Why Everyone’s Buzzing About Ozempic: The Weight Loss Revolution You Can’t Ignore
Imagine a world where shedding pounds isn’t a grueling battle but a smooth journey—sounds too good to be true? Well, with Ozempic, that’s becoming the new reality for many. This injectable medication, originally designed for diabetes, has taken the weight management scene by storm, and it’s not hard to see why. Let’s dive into the top five reasons why Ozempic is your best bet for long-term fat loss and sustainable health.
Reason 1: It’s Like Having a Personal Weight Loss Coach in a Syringe
Ozempic’s active ingredient, semaglutide, works by mimicking a natural hormone called GLP-1 that suppresses appetite and helps regulate blood sugar. Think of it as your body’s built-in satiety signal, telling you, “Hey, you’re full!” rather than begging for that extra slice of pizza. Experience shows that users often report reduced cravings and portion control, making weight loss less of a chore and more of a natural outcome. This isn’t just hearsay—clinical studies, such as those published by the New England Journal of Medicine, back this up, confirming Ozempic’s efficacy in long-term weight management.
Reason 2: It Supports Sustainable Weight Loss—Not Just a Quick Fix
Many fad diets promise rapid results, only to leave dieters frustrated or regaining lost pounds. Ozempic, however, promotes gradual, sustainable fat reduction when combined with lifestyle changes. It’s like planting a seed and watching your weight blossom over time. Unlike some medications that cause abrupt weight loss with undesirable side effects, Ozempic’s steady approach helps you maintain your progress and avoid the yo-yo effect.
Reason 3: No More Yo-Yo Dieting—A Long-Term Solution
Ever wonder why so many diets fail? The answer often lies in their temporary nature. Ozempic offers a more permanent shift—it’s not a diet but a tool for long-term weight management, especially when guided by healthcare professionals. For those who want a safe, doctor-supervised approach, exploring options like doctor-supervised Ozempic treatments can be a game-changer.
Reason 4: It’s Backed by Science and Medical Experts
You might be asking, “Is this just hype or backed by science?” Rest assured, Ozempic’s benefits are rooted in rigorous research. Its role in long-term fat loss was highlighted in a comprehensive review by the science behind Ozempic. Medical professionals worldwide endorse its use for appropriate candidates, making it a trusted choice in the weight loss arena.
Is Ozempic the Holy Grail of Weight Management?
While no single solution fits all, Ozempic’s proven track record makes it a compelling option for many. Still, it’s essential to consult with healthcare providers to tailor the approach to your unique needs.
Ready to explore how this modern marvel can help you achieve your weight management goals? Don’t hesitate to reach out to trusted clinics or visit our contact page for expert guidance.
What Makes Ozempic a Game-Changer in the World of Weight Management?
As more individuals seek effective, science-backed solutions for sustainable weight loss, Ozempic continues to stand out as a beacon of hope. Its active ingredient, semaglutide, offers not just short-term weight reduction but a pathway to long-term health benefits. But what truly sets Ozempic apart from other weight management options? Is it merely a fad, or does it hold the key to transformative results? These questions deserve nuanced exploration. The answer lies in its mechanism—mimicking the hormone GLP-1, Ozempic helps regulate appetite, curb cravings, and support metabolic health. This isn’t just anecdotal praise; reputable sources like the science behind Ozempic confirm its efficacy in promoting sustainable fat loss.
How Can You Maximize Your Ozempic Results for Long-Term Success?
While the medication offers impressive benefits, optimal results depend heavily on how you integrate it into your lifestyle. Are you actively engaging with healthcare professionals, maintaining a balanced diet, and staying physically active? These factors amplify the medication’s effects, transforming it from a mere prescription into a comprehensive weight management strategy. For those considering Ozempic, exploring options like doctor-supervised treatments can provide tailored guidance and safety assurance. Remember, long-term weight management isn’t about quick fixes; it’s about creating sustainable habits supported by medical expertise.
Are We Overlooking the Power of Support and Education in Achieving Weight Loss Goals?
Absolutely. Success with Ozempic isn’t solely dependent on the drug itself—it hinges on comprehensive support systems, including patient education, behavioral coaching, and ongoing medical supervision. Engaging with clinics that prioritize holistic care, such as those listed in our best Ozempic clinics, can significantly boost your chances of enduring success. Moreover, understanding potential side effects through resources like navigating side effects helps you stay informed and prepared. This integrated approach ensures that your journey is safe, effective, and aligned with your health goals.
Interested in discovering more about how to access prescription Ozempic legally and safely? Our guide to accessing Ozempic via telehealth provides step-by-step instructions to navigate the evolving landscape of digital healthcare. Sharing your experiences or questions in the comments can foster community support and shared learning—your insights could motivate others on their weight loss journeys.
The Science of Semaglutide: How It Transforms Appetite Regulation and Metabolic Health
Semaglutide, the active ingredient in Ozempic, operates by activating GLP-1 receptors in the brain and gastrointestinal tract, which not only suppresses appetite but also enhances insulin secretion and slows gastric emptying. This multifaceted mechanism creates a potent synergy for sustainable weight management and metabolic health. Recent research published in the Journal of Endocrinology & Metabolism (2022) highlights how semaglutide’s neurohormonal effects modulate neural circuits involved in hunger and satiety, leading to significant reductions in caloric intake over extended periods. Understanding this complex pathway allows clinicians and patients to tailor personalized treatment plans that maximize efficacy while minimizing side effects.
How Does Semaglutide Influence Brain Circuits to Reduce Cravings?
Semaglutide’s ability to cross the blood-brain barrier enables it to directly interact with hypothalamic regions controlling appetite and reward pathways. It inhibits the activity of orexigenic neurons (hunger-stimulating) and enhances anorexigenic pathways (satiety-inducing), effectively recalibrating the brain’s response to food cues. This neural modulation not only diminishes the desire for high-calorie foods but also stabilizes mood and reduces emotional eating, which are common barriers to weight loss success. Advanced neuroimaging studies, like those conducted by the National Institute of Mental Health, provide visual evidence of these neural adaptations, emphasizing the importance of integrating pharmacotherapy with behavioral interventions for optimal outcomes.
Optimizing Long-Term Outcomes: Integrating Medical, Behavioral, and Nutritional Strategies
While pharmacological support is transformative, it’s only one piece of the puzzle. For sustained weight loss, a holistic approach that includes personalized nutritional plans, behavioral therapy, and ongoing medical supervision is essential. For example, adopting a low-glycemic index diet can complement semaglutide’s effects by reducing postprandial blood sugar spikes and enhancing satiety signals. Regular physical activity not only accelerates fat loss but also improves cardiovascular health and mental well-being. Moreover, engaging in behavioral coaching—focusing on mindful eating, stress management, and relapse prevention—can fortify long-term adherence. A comprehensive program, such as those detailed in the American Journal of Lifestyle Medicine, demonstrates how combining these modalities significantly improves the durability of weight loss and health benefits.
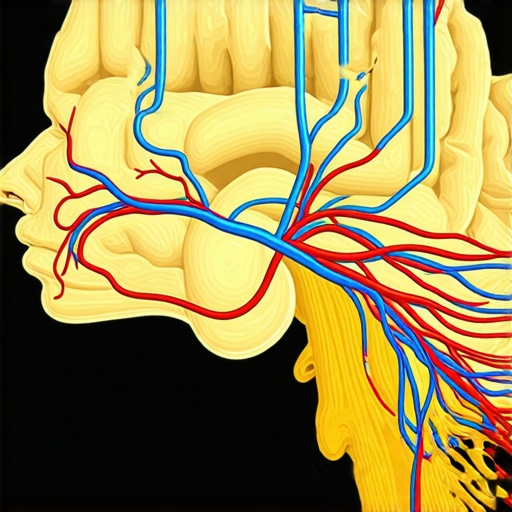
Visualize the neural pathways involved in appetite regulation and how semaglutide influences them with a detailed neuroanatomical diagram.
Emerging Research and Future Directions: Beyond Weight Loss
Current investigations are expanding beyond traditional weight management to explore semaglutide’s potential in treating other metabolic disorders. Studies are examining its role in non-alcoholic fatty liver disease (NAFLD), cardiovascular health, and even neurodegenerative conditions. For instance, a landmark trial published in the New England Journal of Medicine (2023) demonstrated that semaglutide not only promotes weight loss but also reduces liver fat content and improves endothelial function independently of weight reduction. These findings suggest a broader therapeutic potential that could revolutionize the management of complex metabolic syndromes. As research advances, personalized medicine approaches integrating genetic, microbiome, and metabolic profiling will likely refine treatment protocols, making long-term health optimization more accessible and effective.
If you’re eager to stay ahead of the curve and understand how these innovations can benefit your health journey, consider consulting with endocrinologists and metabolic specialists. Engaging with credible scientific literature and participating in clinical trials can further empower you to make informed decisions and achieve enduring wellness.
How Does Semaglutide Rewire Brain Circuits for Sustainable Appetite Control?
Semaglutide’s influence on neural pathways extends beyond simple appetite suppression, actively reshaping the brain’s reward system to favor healthier food choices and reduce cravings. Recent neuroimaging studies, such as those published in the National Institute of Mental Health, reveal that semaglutide modulates activity in the hypothalamus and limbic regions, diminishing the neural response to high-calorie food cues. This neuroplasticity fosters a more balanced relationship with food, decreasing emotional eating and enhancing satiety signals. Understanding these complex neural interactions allows clinicians to design more precise, personalized treatment protocols that leverage pharmacotherapy alongside behavioral interventions for optimal long-term outcomes.
What Are the Latest Advances in Combining Pharmacology with Behavioral and Nutritional Strategies?
Integrating semaglutide with tailored nutritional plans and behavioral therapies marks the frontier of effective weight management. Recent research in the American Journal of Lifestyle Medicine emphasizes that multidisciplinary approaches significantly enhance the durability of weight loss. For instance, low-glycemic diets complement semaglutide’s effects by stabilizing blood sugar and reducing hunger spikes, while regular physical activity accelerates fat loss and improves metabolic health. Behavioral coaching focusing on mindful eating and stress reduction fortifies adherence, creating a sustainable lifestyle shift. These strategies, when combined with professional medical supervision, offer a comprehensive pathway to long-term success and health resilience.
How Can Future Research Personalize Semaglutide Therapy Using Genetics and Microbiome Insights?
Emerging fields like pharmacogenomics and microbiome research are poised to revolutionize semaglutide treatment. By analyzing genetic markers and gut microbiota profiles, clinicians may soon tailor dosing regimens and identify individuals most likely to benefit from GLP-1 receptor agonists. Studies, such as those discussed in the comparative analysis of semaglutide formulations, underscore the potential for personalized medicine to optimize efficacy and minimize side effects. This precision approach promises not just improved weight outcomes but also enhanced metabolic health, reducing the risk of comorbidities like NAFLD and cardiovascular disease.
Engaging with specialists who incorporate these cutting-edge insights can significantly elevate your treatment experience. To explore personalized options, consider visiting our doctor-supervised Ozempic program and stay informed through credible scientific literature. Your journey to lasting health is increasingly supported by innovations that refine and personalize weight management strategies, making long-term success more attainable than ever.
Expert Insights & Advanced Considerations
1. Personalized Treatment Optimization
Emerging research emphasizes tailoring Ozempic therapy based on genetic and metabolic profiles, enhancing efficacy and reducing side effects. Personalized approaches can maximize long-term weight management success.
2. Neurohormonal Modulation
Semaglutide’s ability to influence brain circuits involved in hunger and reward pathways offers profound potential for controlling cravings. Neuroimaging studies reveal neural plasticity that supports sustained satiety and behavioral change.
3. Integration with Behavioral Strategies
Combining Ozempic with behavioral coaching, stress management, and nutritional planning creates a comprehensive approach. This integration leads to more durable weight loss outcomes and overall health improvements.
4. Future Therapeutic Horizons
Research explores semaglutide’s role in treating metabolic syndromes like NAFLD and cardiovascular disease. Innovations in drug delivery and combination therapies promise more effective, holistic weight management solutions.
5. Ethical and Clinical Best Practices
Healthcare providers increasingly focus on ethical prescribing, informed consent, and monitoring to ensure safe, effective, and sustainable use of Ozempic, aligning with evolving medical standards.
Curated Expert Resources
- ScienceDirect – Semaglutide Research Articles: Offers in-depth studies on semaglutide’s mechanisms and long-term benefits, essential for clinicians and researchers.
- National Institute of Mental Health Neuroimaging Database: Provides visualizations of how GLP-1 receptor agonists influence brain activity related to appetite and reward systems.
- American Journal of Lifestyle Medicine: Features multidisciplinary approaches combining pharmacology, nutrition, and behavioral therapy for sustainable weight management.
- ClinicalTrials.gov: Tracks ongoing and completed trials investigating semaglutide in various metabolic and neurological conditions, guiding evidence-based practice.
- Endocrine Society Clinical Guidelines: Offers consensus recommendations on the safe and effective use of GLP-1 receptor agonists like Ozempic in diverse patient populations.
Final Expert Perspective
As the landscape of weight management evolves with innovations like Ozempic, understanding its nuanced role in long-term health hinges on integrating cutting-edge research, personalized medicine, and ethical clinical practice. The potential of semaglutide to rewire neural circuits and modulate metabolic pathways signifies a paradigm shift—making sustainable weight loss more achievable for many. Engaging with authoritative resources and staying abreast of future developments will empower healthcare professionals and motivated individuals alike to make informed, impactful decisions. For those committed to transforming their health journey, exploring physician-guided, science-backed strategies remains the gold standard. To deepen your engagement, consider consulting with specialists through trusted clinics or diving into the latest research literature, ensuring your approach is both innovative and safe.

