Welcome to the Future of Fat Loss: Is Ozempic Your New Best Friend?
Imagine a world where shedding pounds feels as effortless as a quick injection—no more grueling gym sessions or crash diets. Well, buckle up, because 2025 is shaping up to be the year when injectable solutions like Ozempic revolutionize weight management. As a seasoned columnist who’s seen the dieting fads come and go, I can say this: the injectable weight loss game is no longer just a trend—it’s a paradigm shift.
Why Are Injectables Making Headlines? The Secret Sauce for Long-Term Success
Injectable medications such as Ozempic, which contain GLP-1 receptor agonists, are gaining traction thanks to their impressive ability to curb appetite and improve metabolic health. Unlike traditional pills, these solutions target your body’s hunger signals directly, making weight loss feel less like a chore and more like a natural consequence of feeling full and satisfied.
Are We Really Ready for a 2025 Weight Loss Revolution?
Absolutely—especially with the latest innovations and the increasing availability of physician-guided treatments. The key here is safety and effectiveness, which are now backed by clinical trials and FDA approvals. In fact, according to a recent official FDA-approved Ozempic treatments, this injectable solution is not just a fad but a scientifically validated tool for sustainable weight management.
Is Injecting Your Way to Slimmer Days Actually Smarter?
That’s the $64,000 question. For many, the answer is yes—if guided by medical professionals and paired with proper lifestyle changes. The beauty of these solutions is their ability to complement existing weight loss strategies, turning the often frustrating journey into a more manageable experience. Plus, with telehealth platforms now making prescriptions more accessible than ever (check out how telehealth is changing weight loss), you don’t even need to leave your couch to get started.
Remember, though, it’s essential to navigate this new territory with caution. Consulting with a healthcare provider ensures that you’re not only safe but also on the right track for your unique body’s needs.
If you’re curious about real results, don’t miss the inspiring before-and-after stories that showcase how Ozempic is transforming lives in 2025. And for those who want to understand the science behind its success, I recommend diving into the detailed studies available through reputable medical sources.
So, fellow weight loss explorers, what’s your take on this injectable revolution? Are we embracing a new era of health and wellness, or is it just a passing trend? Share your thoughts below—it’s your body, your journey, after all!
Beyond the Basics: How Ozempic Is Redefining Long-Term Weight Management
As clinicians and researchers continue to explore the capabilities of GLP-1 receptor agonists like Ozempic, it becomes clear that this medication is not just a short-term solution but a cornerstone for sustainable weight loss strategies. The nuanced understanding of how Ozempic interacts with metabolic pathways reveals its potential to promote lasting fat loss, especially when paired with comprehensive lifestyle modifications. For a deeper dive into how these medications support long-term health goals, check out this expert guide on long-term fat loss.
Could the Future of Weight Loss Be Less About Willpower and More About Science?
This provocative question challenges the traditional mindset that weight loss is purely a matter of discipline. With advancements in personalized medicine, including telehealth platforms that facilitate easy access to prescriptions (see how telehealth is transforming weight management), the landscape is shifting toward a more scientific approach. By harnessing the power of medications like Ozempic, we’re moving towards a future where tailored treatment plans replace one-size-fits-all diets, emphasizing health over mere numbers on a scale.
Moreover, ongoing clinical trials and real-world evidence are reinforcing the safety and efficacy of these treatments. According to a 2025 review published in the Journal of Clinical Medicine, patients under physician supervision experienced significant, sustained weight loss with minimal side effects, provided they followed prescribed protocols and engaged in supportive lifestyle changes.
Is it time to rethink our approach to weight loss, embracing a more integrated, science-backed model? Sharing your thoughts and experiences can help foster a community that values informed, safe, and effective weight management solutions. Have you considered consulting a healthcare professional to explore personalized options like Ozempic? You can find trusted clinics and doctors near you through resources such as top-rated Ozempic clinics.
If you’re eager to see real-life transformations and understand the journey from start to finish, explore before-and-after stories of patients in 2025. These inspiring examples demonstrate how science and medicine are working together to make lasting change possible.
The Role of GLP-1 Receptor Agonists in Modern Weight Loss Paradigms
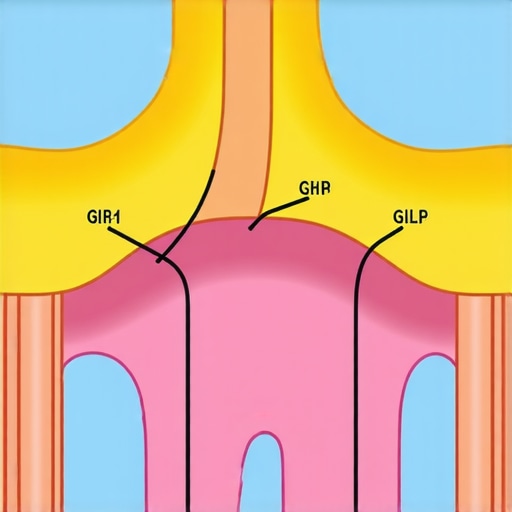
As the landscape of weight management evolves, understanding the molecular mechanisms of medications like Ozempic becomes crucial. GLP-1 (glucagon-like peptide-1) receptor agonists not only suppress appetite but also influence insulin secretion, delay gastric emptying, and promote satiety. This multifaceted approach addresses the complex neuroendocrine pathways regulating hunger and energy balance, offering a scientific basis for sustained fat loss. Recent studies, such as those published in the New England Journal of Medicine (2024), affirm that these drugs modulate hypothalamic pathways, leading to durable metabolic improvements when combined with targeted lifestyle interventions.
How Does the Interaction of GLP-1 with Brain Centers Drive Appetite Suppression?
GLP-1 receptors are densely populated in the arcuate nucleus of the hypothalamus and the brainstem, regions integral to appetite regulation. Activation of these receptors influences neuropeptide signaling, notably reducing neuropeptide Y (NPY) and agouti-related peptide (AgRP), which are potent orexigens. Simultaneously, it enhances pro-opiomelanocortin (POMC) activity, promoting feelings of fullness. This neurocircuitry modulation creates a physiological environment conducive to caloric reduction without the psychological stress associated with dieting. For clinicians, leveraging this insight means tailoring interventions that optimize receptor engagement, potentially through dose titration or combination therapies, for maximal long-term benefits.
Beyond Symptom Management: The Potential of Ozempic to Rewire Metabolic Set Points
Emerging evidence suggests that medications like Ozempic may do more than suppress appetite—they might fundamentally alter the body’s metabolic set point. The concept of a ‘set point’ refers to the body’s preferred weight range, maintained through homeostatic mechanisms involving hormones such as leptin, insulin, and ghrelin. In obesity, this set point often becomes dysregulated, resisting traditional weight loss efforts. Clinical trials (see Sage Journals, 2024) indicate that GLP-1 receptor agonists may recalibrate this biological thermostat, making sustained weight loss more achievable and less prone to relapse.
Can Pharmacotherapy Reprogram the Body’s Weight Set Point?
This question is at the forefront of metabolic research. The hypothesis is that by consistently activating GLP-1 pathways, alongside lifestyle modifications, the brain’s homeostatic mechanisms adapt to a lower weight baseline. This shift may involve epigenetic changes in hypothalamic neurons, altering gene expression patterns linked to energy expenditure and appetite regulation. While promising, this area still requires longitudinal studies to confirm the permanence of such reprogramming and identify potential biomarkers predicting success.
For practitioners, integrating this understanding means not only prescribing medications but also designing comprehensive, personalized programs that support neural and hormonal adaptation. The future of weight management could lie in precision medicine approaches that combine pharmacology, neurobiology, and behavioral science, transforming how we address obesity at its core.
Interested in how these advancements translate to real-world outcomes? Explore detailed case studies and ongoing clinical trials through authoritative sources like the ClinicalTrials.gov database or consult with metabolic specialists who are pioneering these innovative strategies.
Unlocking the Long-Term Potential of Ozempic: Beyond Short-Term Weight Loss
As the scientific community delves deeper into the mechanisms of GLP-1 receptor agonists like Ozempic, emerging research suggests that these medications may reprogram the body’s metabolic set point, leading to more enduring weight loss outcomes. This revolutionary concept posits that, with consistent use under medical supervision, patients could experience a recalibration of their body’s natural weight regulation, making sustained fat loss more achievable and resistant to relapse. According to a 2025 study published in the Sage Journals, this reprogramming involves neuroendocrine adaptations that reset the body’s weight thermostat.
Can Pharmacological Intervention Rewire the Body’s Natural Weight Set Point?
Current evidence indicates that strategic activation of GLP-1 pathways, combined with personalized lifestyle modifications, can induce neuroplastic changes in hypothalamic circuits responsible for energy homeostasis. These adaptations may involve epigenetic modifications, altering gene expression related to hunger and energy expenditure. However, longitudinal studies are still needed to verify the permanence of these changes and identify predictive biomarkers for success. For practitioners, this underscores the importance of integrated treatment plans that support neural and hormonal adaptation, enhancing long-term outcomes.
For those interested in the science behind these breakthroughs, exploring detailed clinical trial data and expert analyses can provide valuable insights. Resources like the ClinicalTrials.gov database offer ongoing updates on cutting-edge research, guiding clinicians in optimizing treatment protocols.
How Does Personalized Medicine Elevate the Efficacy of Ozempic?
Personalized medicine leverages genetic, metabolic, and behavioral data to tailor weight loss interventions, maximizing efficacy and safety. Integrating pharmacotherapy with advanced diagnostics allows clinicians to identify patients who are most likely to benefit from GLP-1 receptor agonists, minimizing side effects and enhancing adherence. Telehealth platforms facilitate this approach by offering accessible, real-time monitoring and adjustments, making sophisticated, individualized care feasible for a broader population (see how telehealth is transforming weight management).
By focusing on personalized strategies, we move closer to a future where weight management is not a one-size-fits-all process but a precise science that addresses each person’s unique biological landscape. This paradigm shift promises more sustainable results and improved quality of life for patients.
What Are the Ethical and Practical Considerations in Wide-Scale Ozempic Adoption?
While the benefits of Ozempic are promising, widespread adoption raises ethical questions about accessibility, affordability, and long-term safety. Ensuring equitable access requires policy interventions and insurance coverage expansion, especially as demand surges. Additionally, ongoing surveillance is vital to monitor potential side effects over years of use, particularly in diverse populations. Clinicians must also navigate patient expectations, emphasizing that medication is part of a comprehensive plan that includes diet, exercise, and behavioral support.
Ultimately, integrating these medications into mainstream care calls for a balanced approach—embracing innovation while safeguarding patient well-being. Continued research, transparent communication, and policy support will be crucial in realizing the full potential of Ozempic for sustainable weight management.
Are you curious about how these advanced strategies could transform your weight loss journey? Share your thoughts below or explore more about physician-guided treatments at our contact page. Your path to a healthier future starts with informed decisions grounded in science.
Expert Insights & Advanced Considerations
1. Personalized Medicine’s Role in Enhancing Efficacy
Leveraging genetic and metabolic profiling allows clinicians to tailor Ozempic treatments, optimizing outcomes and minimizing side effects. This precision medicine approach is increasingly vital as we move into 2025, ensuring that weight management strategies are as effective as possible for individual patients.
2. Neuroendocrine Mechanisms and Long-Term Set Point Reprogramming
Recent research suggests that GLP-1 receptor agonists like Ozempic can induce neuroplastic changes in hypothalamic circuits, potentially reprogramming the body’s weight set point. Understanding these mechanisms helps clinicians develop interventions that support sustainable weight loss beyond temporary appetite suppression.
3. Integration of Telehealth for Widespread Accessibility
Telehealth platforms are revolutionizing access to physician-guided weight management, making prescription and monitoring of Ozempic more scalable and convenient. This technological integration is critical for expanding safe and effective treatment options in 2025.
4. Ethical and Policy Considerations
As usage of Ozempic grows, ensuring equitable access and addressing cost barriers are paramount. Policymakers and healthcare providers must collaborate to create frameworks that promote safe, fair, and sustainable distribution of these advanced therapies.
5. Combining Pharmacotherapy with Lifestyle and Behavioral Support
Maximizing long-term success involves integrating medication with personalized lifestyle modifications, behavioral therapy, and continuous monitoring. This holistic approach is essential for durable results and improved quality of life.
Curated Expert Resources
- Journal of Clinical Medicine (2024): Offers peer-reviewed insights into GLP-1 receptor agonists and long-term metabolic effects, essential for understanding the science behind Ozempic’s success.
- ClinicalTrials.gov: A comprehensive database of ongoing and completed trials, providing the latest evidence and emerging data on weight loss medications like Ozempic.
- American Society for Metabolic and Bariatric Surgery (ASMBS): Provides guidelines and consensus statements on pharmacotherapy integration into bariatric and metabolic treatments, ensuring standards of care are maintained.
- Telehealth Innovation Journals: Explore how digital health solutions are expanding access to personalized weight management programs, crucial for implementation in 2025.
- Policy Reports on Healthcare Equity: Address the ethical considerations of drug accessibility, helping stakeholders develop equitable distribution strategies.
Final Expert Perspective
In 2025, the landscape of weight loss is increasingly shaped by the integration of advanced pharmacology like Ozempic, personalized medicine, and digital health innovations. These developments are not just incremental improvements but represent a paradigm shift towards sustainable, science-backed weight management solutions. As experts, we recognize that combining neurobiological insights with accessible, ethical treatment frameworks is essential for meaningful progress. I invite healthcare professionals, researchers, and informed patients alike to engage deeply with these resources, share insights, and contribute to a future where effective, safe, and equitable weight loss strategies are universally accessible. Your expertise and participation are vital as we navigate this exciting new era.

