
Moreover, digital health applications incorporating AI-driven coaching and behavioral nudges enhance patient engagement, supporting lifestyle modifications alongside pharmacotherapy. Such integrative models not only improve clinical outcomes but also reduce healthcare disparities by reaching underserved or geographically isolated populations.
For clinicians and patients interested in leveraging these innovations, resources such as the American Heart Association’s review on telemedicine in cardiometabolic care provide valuable guidance on implementation and best practices.
Curious about how personalized pharmacogenomic insights or digital tools can enhance your Ozempic experience? Consult with our expert team to discover tailored approaches that align with your unique health profile and lifestyle.
Precision Medicine Meets Weight Loss: The Pharmacogenomic Frontier with Ozempic
Delving deeper into the nuances of Ozempic therapy, pharmacogenomics offers a transformative lens through which clinicians can tailor treatment regimens. Genetic polymorphisms in GLP-1 receptor genes and metabolizing enzymes modulate semaglutide’s pharmacodynamics and pharmacokinetics, explaining why some patients exhibit robust weight loss responses while others encounter diminished effects or side effects. Integrating comprehensive genomic profiling into clinical workflows promises to refine patient stratification, optimize dosing strategies, and reduce adverse event incidence, heralding a new era of personalized obesity management.
How Can Genomic Variability Influence Patient Response to Ozempic?
Genomic variability profoundly impacts receptor sensitivity and drug metabolism. For example, single nucleotide polymorphisms (SNPs) in the GLP1R gene may alter receptor conformation, influencing semaglutide binding affinity and downstream signaling efficacy. Additionally, variants in cytochrome P450 enzymes affect drug clearance rates, necessitating individualized dose adjustments. Understanding these genetic determinants allows clinicians to anticipate therapeutic outcomes and tailor interventions accordingly, minimizing trial-and-error approaches.
Unraveling the Neurocognitive Mechanisms: Enhancing Ozempic’s Appetite Regulation
Beyond peripheral hormonal effects, Ozempic exerts profound influence on central neural circuits governing hunger and reward. Functional MRI studies illuminate its capacity to downregulate activity within the hypothalamus and mesolimbic pathways, attenuating the motivational salience of high-calorie stimuli. This neurocognitive modulation synergizes with behavioral therapies—such as cognitive-behavioral therapy (CBT) and mindful eating—to solidify sustainable eating habits. Emerging research also suggests that aligning meal timing with circadian biology can potentiate GLP-1 receptor agonists’ effects, offering a novel chronotherapeutic dimension.
Transforming Access and Adherence: Telemedicine’s Role in Ozempic Management
The integration of telehealth and digital health innovations is revolutionizing how patients initiate and maintain Ozempic therapy. Remote monitoring tools, including continuous glucose monitoring (CGM) and digital adherence platforms, facilitate real-time data sharing between patients and providers, enabling timely dose titration and side effect mitigation. Artificial intelligence-driven behavioral coaching apps complement pharmacotherapy by reinforcing lifestyle modifications and promoting engagement. Importantly, these advances bridge geographic and socioeconomic barriers, democratizing access to expert care.
For a comprehensive exploration of telemedicine’s impact on cardiometabolic management, the American Heart Association’s review provides an invaluable resource grounded in current evidence and best practices.
Curious to elevate your Ozempic journey with cutting-edge pharmacogenomic insights and digital health solutions? Engage with our specialized clinical team today to craft a truly personalized weight management plan that integrates the latest advances for optimal outcomes.
Frequently Asked Questions (FAQ)
What is Ozempic and how does it aid in weight loss?
Ozempic is a brand name for semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist originally developed for type 2 diabetes management. It aids weight loss by mimicking gut hormones that regulate appetite, increasing feelings of fullness and reducing hunger, which helps decrease caloric intake.
How does Ozempic differ from other prescription weight loss medications?
Unlike traditional weight loss drugs that focus on metabolism or fat absorption, Ozempic centrally modulates appetite through neurocognitive pathways and peripherally slows gastric emptying. Its dual benefits include glycemic control and significant, sustained weight reduction, making it especially useful for patients with diabetes or metabolic syndrome.
What are common side effects of Ozempic and how should patients manage them?
Common side effects include nausea, gastrointestinal discomfort, and occasional vomiting, typically occurring during dose escalation. Patients should follow gradual titration schedules, maintain hydration, and report severe or persistent symptoms to their healthcare provider to ensure safety.
Can Ozempic be used as a standalone weight loss solution?
Ozempic is most effective when integrated into a comprehensive weight management plan that includes dietary modifications, physical activity, and behavioral therapies. Relying solely on medication without lifestyle changes may limit long-term success.
How does pharmacogenomics affect the response to Ozempic?
Genetic variations in GLP-1 receptor genes and drug-metabolizing enzymes can influence individual responses to Ozempic, impacting efficacy and side effect profiles. Pharmacogenomic profiling may enable personalized dosing and improved therapeutic outcomes in the future.
What neurocognitive mechanisms are involved in Ozempic’s appetite regulation?
Ozempic modulates brain regions such as the hypothalamus and reward circuits, reducing the hedonic drive for calorie-dense foods. This central effect complements peripheral satiety signals and can be enhanced by behavioral interventions like cognitive-behavioral therapy.
Are there long-term cardiometabolic benefits of using Ozempic?
Yes, beyond weight loss, Ozempic has demonstrated improvements in blood pressure, lipid profiles, and inflammatory markers, contributing to reduced cardiovascular risk particularly in patients with type 2 diabetes or metabolic syndrome.
How has telemedicine influenced Ozempic treatment and adherence?
Telehealth platforms enable remote monitoring, timely dose adjustments, and digital behavioral support, enhancing patient engagement and access to expert care, especially for those in underserved or remote areas.
Who should consider Ozempic for weight management?
Patients with obesity, especially those with comorbid type 2 diabetes or prediabetes, may benefit from Ozempic under medical supervision. However, candidacy should be determined through thorough clinical evaluation and personalized assessment.
Where can I find reliable medical support for Ozempic therapy?
Seek licensed medical weight loss clinics offering doctor-supervised Ozempic programs to ensure safety, tailored dosing, and comprehensive monitoring. Avoid unverified online sources to protect your health.
Trusted External Sources
- New England Journal of Medicine (NEJM): The STEP clinical trials published here provide robust, peer-reviewed evidence on semaglutide’s efficacy and safety in weight management.
- Mayo Clinic: Offers authoritative reviews on GLP-1 receptor agonists and their integration with behavioral therapies, supporting holistic treatment approaches.
- American Heart Association (AHA): Their comprehensive review on telemedicine in cardiometabolic care informs best practices for remote management of therapies like Ozempic.
- Clinical Pharmacogenomics Research Consortium: Provides insights into genetic factors influencing drug response, relevant for precision medicine applications with Ozempic.
- Journal of Neuroendocrinology: Features studies on neurocognitive mechanisms of appetite regulation that underpin pharmacologic effects of GLP-1 receptor agonists.
Conclusion
Ozempic represents a paradigm shift in prescription weight loss therapies by combining effective glycemic control with potent appetite regulation through both peripheral and central mechanisms. Its integration into personalized treatment plans, supported by emerging pharmacogenomic insights and digital health innovations, enhances efficacy and patient adherence. While side effects and appropriate medical supervision remain critical considerations, the broad cardiometabolic benefits extend its value beyond mere weight reduction. Embracing a comprehensive, multidisciplinary approach that includes lifestyle adjustments and behavioral support maximizes the transformative potential of Ozempic in weight management. We encourage readers to engage with healthcare professionals, explore credible resources, and share their experiences to foster a knowledgeable and supportive community. Discover how the latest advances in prescription weight loss can empower your journey toward sustained health and vitality.

