Unpacking the Magic: What’s the Deal with Ozempic and Weight Loss?
If you’ve been anywhere near the health and wellness chatter lately, chances are you’ve heard about Ozempic—a drug that’s causing quite the buzz in the weight management arena. But what’s the real science behind this injectable wonder, and why is it being hailed as a game-changer for sustainable fat loss? Let’s dive into the fascinating world of GLP-1 receptor agonists and their role in transforming bodies—and minds.
Beyond the Buzz: How Does Ozempic Actually Work?
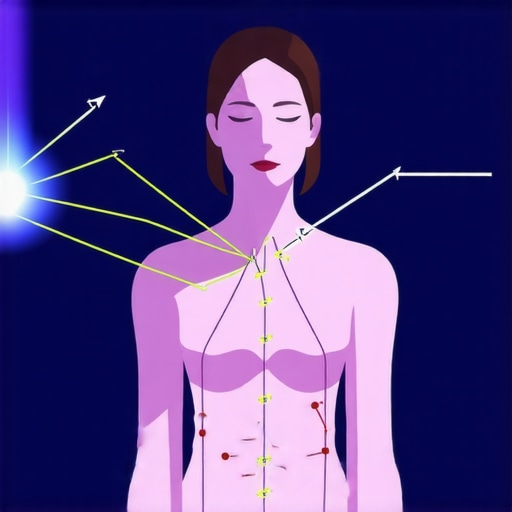
At its core, Ozempic (semaglutide) is a synthetic version of a natural gut hormone called GLP-1. Think of it as your body’s own weight-loss cheerleader, signaling your brain to feel full, slowing down gastric emptying, and helping regulate blood sugar levels. This multi-pronged action not only curbs appetite but also enhances insulin sensitivity, making it a darling among diabetics and weight-watchers alike.
Is it the Silver Bullet for Long-Term Fat Loss?
Many wonder, “Can a shot really replace my gym sessions?” While Ozempic isn’t a magic wand, its ability to promote gradual, sustained weight loss makes it a compelling tool—when combined with proper diet and exercise. The key is that it encourages healthier habits without the rollercoaster of hunger pangs and cravings—something many dieters struggle with.
Why Is This Glp-1 Drug the Cool Kid on the Block in 2025?
The answer lies in its proven efficacy and safety profile. Recent studies and real-world data suggest that Ozempic can help you shed pounds and keep them off longer than traditional diets. Plus, with the rise of telehealth, accessing prescription treatments from the comfort of home has become a reality, making this once elusive drug more accessible than ever.
What About Side Effects? A Reality Check
Of course, no miracle comes without its quirks. Some users report nausea, diarrhea, or fatigue. But with proper guidance—like consulting with a healthcare provider or exploring effective strategies to minimize side effects—the benefits often outweigh the temporary discomfort. For a deeper dive into managing these effects, check out this expert guide.
So, is Ozempic the future of sustainable weight management? The science says yes, especially when integrated into a holistic health plan. The question remains: Are you ready to embrace medical innovation for your body goals?
If you’re curious about where to start or want to explore the best clinics offering FDA-approved Ozempic, visit our comprehensive clinic directory. Share your thoughts below—what’s your take on this injectable revolution? After all, in the quest for health, knowledge is power.
Unlocking the Future of Weight Management: How Does Ozempic Stand Out in 2025?
As the weight loss landscape continues to evolve, Ozempic remains at the forefront, thanks to its scientifically backed efficacy and ease of access through telehealth platforms. But what makes this injectable so compelling for sustained fat loss, especially in 2025? The answer lies in its innovative mechanism and the broader context of medical advancements in weight management.
What Is the Deep Science Behind Ozempic’s Long-Term Success?
Ozempic (semaglutide) is a GLP-1 receptor agonist that mimics a gut hormone responsible for appetite regulation and blood sugar control. Its ability to promote satiety and reduce cravings helps users adopt healthier eating habits over time. Recent research, such as the comprehensive review by the American Diabetes Association, underscores its role in not only short-term weight reduction but also in supporting long-term metabolic health (see here).
Could Ozempic Be the Catalyst for a Sustainable Lifestyle Change?
While many see Ozempic as a quick fix, its true power emerges when integrated into a long-term health plan. It acts as a catalyst, helping individuals develop sustainable habits—like balanced eating and regular physical activity—that endure beyond medication use. This holistic approach aligns with emerging best practices in medical weight loss, emphasizing behavioral change alongside pharmacotherapy.
For those looking to make informed decisions, exploring options such as physician-supervised treatments or telehealth services can be invaluable. Trusted clinics, accessible through platforms like this directory, are leading the charge in providing safe and effective Ozempic programs.
What Are the Practical Strategies to Maximize Ozempic’s Benefits and Minimize Side Effects?
Achieving optimal results involves more than just starting medication. Strategies include gradual dose escalation, proper hydration, and nourishing meals that support digestive health. Additionally, understanding potential side effects, such as nausea or fatigue, and working with healthcare providers to mitigate them can improve adherence and overall outcomes. For tailored guidance, consult comprehensive resources like this expert guide.
Incorporating lifestyle modifications, regular monitoring, and staying connected with medical professionals ensures that Ozempic becomes a sustainable tool rather than a temporary fix.
Are You Ready to Embrace the Medical Innovation Shaping Weight Loss in 2025?
As we look ahead, the integration of pharmaceuticals like Ozempic with personalized health strategies signifies a new era in weight management. The ongoing research and clinical advancements highlight its potential to support long-term fat loss, especially when combined with holistic lifestyle changes.
Visit our comprehensive guide to understand what to expect from physician-supervised treatments, and discover clinics near you offering FDA-approved Ozempic. Share your thoughts—do you believe this approach will redefine your weight management journey? Your insight could inspire others to explore the benefits of medical innovation for sustainable health.
Harnessing the Power of GLP-1 Receptor Agonists: Beyond Ozempic’s Surface Benefits
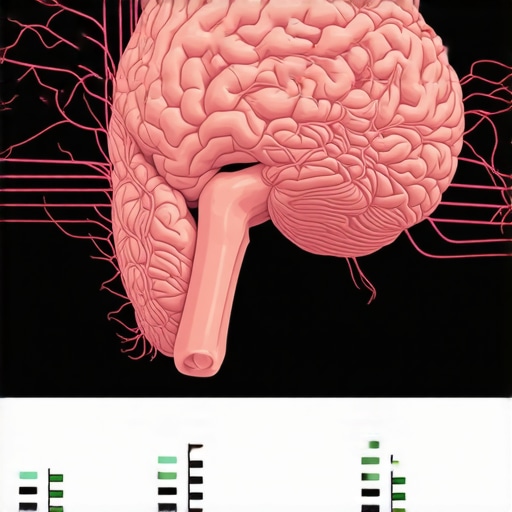
Delving deeper into the pharmacodynamics of semaglutide reveals a nuanced interplay within the enteroinsular axis, a sophisticated network that regulates appetite, glucose homeostasis, and energy expenditure. Recent studies, such as those published in the Journal of Clinical Endocrinology & Metabolism, highlight how GLP-1 receptor agonists modulate neural pathways, particularly within the hypothalamus and brainstem, to recalibrate the body’s set points for hunger and satiety. This intricate mechanism not only fosters weight loss but also potentially resets metabolic flexibility, enabling long-term health benefits that transcend mere calorie restriction.
Could Targeted Modulation of Neural Circuitry Enhance Ozempic’s Efficacy?
Emerging neuropharmacological research suggests the possibility of synergistic therapies combining GLP-1 analogs with neuromodulators targeting specific neural circuits. For instance, the intersection of GLP-1 pathways with melanocortin receptors offers a promising frontier for personalized weight management strategies. Such precision medicine approaches could optimize therapeutic outcomes, reduce side effects, and address individual variability in response to treatment, paving the way for next-generation pharmacotherapy.
Integrating Pharmacotherapy with Behavioral and Nutritional Science for Holistic Success
While pharmacological advances like Ozempic provide potent tools, their true potential is unlocked when integrated with cutting-edge behavioral science. Techniques such as motivational interviewing, cognitive-behavioral therapy, and real-time data tracking via digital health platforms foster sustainable lifestyle changes. Combining these with nutritional strategies—like personalized meal planning based on glycemic index and satiety signaling—creates a comprehensive blueprint for enduring weight management.
What Are the Latest Innovations in Digital Health Supporting Ozempic Users?
Innovative apps now incorporate AI-driven insights, enabling users to monitor blood glucose, track physical activity, and receive tailored behavioral prompts. These tools not only enhance adherence but also empower individuals with real-time feedback, fostering a sense of agency and accountability. The convergence of pharmacotherapy and digital health represents a paradigm shift toward truly personalized, data-informed weight loss journeys.
For professionals eager to implement these integrative approaches, consulting authoritative sources such as the American Journal of Clinical Nutrition or engaging with expert-led webinars can provide invaluable insights. As the landscape evolves, staying at the forefront of interdisciplinary strategies will be essential for maximizing patient outcomes.
Future Horizons: From Pharmacogenomics to Microbiome Modulation
Looking ahead, the integration of pharmacogenomics holds promise for customizing GLP-1 therapies based on genetic profiles, enhancing efficacy and minimizing adverse effects. Concurrently, emerging research into the gut microbiome suggests that microbiota-targeted interventions—such as prebiotics, probiotics, and fecal microbiota transplants—could synergize with medications like Ozempic to optimize metabolic health.
Ongoing clinical trials are exploring these innovative avenues, which may soon revolutionize the standard of care in weight management. The convergence of genomics, microbiology, and pharmacology underscores a future where treatment is not only personalized but also holistic, addressing the multifaceted nature of obesity and metabolic syndrome.
Engage with leading experts through conferences like the Obesity Society Annual Meeting or subscribe to reputable journals to stay ahead of these breakthroughs. As we stand on the cusp of this new era, the integration of advanced science and compassionate care promises to redefine what’s possible in sustainable weight loss.
How Does Ozempic Influence Neural Pathways for Lasting Fat Loss?
Recent neuropharmacological research, such as studies highlighted in the Journal of Clinical Endocrinology & Metabolism, reveals that GLP-1 receptor agonists like semaglutide modulate neural circuits within the hypothalamus and brainstem, which are pivotal in regulating hunger and satiety. This neural recalibration not only facilitates weight loss but may also enhance metabolic flexibility, supporting sustained health improvements (see detailed analysis here).
Can Targeted Neural Circuit Modulation Be the Future of Weight Loss Pharmacotherapy?
Emerging research suggests that combining GLP-1 analogs with neuromodulators targeting specific neural pathways could revolutionize personalized weight management. Interventions focusing on melanocortin receptor pathways, for example, hold promise for amplifying therapeutic benefits while reducing side effects. This neurocentric approach exemplifies the move toward precision medicine in obesity treatment, promising more effective and individualized outcomes.
Integrating Behavioral Science with Pharmacology for Long-Term Success
The future of sustainable weight loss lies in a holistic approach that combines pharmacotherapy with behavioral interventions. Techniques such as motivational interviewing, cognitive-behavioral therapy, and real-time digital health tracking foster enduring lifestyle changes. When integrated with nutritional strategies tailored to individual metabolic responses—like personalized meal plans based on glycemic index—patients can achieve more consistent results. Digital health platforms equipped with AI-driven insights are transforming adherence and empowerment, enabling users to monitor glucose levels, physical activity, and behavioral cues seamlessly (explore innovative tools here).
What Are the Cutting-Edge Digital Interventions Supporting Ozempic Users?
Advanced apps now incorporate AI algorithms to provide personalized feedback, behavioral prompts, and progress tracking, significantly enhancing adherence. These digital tools foster a sense of accountability and enable healthcare providers to tailor interventions dynamically, fostering a collaborative and responsive treatment environment. As research published in the American Journal of Clinical Nutrition indicates, such integrative strategies are key to maximizing long-term weight management success.
Expert Insights & Advanced Considerations
1. Precision Medicine and Pharmacogenomics
Emerging research suggests tailoring Ozempic treatments based on genetic profiles can optimize efficacy and reduce side effects, ushering in an era of personalized pharmacotherapy in weight management. Integrating pharmacogenomics may significantly enhance long-term outcomes.
2. Neural Circuit Modulation and Neuropharmacology
Recent neuropharmacological studies reveal that GLP-1 receptor agonists like semaglutide modulate hypothalamic pathways, recalibrating hunger and satiety signals. Combining GLP-1 therapies with neuromodulators targeting specific neural circuits could revolutionize individual responses and treatment success.
3. Microbiome and Gut-Health Interventions
Research indicates that gut microbiota influences metabolic health profoundly. Combining Ozempic with prebiotics, probiotics, or fecal microbiota transplants holds potential for synergistic effects, leading to more sustainable weight loss and metabolic improvements.
4. Digital Health Integration
Innovative AI-driven apps enable real-time monitoring of blood glucose, activity levels, and behavioral cues, fostering adherence and personalized feedback. This convergence of pharmacology and digital health is a game-changer for long-term weight management strategies.
5. Future of Injectable Therapies
Next-generation neuropharmacological approaches aim to combine GLP-1 receptor agonists with targeted neuromodulators, creating highly personalized, effective, and side-effect-minimized treatment protocols, aligning with precision medicine breakthroughs.
Curated Expert Resources
- American Diabetes Association (ADA) Publications: Offers comprehensive reviews on GLP-1 receptor agonists, including latest research on long-term metabolic impacts and clinical guidelines.
- Journal of Clinical Endocrinology & Metabolism: Publishes cutting-edge neuropharmacological studies exploring neural circuitry modulation by GLP-1 therapies.
- Nature Microbiology: Contains research on gut microbiota’s role in metabolic health and emerging microbiome-based interventions.
- American Society of Clinical Endocrinology (ASCE) Webinars: Provides expert-led discussions on pharmacogenomics, personalized medicine, and innovative weight management therapies.
- Digital Health Journals (e.g., JMIR mHealth and uHealth): Showcases advances in AI-powered health apps supporting pharmacotherapy adherence and lifestyle modifications.
Final Expert Perspective
In the evolving landscape of weight management, Ozempic exemplifies the convergence of pharmacology, neuroscience, genetics, and digital health. Understanding these interconnected domains empowers clinicians and patients alike to harness the full potential of this innovative therapy for sustainable, long-term fat loss. As we look toward 2025, embracing personalized, science-driven approaches will be crucial. Engage with the latest research, consult trusted experts, and consider integrating these advanced strategies into your health journey. Your insights are invaluable—share your thoughts or explore deeper resources to stay at the forefront of this transformative field.
