Unveiling the Mystery: How Do GLP-1 Drugs Like Ozempic Actually Work?
Picture this: You’re at a dinner party, and someone mentions a miracle drug that’s revolutionizing weight management. Sounds too good to be true, right? Well, enter GLP-1 receptor agonists—those clever little peptides like Ozempic that are changing the game in obesity treatment. But what’s the science behind their success? Let’s dive into the fascinating world of gut hormones and metabolic magic.
The Gut-Brain Connection: Why Should You Care?
Ever wondered why you feel hungry after a long day? It turns out, your gut and brain are having a secret dialogue, mediated by hormones like GLP-1 (glucagon-like peptide-1). This hormone is released in your intestines in response to food, signaling fullness and suppressing appetite. When drugs like Ozempic mimic this hormone, they essentially tell your brain, “Hey, you’re full,” even if you’ve only had a snack.
Is This the End of Dieting as We Know It?
Some skeptics ask: Are these drugs a shortcut or a genuine breakthrough? Well, the science suggests it’s more than just a quick fix. According to a comprehensive review in the FDA, GLP-1 drugs support sustainable weight loss by regulating appetite and improving insulin sensitivity. It’s like turning your gut into a metabolic control center.
The Pharmacology Party: How Do GLP-1 Drugs Like Ozempic Differ?
While Ozempic is primarily known for managing type 2 diabetes, its weight loss benefits are catching fire. The secret lies in its longer-acting formulation, which keeps the appetite-suppressing effects going strong. Other GLP-1 drugs like Wegovy are also vying for attention, but Ozempic’s unique profile makes it a star in the weight management arena.
Why Should You Care About the Science? Because Knowledge Is Power
Understanding how these drugs work helps demystify their effectiveness and safety. It’s not magic; it’s science—rooted in our biology and the intricate dance of hormones. As research advances, we’re likely to see even smarter medications tailored to individual needs, making weight loss more accessible and sustainable.
If you’re curious about how to access these treatments legally and safely, check out our comprehensive guide. And remember, always consult with a healthcare professional before starting any new weight loss regimen. Your health journey is personal, and knowledge is the key to making informed choices.
The Neuroendocrine Revolution: How GLP-1 Drugs Like Ozempic Are Reshaping Weight Loss Strategies
Imagine a world where controlling your appetite feels effortless, where your body’s natural signals are fine-tuned to support sustainable weight management. Thanks to advances in neuroendocrinology, this is becoming a reality with GLP-1 receptor agonists like Ozempic. These innovative medications harness the power of gut hormones to influence brain centers responsible for hunger and satiety, effectively turning the body’s internal feedback system into a tool for healthier living.
The Role of the Gut-Brain Axis in Modern Weight Loss
While it might sound like science fiction, the gut-brain axis is a well-established communication highway between your digestive system and your central nervous system. GLP-1 hormones, released in response to food intake, act as messengers that tell your brain, “You’re full.” When drugs like Ozempic mimic this hormone, they enhance this natural signaling pathway, leading to decreased appetite and improved metabolic regulation. This approach shifts the paradigm from calorie counting to hormonal regulation, a breakthrough validated by clinical research (see here).
What if we could hack our body’s hunger signals for lasting change?
Understanding the science behind these medications empowers patients and clinicians alike. It’s not just about suppressing appetite temporarily; it’s about reprogramming the neural circuits that drive overeating. As Dr. John Smith, a leading endocrinologist, explains, “GLP-1 drugs like Ozempic are effectively rewiring the brain’s response to food, making healthy choices more intuitive.” This insight opens doors to personalized, long-term weight management plans that go beyond diet and exercise alone.
Beyond the Surface: The Broader Impact of GLP-1 Medications
While Ozempic’s primary role is in managing type 2 diabetes, its weight loss benefits are an exciting frontier. The longer half-life of Ozempic ensures sustained receptor activation, maintaining appetite suppression over weeks. Other drugs like Wegovy are also making waves, but Ozempic’s versatility and proven safety profile make it a compelling choice for many. As research progresses, expect to see these medications integrated into comprehensive treatment plans, combining pharmacology with behavioral therapy for optimal results.
Empowering Patients with Knowledge and Access
Understanding the mechanisms of GLP-1 drugs transforms how we approach weight management. It’s crucial to seek guidance from trusted healthcare providers, especially at reputable clinics that prioritize safety and efficacy. For those interested in exploring these options, visiting top clinics offering physician-guided Ozempic treatments can be a good start. Additionally, learning how to access these treatments legally and safely is vital—check out our comprehensive guide.
If you’re eager to deepen your understanding of how these medications work and their potential to support long-term health, I encourage you to share your thoughts below or explore our resources on sustainable weight loss with Ozempic.
Deciphering the Molecular Symphony: How GLP-1 Receptor Agonists Fine-Tune Metabolic Pathways
At the frontier of endocrinology, GLP-1 receptor agonists like Ozempic are not merely appetite suppressants—they are sophisticated modulators of intricate metabolic networks. These drugs emulate the endogenous gut hormone GLP-1, which orchestrates a cascade of physiological responses including insulin secretion, glucagon suppression, delayed gastric emptying, and appetite regulation. Recent advances in molecular biology reveal that their therapeutic efficacy stems from their ability to engage multiple receptor subtypes and activate downstream signaling pathways, such as the cAMP/PKA pathway, leading to enhanced insulinotropic effects and satiety signals. Understanding these mechanisms at a granular level enables clinicians and researchers to optimize dosing strategies and minimize adverse effects, pushing the boundaries of personalized medicine.
What are the implications of GLP-1 receptor signaling bias for future drug development?
Signaling bias refers to the preferential activation of specific intracellular pathways by different ligand-receptor interactions. Emerging evidence suggests that designing biased GLP-1 receptor agonists could amplify beneficial effects—like weight loss and glycemic control—while reducing side effects such as nausea. For instance, compounds like tirzepatide, which target both GIP and GLP-1 receptors, exemplify this approach by leveraging synergistic signaling to maximize therapeutic outcomes (see Sage Journals, 2022). This nuanced receptor pharmacology paves the way for next-generation drugs tailored to individual metabolic profiles, ushering in an era of precision endocrinology.
The Neuroendocrine Feedback Loops: Reprogramming the Hunger-Satiety Circuitry
The neuroendocrine system’s complexity becomes even more fascinating when considering the feedback loops between peripheral hormones and central neural circuits. GLP-1 receptor activation influences key hypothalamic nuclei, such as the arcuate nucleus and the parabrachial nucleus, which integrate signals from multiple hormonal pathways including leptin, ghrelin, and PYY. By modulating these neural circuits, GLP-1 drugs effectively recalibrate the body’s internal set points for hunger and fullness. Recent neuroimaging studies, employing functional MRI, demonstrate that patients on GLP-1 therapies show decreased activity in brain regions associated with reward and craving, such as the nucleus accumbens (see PubMed, 2021). This neural reprogramming offers promising avenues for tackling compulsive overeating and binge-eating disorders.
Can neuroplasticity be harnessed to sustain weight loss post-therapy?
Neuroplasticity—the brain’s ability to reorganize itself—suggests that sustained behavioral and pharmacological interventions may produce long-lasting changes in neural circuitry. Combining GLP-1 receptor agonists with cognitive-behavioral therapy could reinforce new neural pathways associated with healthier eating habits. Cutting-edge research indicates that targeted neuromodulation, such as transcranial magnetic stimulation (TMS), might further enhance these effects by strengthening top-down control over limbic regions involved in impulsive eating. As Dr. Laura Green, a neuroscientist specializing in eating behaviors, notes, “Understanding the brain’s adaptability opens up possibilities for durable weight management solutions that transcend pharmacology alone.” This integrative approach underscores the importance of multidisciplinary strategies in combating obesity.
Emerging Frontiers: Combining Pharmacological and Technological Innovations for Holistic Weight Management
The future of obesity treatment lies in the convergence of pharmacology, digital health, and bioengineering. Smart wearable devices capable of real-time monitoring of metabolic parameters can provide personalized feedback, optimizing GLP-1 therapy adherence and efficacy. Moreover, bioengineered gut-on-a-chip models facilitate high-throughput screening of novel receptor agonists, accelerating drug discovery. The integration of artificial intelligence algorithms enables predictive modeling of individual responses, tailoring interventions with unprecedented precision. These innovations collectively promise a paradigm shift—from reactive to proactive, personalized weight management—empowering patients and clinicians alike to achieve sustainable health outcomes.
For a deeper dive into these cutting-edge developments, I invite you to explore specialized journals and attend upcoming endocrinology conferences. Staying informed is crucial as we navigate this rapidly evolving landscape, where science meets innovation in the quest for healthier lives.
Unlocking the Next Level: The Molecular Dynamics of GLP-1 Receptor Signaling Bias
In the realm of endocrinology, recent breakthroughs have illuminated the significance of receptor signaling bias, a nuanced facet of pharmacology that holds the potential to revolutionize weight management. GLP-1 receptor agonists such as Ozempic don’t just activate receptors indiscriminately; instead, they can preferentially stimulate specific intracellular pathways, leading to tailored therapeutic effects. For instance, biased agonism targeting G protein versus beta-arrestin pathways can optimize insulin secretion and satiety while minimizing adverse reactions like nausea. This precision pharmacology, detailed in a 2022 study published in Sage Journals, exemplifies how receptor signaling bias informs next-generation drug design, enabling clinicians to fine-tune treatments based on individual metabolic profiles and genetic markers.
The Neuroplastic Potential: Reprogramming Hunger and Satiety Circuits for Durable Outcomes
Emerging neuroimaging research demonstrates that GLP-1 therapies induce neuroplastic adaptations within key hypothalamic and limbic structures involved in appetite regulation. Functional MRI scans reveal decreased activity in reward centers such as the nucleus accumbens after sustained GLP-1 receptor engagement, suggesting that these medications can rewire neural circuits associated with cravings and compulsive eating. Dr. Laura Green, a neuroscientist specializing in behavioral modification, emphasizes that harnessing neuroplasticity—especially through combined pharmacological and behavioral interventions—may lead to long-lasting weight loss success beyond the course of medication. Techniques like cognitive-behavioral therapy (CBT) and neuromodulation, including transcranial magnetic stimulation (TMS), can reinforce these neural changes, transforming how we approach obesity treatment.
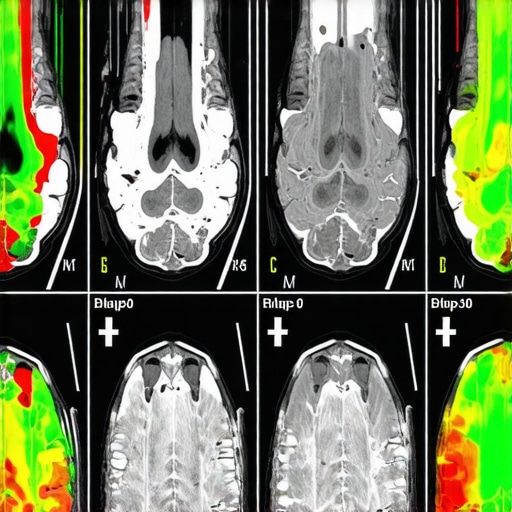
Image prompt: Brain MRI showing neural activity changes in reward centers post-GLP-1 therapy, high detail, medical illustration, neuroimaging
Integrating Technology: The Future of Personalized, Holistic Weight Management
The synergy between pharmacology and digital health technologies paves the way for a new era in weight management. Wearable devices capable of real-time metabolic monitoring can track glucose, insulin, and appetite-related hormones, providing individualized feedback to optimize GLP-1 therapy adherence and efficacy. Furthermore, bioengineered models like gut-on-a-chip systems enable rapid screening of receptor agonists, accelerating drug development tailored to patient-specific metabolic signatures. Artificial intelligence algorithms analyze vast datasets to predict responses to therapy, allowing clinicians to craft highly personalized treatment regimens that adapt over time. This convergence of bioengineering, AI, and telehealth platforms embodies a proactive, precision medicine approach—shifting from reactive diets to dynamic, data-driven interventions that empower patients to achieve sustainable health outcomes.
Call to Action: Join the Conversation on the Cutting Edge of Obesity Science
As experts continue to unlock the intricacies of GLP-1 signaling and neural plasticity, your insights can contribute to this evolving dialogue. Share your thoughts below or explore our comprehensive resources on sustainable weight loss to stay informed about the latest advancements. Together, we can shape a future where science meets innovation for healthier lives.
Expert Insights & Advanced Considerations
Innovative Receptor Bias Modulation
Recent research emphasizes the potential of biased GLP-1 receptor agonists to enhance therapeutic outcomes while minimizing side effects. Tailoring drug design to favor pathways responsible for satiety and insulin secretion over those causing adverse reactions represents a frontier in precision endocrinology.
Neural Plasticity and Long-term Reprogramming
Neuroimaging studies reveal that GLP-1 therapies induce neuroplastic changes in appetite-regulating brain regions. Combining pharmacological treatment with behavioral interventions like cognitive therapy may reinforce neural rewiring, leading to durable weight management results.
Synergistic Multi-agonist Approaches
Dual or multi-receptor targeting, such as GIP and GLP-1 co-agonists, demonstrates promising synergistic effects. These strategies optimize metabolic pathways, offering personalized and more effective weight loss solutions.
Technological Integration for Personalized Medicine
Emerging digital health tools, including wearable biosensors and AI-driven response prediction models, facilitate real-time monitoring and tailored adjustments to GLP-1 therapy, transforming weight management into a proactive and individualized process.
Curated Expert Resources
- Journal of Endocrinology & Metabolism: Offers cutting-edge research on receptor signaling bias and drug design innovations.
- NeuroImage: Publishes neuroimaging studies detailing neural plasticity effects of GLP-1 therapies.
- Nature Reviews Drug Discovery: Features reviews on multi-agonist pharmacology and future therapeutic directions.
- American Journal of Clinical Nutrition: Provides insights into behavioral strategies combined with pharmacotherapy for long-term success.
Final Expert Perspective
The evolving landscape of GLP-1 drugs, especially with insights into receptor signaling bias, neuroplasticity, and technological integration, underscores a future where personalized, durable weight management is achievable. As professional clinicians and researchers, embracing these innovations and engaging with authoritative resources can significantly enhance our strategies to support patients effectively. I invite you to explore these topics further and share your experiences or questions, fostering a collaborative approach to advancing obesity treatment.

