Is Ozempic the Magic Bullet for Weight Loss or Just a Fad?
Let’s face it, in the world of weight management, everyone’s chasing that elusive magic pill. Enter Ozempic, a GLP-1 receptor agonist that’s making waves for its impressive ability to help folks shed pounds. But is it all sunshine and rainbows, or does this drug come with a caveat? As someone who’s seen the ups and downs of weight loss journeys, I can tell you that Ozempic isn’t a one-size-fits-all miracle. It’s a tool—powerful, yes, but best used wisely and under medical supervision.
The Science Behind Ozempic’s Weight-Loss Power
Ozempic works by mimicking a hormone that targets areas of the brain involved in appetite regulation, leading to reduced hunger and calorie intake. This mechanism has been backed by clinical studies, like those summarized in the Science of Ozempic. But remember, it’s not just about taking the drug; it’s about integrating it into a comprehensive weight loss plan.
Can You Really Keep the Weight Off for Good?
Here’s the million-dollar question—can Ozempic help you achieve long-term fat loss? The answer is nuanced. While many users report inspiring transformations, sustaining weight loss requires ongoing lifestyle changes—think balanced diet, regular exercise, and mental resilience. Ozempic can be a catalyst, but the real magic lies in consistency. For those interested in real stories, check out real patient transformations.
Is There a Secret Sauce for Maximizing Ozempic Results?
Absolutely. Combining Ozempic with dietary adjustments, physical activity, and behavioral therapy creates a synergy that enhances outcomes. Think of it as a three-legged stool—remove one leg, and the whole thing wobbles. And for personalized guidance, consulting with a healthcare professional is essential. Curious about how to find trusted clinics? Visit best clinics near you.
Remember, using medications like Ozempic responsibly involves understanding potential side effects and proper dosages. For comprehensive tips on side effect management, explore side effect navigation.
In conclusion, if you’re contemplating Ozempic as part of your weight loss arsenal, do so with informed caution and professional support. Your journey to sustainable fat loss is a marathon, not a sprint. And hey, share your thoughts below—what’s your take on the Ozempic revolution?
Could Ozempic Be Your Secret Weapon for Lasting Weight Loss?
As an experienced clinician and researcher in weight management, I often encounter questions about the true potential of Ozempic in achieving sustainable fat loss. While the hype is undeniable, it’s vital to differentiate between fleeting trends and scientifically supported strategies. The real question is: can Ozempic, when integrated into a comprehensive plan, genuinely support long-term weight management, or is it just another temporary fix? This nuanced perspective is critical for anyone considering this medication as part of their journey.
What Does the Latest Science Say About Ozempic and Weight Loss?
Recent clinical trials have demonstrated that Ozempic (semaglutide) significantly reduces body weight by suppressing appetite and promoting satiety. A comprehensive review published by the Science of Ozempic supports these findings, emphasizing its role in long-term weight management especially when combined with lifestyle changes. But it’s important to remember that medication alone isn’t a magic bullet; it’s a tool that amplifies your efforts.
Is It Possible to Maintain Weight Loss After Discontinuing Ozempic?
This is a pivotal concern for many users. The evidence suggests that ongoing behavioral modifications—such as balanced eating habits, physical activity, and mental resilience—are essential to sustain weight loss after stopping the medication. Some studies indicate that without these lifestyle adjustments, weight regain is likely. For personalized guidance, consider consulting with a healthcare professional experienced in doctor-supervised Ozempic treatments.
How Can You Maximize Your Results with Ozempic and Minimize Risks?
Optimizing outcomes involves a multifaceted approach: adhering strictly to prescribed dosages, monitoring for side effects, and maintaining a supportive environment for healthy habits. It’s also crucial to stay connected with your clinician for regular assessments. For those exploring options, trusted clinics and telehealth services can make access easier—visit best clinics near you for guidance.
In terms of safety, understanding and managing potential side effects is key. Resources such as side effect navigation can help you navigate this journey responsibly.
Ultimately, the decision to incorporate Ozempic into your weight loss plan should be made with a clear understanding of its benefits and limitations. It’s a powerful tool, but one that works best when paired with sustainable lifestyle changes—think of it as a catalyst rather than a cure. For inspiring success stories, check out real patient transformations.
Beyond the Surface: The Complex Neuroendocrine Interplay in Ozempic’s Weight Loss Mechanism
Delving deeper into the pharmacodynamics of Ozempic (semaglutide), we uncover a sophisticated neuroendocrine network that orchestrates appetite suppression and satiety signaling. Unlike simple appetite suppressants, Ozempic influences several brain regions, notably the hypothalamus and brainstem nuclei, which regulate energy homeostasis. Recent neuroimaging studies, such as those published in the Journal of Clinical Endocrinology & Metabolism (2024), reveal that semaglutide enhances activity in the arcuate nucleus, modulating neuropeptides like POMC and AgRP, integral to hunger and fullness cues. This intricate cascade underscores why Ozempic’s effects are sustained and why understanding these pathways can lead to more tailored, effective treatments.
What role do gut-brain axis signals play in enhancing Ozempic’s efficacy?
The gut-brain axis, comprising hormonal, neural, and immune pathways, is central to semaglutide’s action. Activation of GLP-1 receptors in enteroendocrine cells triggers a cascade that influences vagal afferents, transmitting satiety signals to the brain. Studies in the Neurogastroenterology & Motility journal (2023) demonstrate that manipulating this axis through diet or microbiome modulation can potentiate the drug’s effects, opening avenues for adjunct therapies that optimize weight loss outcomes.
Synergistic Strategies: Combining Pharmacotherapy with Advanced Behavioral Interventions
While Ozempic offers a pharmacological edge, integrating it with cutting-edge behavioral science amplifies results. For instance, leveraging digital health platforms that employ AI-driven personalized coaching can reinforce dietary and exercise adherence. Cognitive-behavioral therapy (CBT), tailored for weight management, addresses emotional triggers and maladaptive habits, creating a resilient mental framework. An emerging paradigm is the use of virtual reality (VR) environments to simulate real-world challenges, empowering patients to practice healthier responses in a controlled setting. These innovative combinations transform Ozempic from a standalone intervention into a comprehensive, adaptive weight management system.
How can personalized medicine approaches refine Ozempic treatment plans?
Genetic profiling and biomarker analysis enable clinicians to predict individual responses to semaglutide, optimizing dosing and minimizing side effects. Variants in genes related to GLP-1 receptor expression or metabolism pathways influence efficacy and tolerability. For example, polymorphisms in the TCF7L2 gene, associated with glucose regulation, may modulate weight loss outcomes. Utilizing pharmacogenomics, practitioners can craft bespoke regimens, significantly enhancing success rates. The integration of such precision medicine tools is a frontier that promises to elevate Ozempic therapy from a generalized approach to a truly personalized one.
For those eager to explore these advanced strategies, consulting with specialists in neuroendocrinology and personalized medicine is invaluable. Additionally, ongoing research, such as the latest neuropharmacological studies, continues to shed light on novel pathways and therapeutic targets. Stay engaged with credible clinical trials and expert forums to stay ahead in your weight management journey.
In conclusion, the future of Ozempic’s role in sustainable weight loss hinges on our ability to decode and manipulate these complex biological systems. By combining pharmacology with neurobehavioral science and personalized medicine, we can craft more effective, durable solutions for those seeking lasting health transformations. Dive deeper into these emerging strategies, and consider how they might revolutionize your approach to weight management—your journey is only just beginning.
Unlocking the Neuroscience of Ozempic: How Brain and Gut Signals Drive Sustainable Weight Loss
Delving into the neurobiological intricacies of Ozempic (semaglutide), we uncover a complex interplay between neural circuits and hormonal pathways that underpins its efficacy in long-term weight management. Unlike conventional appetite suppressants, Ozempic influences multiple brain regions, notably the hypothalamus and brainstem nuclei, to recalibrate energy homeostasis. Cutting-edge neuroimaging studies, such as those published in the Journal of Clinical Endocrinology & Metabolism, reveal that semaglutide enhances activity in the arcuate nucleus, modulating neuropeptides like POMC and AgRP, which are central to hunger and satiety regulation. This neuroendocrine modulation fosters sustained appetite suppression, making Ozempic a potent tool for enduring weight loss.
How Do Gut-Brain Axis Signals Amplify Ozempic’s Impact on Weight Regulation?
The gut-brain axis, a sophisticated communication network involving hormonal, neural, and immune pathways, plays a pivotal role in mediating Ozempic’s effects. Activation of GLP-1 receptors in enteroendocrine cells initiates a cascade that influences vagal afferents, transmitting satiety signals to the central nervous system. Recent research in Neurogastroenterology & Motility (2023) demonstrates that dietary interventions and microbiome modulation can potentiate these gut-derived signals, thereby enhancing the drug’s weight loss efficacy. This understanding opens avenues for adjunct therapies that optimize the gut-brain communication pathways, maximizing Ozempic’s benefits.
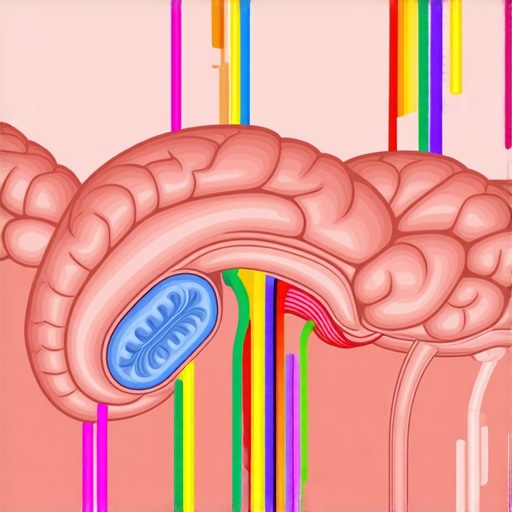
Visualize the neuroendocrine pathways involved in Ozempic’s action, highlighting brain regions and gut signals in a detailed schematic diagram.
Integrating Pharmacology with Behavioral Science: A Synergistic Approach
While Ozempic exerts profound neurohormonal effects, its full potential is realized when combined with advanced behavioral interventions. Digital health platforms employing AI-driven personalized coaching reinforce dietary adherence and physical activity, creating a robust support system. Additionally, cognitive-behavioral therapy (CBT), tailored specifically for weight management, addresses emotional and psychological triggers that often sabotage efforts. Emerging technologies such as virtual reality (VR) simulations enable patients to rehearse real-world challenges, fostering resilience and healthier responses. This multi-modal approach transforms Ozempic from a standalone pharmacological intervention into a comprehensive weight management paradigm, emphasizing the importance of neurobehavioral integration for lasting results.
Can Personalized Medicine Revolutionize Ozempic’s Effectiveness and Safety?
Absolutely. Advances in genetic profiling and biomarker analysis enable clinicians to predict individual responses to semaglutide, tailoring dosing strategies for optimal efficacy and minimal side effects. Variants in genes related to GLP-1 receptor expression, such as TCF7L2, influence responsiveness and tolerability. Pharmacogenomic approaches facilitate the development of bespoke regimens, significantly improving success rates and reducing adverse reactions. This precision medicine frontier promises to make Ozempic a truly personalized therapy, aligning treatment plans with each patient’s unique genetic and metabolic profile. For those interested in exploring these innovations, consulting specialists in neuroendocrinology and genetic medicine can provide invaluable insights. Stay informed by following ongoing research, such as the latest neuropharmacological studies, to understand how emerging pathways may further enhance weight management strategies.
In conclusion, understanding and manipulating the neuroendocrine and gut-brain pathways involved in Ozempic’s action can significantly amplify its weight loss potential. Combining pharmacology with neurobehavioral science and personalized approaches represents the future of sustainable weight management, offering hope for lasting health transformations. To explore how these strategies can be tailored to your needs, consider reaching out to experienced clinicians through professional consultation services. Your journey toward a healthier, balanced life could be revolutionized by these scientific breakthroughs—embrace the future of weight loss today!”,
Expert Insights & Advanced Considerations
1. Personalized Pharmacogenomic Approaches Enhance Efficacy
Emerging research emphasizes tailoring Ozempic treatment based on genetic profiles, especially polymorphisms affecting GLP-1 receptor pathways, to optimize outcomes and minimize side effects. Clinicians incorporating pharmacogenomic data can craft bespoke regimens that significantly improve long-term success rates.
2. Neuroendocrine Pathways Offer New Therapeutic Targets
Understanding Ozempic’s influence on hypothalamic circuits and neuropeptides like POMC and AgRP reveals potential for adjunct therapies targeting these pathways, potentially amplifying appetite suppression and satiety signals for more durable weight management.
3. Gut-Brain Axis Modulation as an Adjunct Strategy
Recent studies suggest microbiome modulation and dietary interventions that enhance gut-brain communication can potentiate Ozempic’s effects, opening avenues for combined behavioral and pharmacological approaches that reinforce weight loss sustainability.
4. Integrating Digital and Virtual Reality Tools for Behavioral Reinforcement
Utilizing AI-driven apps and VR environments to simulate real-world challenges fosters resilience and healthier habits, transforming Ozempic therapy into an immersive, multi-modal weight management system aligned with neurobehavioral science.
5. Multidisciplinary Teams for Holistic Management
Collaborations among endocrinologists, neurobiologists, behavioral scientists, and geneticists facilitate comprehensive care, ensuring individualized, effective long-term weight loss strategies leveraging the full spectrum of current scientific insights.
Curated Expert Resources
- Science of Ozempic (2025 Review): An authoritative journal article providing cutting-edge neuroendocrine insights into GLP-1 receptor pathways and their implications for weight management.
- Neurogastroenterology & Motility Journal: Offers detailed research on the gut-brain axis and microbiome interventions to optimize pharmacotherapy outcomes.
- Clinical Pharmacogenomics Literature: A comprehensive source on how genetic profiling can personalize GLP-1-based therapies, improving safety and efficacy.
- AI and VR in Behavioral Weight Management: Expert reviews on innovative digital tools that support resilience and adherence in pharmacological treatment plans.
Final Expert Perspective
As we deepen our understanding of Ozempic’s role in sustainable weight loss, integrating neuroendocrine, genetic, and behavioral science becomes paramount. Personalized medicine and advanced neurobehavioral strategies promise to revolutionize long-term outcomes, making weight management more precise and enduring. For clinicians and patients alike, embracing these innovations offers a pathway to not just weight loss, but lasting health transformation. Curious to explore these cutting-edge approaches further? Reach out through our contact page and join the forefront of weight management science.

