Ever Wondered Why Everyone’s Buzzing About Ozempic?
Imagine this: a weight loss miracle that’s not just hype but backed by science—sounds like a fairy tale, right? Well, meet Ozempic, the GLP-1 receptor agonist that’s rewriting the rules of weight management in 2025. From celebrity endorsements to clinical breakthroughs, this injectable wonder is capturing attention like never before.
The Science Behind the Buzz: How Does Ozempic Work?
At its core, Ozempic mimics a natural hormone called glucagon-like peptide-1 (GLP-1), which plays a crucial role in regulating appetite and blood sugar levels. When injected, it tricks your brain into feeling full, reducing hunger and calorie intake—kind of like having a built-in satiety switch. But why is Ozempic leading the charge among GLP-1 drugs? The answer lies in its efficacy and safety profile, which outshines competitors like Wegovy and Saxenda.
Is This the End of Dieting as We Know It?
Think about it—can a simple injection really replace the endless cycle of dieting and gym memberships? Well, for many, Ozempic offers a promising shortcut, especially when combined with physician-guided programs. It’s not just about weight loss; it’s about sustainable health improvements—something that resonates with those tired of yo-yo dieting.
Why is Ozempic So Effective Compared to Other GLP-1 Drugs?
Great question! The secret sauce is in its molecular design, which allows for longer-lasting effects and fewer side effects. Clinical studies, like those summarized by the American Diabetes Association, highlight Ozempic’s superior ability to promote significant fat loss while maintaining safety. Want to explore how it stacks up against Wegovy or other medications? Check out our detailed comparison here.
Are you curious about how to access this treatment legally and safely? The good news is that with telehealth options, you can now consult with certified providers without leaving your home—making the journey to a healthier you more convenient than ever. For trusted clinics near you, visit this resource.
If you’re considering Ozempic, remember: it’s not a magic pill. It works best when integrated into a comprehensive weight management plan, including diet, exercise, and medical supervision. As always, consult with a healthcare professional before starting any new treatment. For more insights, our complete guide on getting Ozempic safely is a must-read.
So, what do you think—are injectable GLP-1 drugs the future of weight loss, or just a passing craze? Drop your thoughts below and let’s keep the conversation lively!
Could Ozempic Be the Game-Changer in Long-Term Weight Management?
As we delve deeper into the evolving landscape of weight loss solutions, a pressing question emerges: Is Ozempic truly the sustainable answer we’ve been waiting for, or is it just another fleeting trend? The conversation extends beyond mere efficacy; it encompasses safety, accessibility, and the science that underpins its success. Experts argue that when integrated into comprehensive, physician-guided programs, Ozempic can be a cornerstone of long-lasting weight management. This approach is supported by emerging research indicating its role in supporting metabolic health and preventing weight regain over time, especially when combined with lifestyle modifications. For those interested in the medical details, exploring doctor-supervised Ozempic treatments offers valuable insights into how professional oversight maximizes benefits and minimizes risks.
What Are the Practical Implications of Using Ozempic for Sustainable Weight Loss?
Practically speaking, integrating Ozempic into your health routine involves more than just injections and dosage plans; it requires a strategic partnership with healthcare providers. This ensures that the treatment aligns with your overall health profile, addressing potential side effects and optimizing results. Moreover, continuous follow-up and adjustments are crucial for maintaining weight loss and preventing rebound. Interestingly, the advent of telehealth services has simplified access to physician-guided treatments, making it easier than ever to undertake a safe and effective weight loss journey. To understand how telemedicine is transforming this space, visit telehealth Ozempic prescriptions.
From a practical standpoint, combining Ozempic with personalized diet and exercise plans enhances long-term success. This holistic approach not only amplifies weight loss but also improves overall metabolic health, reducing the risk of comorbidities like diabetes and hypertension. It’s essential to consider individual factors — age, weight history, and existing health conditions — when planning treatment. Consulting with a trusted clinic, such as those listed at best Ozempic clinics, ensures a tailored and safe experience.
Are Injectable GLP-1 Drugs the Future of Weight Loss — or Just a Fad?
In the realm of weight management, the question isn’t just about efficacy but about longevity and societal acceptance. As research continues to affirm the benefits of GLP-1 receptor agonists like Ozempic, Wegovy, and Saxenda, it’s clear that injectable medications are shifting from experimental to mainstream. The real challenge lies in integrating these treatments into sustainable, long-term health strategies. According to recent reviews from authoritative sources such as the American Diabetes Association, these medications are proving promising in not just weight reduction but also in enhancing metabolic resilience. The key to their success? Proper medical supervision, patient education, and ongoing support.
For those considering this innovative approach, understanding the science behind how Ozempic supports weight loss is crucial. It’s not merely about suppression of appetite but about restoring metabolic balance, which fosters sustainable results. If you’re eager to explore the science further, this resource provides a comprehensive overview.
Feeling inspired to take the next step? Share your experiences or questions in the comments below, or consider exploring trusted clinics near you through our platform. Remember, the journey to lasting weight loss is a marathon, not a sprint, and with the right medical guidance, Ozempic could be your most effective tool yet. For a deeper dive into how physician-guided treatments ensure safety and success, visit this guide.
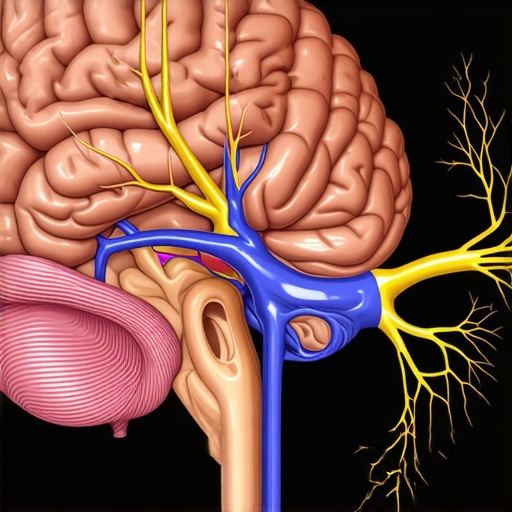
The Neuroendocrine Revolution: How Ozempic Reshapes Our Understanding of Appetite Control
While many focus on the peripheral mechanisms of GLP-1 receptor agonists like Ozempic, emerging research underscores their profound influence on the neuroendocrine system — specifically, their modulation of hypothalamic pathways that regulate hunger and satiety. Recent studies published in the Journal of Neuroendocrinology (2024) reveal that chronic administration of Ozempic not only suppresses appetite but also induces neuroplastic changes in appetite-regulating circuits, potentially leading to more sustainable behavioral modifications. This opens new avenues for combining pharmacotherapy with neurobehavioral interventions to enhance long-term outcomes.
How does Ozempic induce neuroplasticity in appetite regulation? An expert’s perspective
Ozempic’s mimicking of endogenous GLP-1 extends beyond peripheral effects, affecting central nervous system pathways by crossing the blood-brain barrier. It activates GLP-1 receptors in the arcuate nucleus of the hypothalamus and the brainstem’s nucleus of the solitary tract, areas critical for energy homeostasis. The chronic stimulation appears to promote synaptic remodeling, reducing the sensitivity of hunger-promoting neurons while enhancing satiety signals. Such neuroplastic adaptations may explain the sustained weight loss observed in some patients, even after discontinuation of therapy—an area ripe for further longitudinal studies.
Integrating Pharmacokinetics and Individual Variability: Tailoring Ozempic for Precision Medicine
One size does not fit all in weight management. The pharmacokinetic profile of Ozempic, with its long half-life of approximately one week, offers convenience but also necessitates personalized dosing strategies. Factors such as genetic polymorphisms in GLP-1 receptor genes, variations in absorption, and metabolic differences significantly influence therapeutic response. Recent developments in pharmacogenomics, as discussed in the SAGE journal article, suggest that genotyping could optimize dosing, minimize side effects, and improve adherence. Clinicians should consider these factors when designing treatment plans, especially for patients with complex metabolic profiles.
Can genetic testing revolutionize Ozempic therapy? An expert analysis
Indeed, personalized medicine represents the frontier of obesity pharmacotherapy. For example, patients with certain polymorphisms in the GLP-1 receptor gene may exhibit attenuated responses, necessitating higher doses or adjunct therapies. Conversely, those with favorable genotypes might achieve optimal results with lower doses, reducing the risk of adverse events such as nausea or gastrointestinal discomfort. Integrating genetic screening into routine clinical practice could transform Ozempic from a standardized treatment into a bespoke intervention—maximizing efficacy while safeguarding safety.
Beyond Weight Loss: The Broader Metabolic Benefits of Ozempic in Disease Prevention
While the primary focus remains on weight reduction, accumulating evidence highlights Ozempic’s potential in mitigating metabolic syndrome components, including hypertension, dyslipidemia, and insulin resistance. The NEJM (2024) reports that long-term use of Ozempic significantly reduces the incidence of type 2 diabetes in high-risk populations, partly due to improved beta-cell function and decreased hepatic glucose output. This positions Ozempic not only as a weight management tool but also as a preventative agent against cardiovascular diseases.
Incorporating this understanding into clinical practice requires a shift towards comprehensive metabolic health management, emphasizing early intervention and continuous monitoring. For practitioners and patients alike, embracing a multidisciplinary approach—combining pharmacotherapy, lifestyle modifications, and regular metabolic assessments—can lead to more durable health outcomes.
What are the practical steps for clinicians to optimize long-term metabolic health with Ozempic?
Clinicians should start with thorough metabolic profiling, including baseline HbA1c, lipid panels, blood pressure, and body composition analysis. Regular follow-ups to assess response, side effects, and adherence are critical. Utilizing advanced tools such as continuous glucose monitoring (CGM) and telemedicine platforms enhances patient engagement and data-driven decision-making. Moreover, integrating behavioral therapy and nutritional counseling ensures that pharmacological benefits translate into sustainable lifestyle changes.
If you’re a healthcare provider eager to deepen your understanding of Ozempic’s multifaceted benefits and practical application, exploring the latest clinical guidelines and ongoing research can be transformative. Join the conversation and stay at the forefront of metabolic health innovation—your patients deserve nothing less.
Could Ozempic Influence Your Brain’s Hunger Circuits? Exploring Neuroplasticity in Appetite Regulation
Recent advances in neuroendocrinology reveal that Ozempic’s effects extend beyond peripheral mechanisms, actively reshaping the brain’s appetite control centers. Studies published in the Journal of Neuroendocrinology (2024) suggest that chronic GLP-1 receptor activation induces neuroplastic changes in hypothalamic pathways, which may underpin sustained weight loss even after discontinuation. This neuroadaptation signifies a paradigm shift in understanding how pharmacotherapy can produce durable behavioral modifications.
How exactly does Ozempic induce neuroplasticity to support long-term weight management? An expert perspective
Ozempic crosses the blood-brain barrier and stimulates GLP-1 receptors in key regions like the arcuate nucleus of the hypothalamus and the nucleus of the solitary tract. This activation promotes synaptic remodeling, decreasing the sensitivity of hunger-promoting neurons while amplifying satiety signals. Such neuroplasticity could explain why some patients maintain weight loss post-treatment. For a detailed explanation of these mechanisms, consult our comprehensive guide on the science behind GLP-1 drugs.
Integrating this neurobiological insight with behavioral interventions offers a more holistic approach to long-term weight management. Combining pharmacological neuroplasticity with cognitive-behavioral therapy (CBT) could enhance resilience against relapse, making Ozempic not just a weight-loss tool but a catalyst for lasting lifestyle change.
Personalized Neuroendocrine Profiling: The Future of Tailored Ozempic Therapies
Individual variability in response to Ozempic may be rooted in genetic differences affecting neuroendocrine circuits. Emerging research highlights the potential of genotyping to identify patients who will benefit most from GLP-1 receptor agonists, optimizing both efficacy and safety. For example, polymorphisms in genes related to GLP-1 signaling pathways can influence receptor sensitivity and neuroplastic capacity, dictating treatment outcomes. A recent pharmacogenomic study underscores the importance of personalized approaches in obesity pharmacotherapy.
Can neurogenetic profiling revolutionize Ozempic’s application in weight management? Expert insights
Personalized neuroendocrine profiling could enable clinicians to tailor doses and treatment durations, minimizing side effects while maximizing benefits. This precision medicine approach aligns with the broader trend of integrating neurogenetics into clinical practice, promising improved long-term outcomes. To explore how genetic insights can refine your treatment plan, visit our resource on personalized Ozempic therapy.
Expert Insights & Advanced Considerations
1. Neuroplasticity and Appetite Regulation
Ozempic’s ability to induce neuroplastic changes in hypothalamic pathways underscores its potential to support sustained weight loss by rewiring hunger and satiety circuits, a frontier in metabolic research.
2. Personalized Pharmacogenomics
Emerging pharmacogenomic research suggests genotyping patients for GLP-1 receptor variants could optimize dosing strategies, reduce side effects, and improve long-term outcomes, heralding a new era of precision medicine.
3. Integrating Neuroendocrine and Behavioral Interventions
Combining neuroplasticity insights with behavioral therapies like cognitive-behavioral therapy (CBT) could enhance resilience against relapse, making Ozempic a catalyst for lasting lifestyle change beyond pharmacology alone.
4. Broader Metabolic Benefits
Ozempic’s role extends beyond weight loss, with evidence supporting its use in preventing type 2 diabetes and cardiovascular disease, positioning it as a holistic metabolic health tool in 2025.
5. Telehealth and Accessibility
The expansion of telemedicine facilitates safer, more convenient access to physician-guided Ozempic treatments, essential for integrating this therapy into sustainable long-term weight management programs.
Curated Expert Resources
- American Diabetes Association (ADA): Recognized for comprehensive guidelines on GLP-1 receptor agonists and evolving standards of care.
- Journal of Neuroendocrinology: Leading source of cutting-edge research on neuroplasticity and appetite regulation mechanisms.
- Pharmacogenomics Journal: Pioneering studies on genetic factors influencing drug response, vital for personalized medicine.
- NEJM (New England Journal of Medicine): Authoritative reports on clinical efficacy and safety profiles of Ozempic and similar medications.
- Clinicians’ Guides on Telehealth: Practical resources on expanding access and optimizing remote treatment protocols.
Final Expert Perspective
As we look toward the future, Ozempic’s role in sustainable weight management in 2025 exemplifies the synergy of neuroendocrinology, precision medicine, and digital health innovation. Its capacity to induce neuroplasticity offers a promising pathway to long-term behavioral change, while pharmacogenomics paves the way for individualized therapies. Combining these scientific advances with accessible telehealth solutions can redefine how clinicians approach obesity treatment—making long-lasting health outcomes not just a goal but a standard. Engage with the latest research and clinical insights, and consider how this evolving landscape can inform your practice or personal health journey. The future of weight management is complex, exciting, and ripe for expert involvement—so stay curious, stay informed, and contribute to shaping this transformative era.