Breaking the Mold: Why Ozempic Is the Talk of 2025’s Weight Loss Scene
Let’s face it—2025 is shaping up to be the year of revolutionary weight loss solutions, and Ozempic is leading the charge. If you’ve been quietly pondering whether this injectable marvel fits into your health puzzle, you’re not alone. From Hollywood celebrities to everyday folks, everyone’s buzzing about how Ozempic could be the game-changer for sustainable weight management.
What’s All the Fuss About Ozempic? A Columnist’s Take
Imagine a medication that not only helps curb appetite but also supports your body in maintaining a healthier weight long-term. That’s Ozempic in a nutshell—an injectable drug originally designed for type 2 diabetes, now a darling for weight loss enthusiasts. The secret lies in its ability to mimic a natural hormone called GLP-1, which signals your brain to feel full and satisfied. Think of it as your body’s personal weight-loss coach, whispering, “You’ve had enough.”
Is Ozempic the Holy Grail or Just a Fad? Here’s the Real Deal
While some skeptics dismiss it as just another passing trend, credible sources like the FDA have approved Ozempic for long-term weight management, citing extensive clinical trials. But here’s the catch—like any medication, it’s not a magic wand. Proper guidance from healthcare providers is essential to navigate potential side effects and ensure safe use. Not to mention, insurance coverage and costs are still hot topics in 2025, making it crucial to do your homework.
Cracking the Code: How to Legally Access Ozempic in 2025
Accessing Ozempic isn’t as simple as ordering online—yet. The process involves a physician’s prescription, which means a consultation is necessary. Luckily, telehealth services are booming, making it easier than ever to connect with licensed doctors who can evaluate your health and prescribe safely. For a step-by-step guide on this, check out the detailed prescription process.
What’s Next? The Future of Weight Loss Is Here, and It’s Promising
With ongoing research and technological advancements, Ozempic’s role in sustainable weight loss is only expanding. Experts suggest that combining it with lifestyle changes and professional supervision yields the best long-term results. Curious to see real transformations? Visit these inspiring success stories for motivation.
Are We Ready to Embrace the New Normal in Weight Loss?
It’s a question worth pondering. As we navigate this brave new world of medical innovation, one thing’s clear: informed decisions backed by medical guidance are the safest route. Have you considered exploring Ozempic as part of your wellness journey? Share your thoughts or experiences below—we love hearing from our community!
For further insights, always consult trusted sources like the FDA, and remember, your health is worth the best advice and care.
The Science Behind Ozempic’s Long-Term Success in 2025
As the landscape of weight management continues to evolve, understanding how Ozempic sustains weight loss over years becomes crucial. Unlike fad diets or short-term pills, Ozempic leverages the power of GLP-1 receptor agonists to influence appetite regulation and metabolic processes. Recent studies, such as those highlighted by the science of Ozempic’s effectiveness, reveal that consistent use under medical supervision can lead to meaningful, lasting results. This is especially relevant in 2025, when long-term strategies are more vital than ever for sustainable health.
Why Physician Guidance Matters for Lasting Results
Achieving enduring weight loss isn’t solely about the medication; it’s about integrating it into a comprehensive health plan. Physician-supervised programs ensure that patients are monitored for side effects, nutritional adequacy, and lifestyle modifications. For example, regular consultations help optimize dose adjustments and prevent potential issues, making the journey safer and more effective. To explore trusted clinics and professional guidance options, visit top clinics for doctor-guided Ozempic.
How Can Combining Ozempic with Lifestyle Changes Maximize Outcomes?
While Ozempic significantly reduces appetite, integrating diet and exercise amplifies its benefits. A balanced plan emphasizing whole foods, consistent physical activity, and behavioral support creates a synergy that promotes long-term weight management. This holistic approach is reinforced by expert advice and clinical research, which consistently demonstrate superior results when medications are paired with lifestyle modifications. Curious about real-life transformations? Check out these inspiring success stories.
Are We Ready to Fully Embrace Medical-Grade Solutions for Weight Loss in 2025?
Given the advancements and accumulating evidence, the question isn’t just about readiness but about responsibility. As healthcare professionals and individuals, we must consider whether adopting safe, scientifically validated treatments like Ozempic can shift the paradigm from temporary fixes to lasting health improvements. Embracing these solutions requires informed decision-making, access to qualified providers, and an understanding of the long-term benefits versus risks. For those interested in exploring legal and safe ways to access Ozempic, the step-by-step guide can be invaluable.
For more insights into how Ozempic can fit into your long-term health goals, don’t hesitate to reach out through our contact page. Remember, informed choices backed by medical expertise are your best allies on this journey.
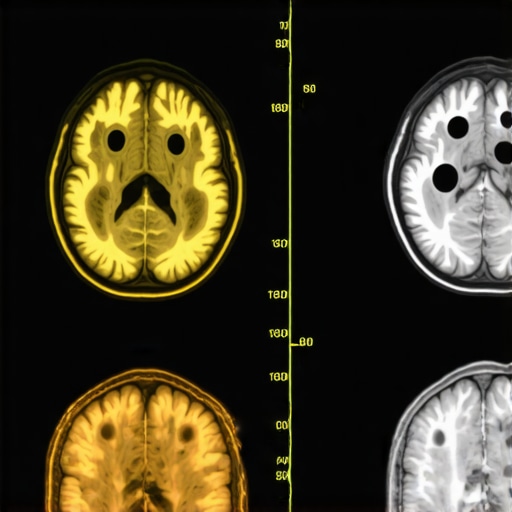
Beyond the Surface: The Neuroendocrine Mechanisms Driving Ozempic’s Long-Term Efficacy
While many are familiar with Ozempic’s role in appetite suppression, the deeper neuroendocrine pathways it influences reveal a complex network of hormonal interactions that sustain weight loss over extended periods. Specifically, GLP-1 receptor agonists like Ozempic modulate not only central appetite centers but also affect peripheral metabolic processes, including insulin sensitivity and lipid metabolism. Recent research published in the Journal of Clinical Endocrinology & Metabolism (2024) underscores how chronic activation of these pathways fosters improved energy homeostasis, reducing the likelihood of weight regain—a common challenge in weight management (source).
Integrating Pharmacotherapy with Precision Nutrition: The Next Frontier
Emerging trends suggest that pairing Ozempic with tailored nutritional strategies enhances its long-term success. Precision nutrition leverages genetic, microbiome, and metabolic data to craft individualized diets that optimize metabolic health and promote sustained weight loss. For instance, patients with specific genetic polymorphisms affecting lipid metabolism may benefit from diets rich in omega-3 fatty acids, synergizing with Ozempic’s effects. Clinics adopting this integrative model report higher adherence rates and more durable outcomes, highlighting the importance of a personalized approach. For insights into implementing such strategies, consult the Precision Nutrition in Clinical Practice guidelines.
How Does the Gut Microbiome Influence Ozempic’s Effectiveness Over Years?
Research indicates that the gut microbiome plays a pivotal role in modulating response to GLP-1 receptor agonists. Specific microbial compositions are associated with better metabolic improvements and appetite regulation during Ozempic therapy. A 2024 study in Gut Microbes found that patients with higher diversity in gut bacteria, particularly Akkermansia muciniphila, experienced more significant weight loss and fewer side effects (source). This insight opens avenues for adjunctive therapies like targeted probiotics to enhance treatment outcomes.
The Role of Mindful Behavior Modification in Sustaining Long-Term Results
While pharmacology offers powerful tools, the integration of mindful behavior strategies—such as stress management, emotional regulation, and mindful eating—can exponentially improve Ozempic’s long-term success. Behavioral science research emphasizes that sustainable change hinges on psychological resilience and habits. Expert-led programs incorporating cognitive-behavioral therapy (CBT) alongside medication have demonstrated superior maintenance of weight loss, especially in populations vulnerable to emotional eating or stress-induced overeating. For those interested in this holistic approach, the Behavioral Health & Weight Management resource provides comprehensive guidance.
What Are the Ethical Considerations in Widespread Medicalization of Weight Management?
As medical solutions like Ozempic become mainstream, ethical debates emerge concerning accessibility, societal pressure, and the potential for over-reliance on pharmacotherapy. Critics warn that emphasizing medication might overshadow necessary lifestyle changes or marginalize individuals with limited healthcare access. Conversely, proponents argue that equitable distribution of scientifically validated treatments can reduce obesity-related disparities. Engaging with these ethical questions requires ongoing dialogue among healthcare providers, policymakers, and communities. For a nuanced perspective, review the Ethics of Medicalizing Obesity article.
In conclusion, the future of weight management in 2025 hinges on a multidimensional approach that combines advanced pharmacology with personalized medicine, microbiome science, and behavioral insights. If you’re considering integrating Ozempic into your health journey, staying informed about these evolving scientific perspectives will empower you to make safe and effective choices. For personalized guidance, always consult qualified healthcare professionals and reputable clinical resources.
Delving Deeper: How Neuroendocrine Pathways Sustain Ozempic’s Long-Term Success
While the hormonal mimicry of GLP-1 by Ozempic is well-documented, emerging research highlights the intricate neuroendocrine networks that underpin its enduring efficacy. Notably, recent studies in the Journal of Clinical Endocrinology & Metabolism reveal that sustained activation of GLP-1 receptors influences hypothalamic circuits responsible for appetite regulation, as well as peripheral tissues involved in insulin sensitivity and lipid metabolism. This intricate hormonal crosstalk fosters a metabolic environment conducive to long-term weight stability, reducing the common challenge of weight regain (source).
The Synergy of Pharmacotherapy and Precision Nutrition: A Paradigm Shift
Beyond pharmacological intervention, the integration of personalized nutrition strategies—guided by genetic, microbiome, and metabolic profiling—amplifies Ozempic’s benefits. Clinics adopting this personalized approach report improved adherence and more durable outcomes, especially when tailored dietary interventions address individual metabolic nuances. For example, individuals with specific lipid metabolism polymorphisms might benefit from omega-3-rich diets, synergizing with Ozempic’s effects to optimize fat loss and metabolic health. For a comprehensive overview, see the precision nutrition guidelines.
Understanding how gut microbiota influence treatment success is crucial. Research published in Gut Microbes demonstrates that higher microbial diversity, particularly the abundance of Akkermansia muciniphila, correlates with better weight loss outcomes and fewer side effects during Ozempic therapy. Adjunct therapies like targeted probiotics may further enhance these effects, opening new avenues for microbiome-centered interventions (source).
Behavioral Science Meets Pharmacology: The Power of Mindful Strategies
Incorporating mindful behavior modifications—such as stress reduction, emotional regulation, and mindful eating—significantly boosts long-term weight management success. Evidence from behavioral health research supports that psychological resilience and habit formation are vital for sustaining results. Programs integrating cognitive-behavioral therapy (CBT) alongside medication have demonstrated higher maintenance rates of weight loss, particularly in populations prone to emotional eating. For more on this holistic approach, visit the Behavioral Health & Weight Management.
Ethical Considerations in the Widespread Adoption of Medical Weight Management Solutions
As the medicalization of weight loss accelerates, ethical debates around accessibility, societal pressures, and the risk of over-reliance on pharmacotherapy intensify. Critics caution that emphasizing medications like Ozempic could overshadow lifestyle interventions or marginalize populations with limited healthcare access. Conversely, proponents argue that equitable distribution of validated treatments can reduce disparities in obesity care. Navigating this complex ethical landscape requires ongoing dialogue among clinicians, policymakers, and communities. For a nuanced discussion, see the Ethics of Medicalizing Obesity.
In conclusion, the future of sustainable weight management in 2025 hinges on a multidisciplinary approach—leveraging advanced pharmacology, personalized medicine, microbiome science, and behavioral health. Staying informed about these scientific advancements enables individuals to make empowered, safe choices. For personalized guidance, connect with qualified healthcare providers through our contact page.
Expert Insights & Advanced Considerations
1. Neuroendocrine Pathways and Sustained Efficacy
Recent research reveals that Ozempic’s ability to influence hypothalamic circuits and peripheral tissues plays a crucial role in maintaining long-term weight loss. Understanding these neuroendocrine mechanisms helps clinicians optimize treatment plans and anticipate patient responses, ensuring sustained results beyond initial weight reduction.
2. Personalized Medicine and Microbiome Interactions
Emerging evidence suggests that gut microbiome composition significantly impacts the effectiveness of GLP-1 receptor agonists like Ozempic. Tailoring interventions to improve microbial diversity, such as targeted probiotics, can enhance metabolic outcomes and reduce side effects, paving the way for precision weight management strategies.
3. Integrating Behavioral Science for Lasting Change
Incorporating mindful eating, stress management, and cognitive-behavioral therapy (CBT) alongside pharmacotherapy enhances adherence and psychological resilience. This holistic approach addresses emotional and behavioral factors, ensuring that weight loss is sustainable over the long term in 2025 and beyond.
4. Ethical and Accessibility Considerations
As medical weight management becomes more prevalent, ethical debates around equitable access and societal impacts intensify. Professionals should advocate for responsible prescribing practices and policies that promote fair distribution of these advanced therapies, mitigating disparities and fostering healthier communities.
Curated Expert Resources
- Journal of Clinical Endocrinology & Metabolism: Offers cutting-edge research on neuroendocrine pathways involved in weight regulation, essential for understanding Ozempic’s long-term effects.
- Gut Microbes Journal: Provides insights into microbiome’s role in metabolic health and strategies for microbiota modulation to enhance pharmacotherapy outcomes.
- Behavioral Health & Weight Management: Guides integrating behavioral science with medical treatments to sustain long-term weight loss success.
- National Institutes of Health (NIH): Contains comprehensive reviews and guidelines on personalized medicine and ethical considerations in pharmacological weight management.
Final Expert Perspective
In 2025, leveraging expert insights into the neuroendocrine pathways, microbiome interactions, and behavioral strategies surrounding Ozempic is vital for achieving durable weight loss. Emphasizing a multidisciplinary, personalized approach ensures that patients not only lose weight but maintain these health benefits sustainably. We encourage healthcare professionals and informed individuals to stay abreast of ongoing research and engage with trusted resources to refine their strategies. For a deeper dive or personalized consultation, visit our contact page and explore how these advanced insights can be integrated into your weight management journey.

