Ozempic in 2025: The Long Game of Fat Loss — Are We Ready?
Imagine a world where shedding pounds isn’t just a fleeting victory but a sustainable lifestyle. Well, folks, the future’s knocking — and it’s called Ozempic. As we stand at the cusp of 2025, the science behind this revolutionary GLP-1 receptor agonist is revealing secrets that could redefine long-term weight management. No more crash diets or miracle pills; this is about understanding the real deal behind Ozempic’s lasting impact.
Decoding the Science: How Does Ozempic Work Its Magic?
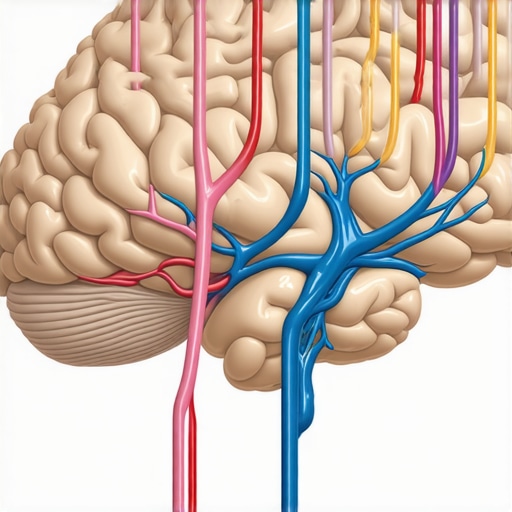
Let’s get a little nerdy for a moment. Ozempic, scientifically known as semaglutide, mimics a hormone that your body naturally produces to regulate appetite and insulin. It slows gastric emptying, making you feel full longer, and even influences brain centers to curb hunger cravings. This dual action isn’t just a quick fix — it’s a scientifically backed strategy for sustainable weight loss. According to expert research, semaglutide’s long half-life allows for steady, consistent effects, which is key for long-term benefits.
Why 2025 Is a Turning Point for Fat Loss Enthusiasts
In the past, weight loss solutions were often short-lived, leaving folks frustrated and back to square one. But with ongoing studies and real-world evidence, 2025 might just be the year when Ozempic becomes the gold standard in sustained fat management. The latest clinical trials show that users not only lose weight but also maintain their results for years, thanks to the drug’s influence on metabolic pathways. Plus, the convenience of weekly injections makes compliance a breeze.
Is This the End of Yo-Yo Diets?
It’s a provocative question, isn’t it? Could Ozempic finally put an end to the relentless cycle of losing and regaining weight? The evidence suggests yes, especially when combined with lifestyle adjustments. But let’s not forget, no magic pill exists in a vacuum; long-term success depends on a holistic approach, including diet, exercise, and ongoing medical supervision. As healthcare providers refine protocols and patient education improves, the future looks bright.
To explore how Ozempic stacks up against other GLP-1 drugs like Wegovy, check out our detailed comparison.
If you’re curious about starting your journey with physician-guided Ozempic treatments, our comprehensive guide walks you through the process step-by-step.
So, what’s your take? Are we on the brink of a new era in weight management, or is there still a long road ahead? Drop your thoughts below or share this article with friends eager to learn more about this groundbreaking shift.
Can Ozempic Truly End the Yo-Yo Diet Cycle?
As we delve deeper into the potential of Ozempic for sustainable weight management in 2025, one can’t help but wonder whether this medication might finally offer a permanent solution to the age-old yo-yo dieting phenomenon. The key lies in its ability to influence metabolic pathways and appetite regulation over the long term, supported by ongoing clinical research that highlights its role in maintaining weight loss for extended periods. However, success isn’t solely dependent on medication—comprehensive lifestyle changes, including diet, exercise, and continuous medical supervision, remain critical components for enduring results.
Are We Overestimating the Power of Pharmacotherapy Alone?
While the promise of Ozempic is compelling, experts caution against viewing it as a silver bullet. The complexity of weight regulation involves psychological, behavioral, and physiological factors that medication alone can’t fully address. For instance, recent studies emphasize the importance of integrating pharmacotherapy with behavioral therapy and nutritional counseling to optimize outcomes. This holistic approach not only enhances efficacy but also fosters healthier habits that are essential for long-term success. To explore how medical professionals are combining these strategies effectively, visit our comprehensive guide.

According to research published by scientific experts, semaglutide’s long half-life and steady pharmacokinetics underpin its success in supporting sustained weight loss, making it a cornerstone in the evolving landscape of medical weight management. The ongoing refinement of dosing protocols and patient monitoring will likely enhance its long-term effectiveness, ensuring that more individuals can achieve and maintain their ideal weight.
Interested in how you can access physician-guided Ozempic treatments? Our detailed process walks you through the steps involved. Don’t forget to share your thoughts—do you believe pharmacotherapy like Ozempic will revolutionize weight management in the next decade? Or do you see potential hurdles still to overcome? Drop a comment below or share this article with friends eager to understand the future of weight loss solutions.
Beyond the Basics: Exploring the Neuroendocrine Modulation of Appetite by Semaglutide
As we delve deeper into the mechanistic intricacies of Ozempic, or semaglutide, it becomes evident that its influence extends beyond mere gastric emptying and satiety signaling. Recent neuroscientific research indicates that GLP-1 receptor agonists modulate specific neural circuits in the hypothalamus and brainstem, which are critical for integrating metabolic signals and orchestrating appetite suppression. This neuroendocrine interplay suggests that semaglutide may recalibrate the body’s natural energy balance set points, potentially leading to more durable weight loss outcomes. A comprehensive review by Physiological Reviews underscores the complexity of these neural pathways and highlights avenues for optimizing pharmacotherapy.
What Are the Challenges in Achieving Long-term Neural Plasticity with Pharmacotherapy?
While the neuroplastic effects of GLP-1 analogs are promising, achieving sustained modifications in neural circuitry presents challenges. The brain’s inherent resilience and adaptive mechanisms may diminish the efficacy of pharmacological interventions over time. To counter this, innovative strategies such as combined neuromodulation, behavioral therapy, and personalized medicine are under investigation. For example, pairing semaglutide with targeted cognitive-behavioral approaches could reinforce neural pathways associated with satiety, increasing the likelihood of lasting change. Ongoing clinical trials are exploring these multidimensional interventions to maximize long-term success.
Interested in how emerging research is shaping future treatments? Dive into our latest studies for insights into cutting-edge approaches.
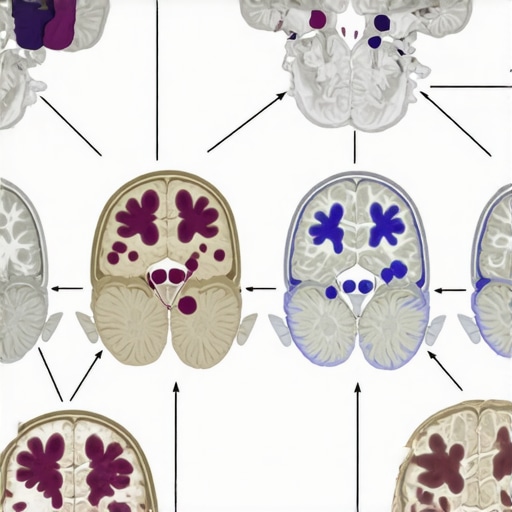
Precision Medicine and Pharmacogenomics: Tailoring Weight Loss Strategies with Semaglutide
As personalized medicine gains momentum, understanding genetic variations that influence response to GLP-1 receptor agonists becomes paramount. Pharmacogenomic research reveals that polymorphisms in genes related to GLP-1 receptor expression, insulin regulation, and neuropeptide signaling can significantly impact individual treatment outcomes. For instance, variants in the TCF7L2 gene, known for its role in glucose metabolism, may predict differential responses to semaglutide therapy. Harnessing this knowledge enables clinicians to customize weight management plans, optimizing efficacy while minimizing adverse effects. A recent meta-analysis by Nature Communications emphasizes the potential of genomic profiling in refining pharmacotherapy strategies.
How Can Clinicians Incorporate Pharmacogenomics into Routine Practice?
Integrating genetic testing into clinical workflows requires robust infrastructure and clinician education. Practical steps include establishing genetic screening protocols prior to initiating GLP-1 agonists, interpreting results within a multidisciplinary framework, and adjusting treatment plans accordingly. Furthermore, developing comprehensive guidelines and decision-support tools can facilitate this process, ensuring that personalized approaches become standard practice. As this field evolves, collaboration between geneticists, endocrinologists, and behavioral specialists will be essential for translating genomic insights into meaningful health outcomes.
To learn more about implementing precision medicine in weight management, visit our expert-guided resources.
Revolutionizing Weight Management: The Neuroendocrine Dimension of Semaglutide in 2025
As the landscape of obesity treatment evolves, experts are increasingly recognizing the importance of understanding the neuroendocrine mechanisms underpinning the efficacy of GLP-1 receptor agonists like Ozempic. Beyond its gastrointestinal effects, recent neuroscientific research reveals that semaglutide profoundly influences neural circuits responsible for appetite regulation and energy homeostasis. This paradigm shift underscores the potential to harness neuroplasticity for long-term weight management strategies, making 2025 a pivotal year in personalized obesity care.
Deciphering Neural Circuitry: How Semaglutide Recalibrates the Brain’s Hunger Signals
Emerging studies demonstrate that semaglutide modulates key hypothalamic nuclei and brainstem pathways involved in satiety and reward processing. By interacting with GLP-1 receptors in these regions, the drug can recalibrate the body’s natural energy set points, leading to sustained reductions in appetite. This neuroendocrine interplay suggests that long-term success may depend not only on pharmacological effects but also on the brain’s capacity for neuroplastic adaptation. For a detailed review of these neural pathways, consult Physiological Reviews.
Can Targeted Neuromodulation Enhance Semaglutide’s Long-Term Effects?
Addressing the challenge of maintaining neural plasticity, researchers are exploring combined approaches such as transcranial magnetic stimulation (TMS) and behavioral therapy to reinforce satiety circuits. These techniques aim to potentiate semaglutide’s effects, potentially leading to more durable weight loss outcomes. Integrating neuromodulation with pharmacotherapy represents a frontier in obesity management, promising personalized interventions tailored to individual neural responsiveness. Interested in cutting-edge strategies? Discover more at our latest clinical trials.
Understanding the neural basis of appetite regulation is crucial for advancing long-term weight management solutions. Image depicts neural pathways affected by GLP-1 receptor agonists, highlighting hypothalamic and brainstem circuits involved in satiety and reward processing.
Personalized Medicine: The Role of Pharmacogenomics in Optimizing Outcomes in 2025
Genetic variations significantly influence individual responses to semaglutide, and ongoing advancements in pharmacogenomics are paving the way for truly personalized treatment plans. Variants in genes such as TCF7L2 and GLP1R can predict responsiveness or adverse reactions, enabling clinicians to tailor therapies with greater precision. Integrating genomic profiling into routine practice not only maximizes efficacy but also minimizes the risk of side effects, aligning with the broader shift toward precision medicine in metabolic health. For practical guidance on implementing pharmacogenomics, explore our expert resources.
How Close Are We to Routine Genomic Screening for Weight Loss Therapies?
While still emerging, the integration of genetic testing into clinical workflows is rapidly advancing. Challenges such as cost, accessibility, and clinician education are being addressed through technological innovations and interdisciplinary collaborations. Future protocols may include pre-treatment genetic screening to inform drug selection, dose adjustments, and monitoring strategies. This evolution promises a new era where treatment is customized not just based on clinical parameters but also on individual genetic makeup, elevating the standard of care in obesity medicine.
Expert Insights & Advanced Considerations
1. Neuroendocrine Modulation as a Key to Sustained Weight Loss
Recent neuroscientific research highlights how semaglutide influences brain circuits responsible for appetite and energy balance, suggesting that targeting neural pathways may enhance long-term outcomes. Understanding these mechanisms allows clinicians to develop more effective, personalized interventions that leverage neuroplasticity.
2. The Role of Pharmacogenomics in Personalized Treatment
Emerging evidence indicates that genetic variations in GLP-1 receptor genes can predict individual responses to Ozempic. Incorporating pharmacogenomic profiling into clinical practice enables tailored therapies, maximizing efficacy while minimizing adverse effects, thus pushing the boundaries of precision medicine in weight management.
3. Combining Pharmacotherapy with Behavioral and Neuromodulation Techniques
Integrating medication with behavioral therapies and neuromodulation (like TMS) may potentiate neural circuit re-calibration, leading to more durable weight loss. This multidimensional approach represents the frontier of obesity treatment, emphasizing the importance of comprehensive, personalized strategies.
Curated Expert Resources
- Physiological Reviews: Offers in-depth analysis of neural pathways affected by GLP-1 receptor agonists, crucial for understanding long-term neuroendocrine effects.
- Nature Communications: Provides latest pharmacogenomic research that can inform personalized Ozempic treatment plans.
- ClinicalTrials.gov: A platform for exploring ongoing studies on neuroplasticity, neuromodulation, and combination therapies for obesity management.
- American Journal of Physiology: Features reviews on neuroendocrine mechanisms underlying appetite regulation and weight loss.
- Endocrinology & Metabolism Clinics of North America: Discusses integrating genetic profiling into routine clinical practice for obesity treatment.
Final Expert Perspective
The future of weight management with Ozempic in 2025 hinges on integrating neuroendocrine insights, pharmacogenomics, and multimodal therapies. As experts, we recognize that personalized, science-backed strategies will redefine long-term fat loss success. Engage with these resources and consider your role in advancing this evolving field—your expertise could be the key to unlocking sustained health for countless individuals.

