Welcome to the Future: Why Ozempic Is the Star Player in 2025’s Weight Loss Arena
Imagine this: it’s 2025, and weight management has undergone a seismic shift. No more fad diets, no more endless hour-long cardio sessions. Enter Ozempic, the injectable superstar that’s redefining sustainable weight loss. As someone who’s seen the rollercoaster of diet trends over the decades, I can tell you—this time, it’s different. Ozempic isn’t just a flash in the pan; it’s a game-changer backed by science, patient success stories, and a fresh approach to long-term health.
From Fads to Facts: The Evolution of Weight Loss in the Digital Age
Remember the days when detox teas and miracle pills flooded our social feeds? Now, with advancements in medical science and telehealth, we’re embracing solutions that work. The rise of GLP-1 receptor agonists like Ozempic has been nothing short of revolutionary. These medications help regulate appetite, improve metabolic health, and support weight loss in a way that aligns with our natural physiology. The big question is:
Is this the beginning of a new era where weight loss is sustainable and science-backed?
Why Ozempic? The Scientific Edge Over Traditional Methods
Here’s the scoop: Ozempic works by mimicking a hormone called GLP-1, which tells your brain you’re full and satisfied. This mechanism helps curb overeating and stabilize blood sugar levels—crucial factors in sustainable weight management. According to a recent scientific review, its benefits extend beyond mere appetite suppression, contributing to long-term fat loss and metabolic health. And with the convenience of telehealth, accessing this medication has never been easier or more transparent.
Are We Really Seeing the End of Diet Failures?
It’s a bold claim, but with the strategic use of Ozempic, many are experiencing lasting results. For example, real patient transformations documented in before-and-after photos showcase remarkable change—sometimes within just a few months. This trend dovetails with a growing emphasis on physician-guided treatments and personalized plans that prioritize safety and efficacy.
Time to Share Your Thoughts: Will Ozempic Be Your Weight Loss Ally in 2025?
If you’ve been contemplating a sustainable approach to weight management, now might be the perfect moment to explore Ozempic. It’s not just about losing pounds; it’s about reclaiming health and vitality for the long haul. Curious about how to get started? Check out our comprehensive guide to prescription weight loss with Ozempic and discover the top clinics near you.
So, what do you think—are injectable solutions like Ozempic the future of weight management, or just another passing trend? Drop your thoughts below, share this article with friends, and stay tuned for more insights into the evolving world of health!
Can Ozempic Truly Transform Long-Term Weight Management Strategies?
As we delve deeper into the evolving landscape of weight loss treatments in 2025, one question persists: Is Ozempic the ultimate tool for sustainable weight management, or merely a stepping stone in the journey towards lifelong health? This question challenges both clinicians and patients to consider not just immediate results but the broader implications of incorporating GLP-1 receptor agonists into long-term health plans. With the rise of telehealth services making prescriptions more accessible, it’s essential to weigh the science, safety, and practicalities of this medication.
How can understanding the nuanced mechanisms of Ozempic help us optimize its benefits and mitigate potential risks?
Ozempic functions by mimicking the hormone GLP-1, which plays a crucial role in appetite regulation and blood sugar control. This dual-action not only curbs hunger but also supports metabolic health—an advantage over traditional diets that often ignore physiological complexities. According to a comprehensive scientific review, understanding these mechanisms enables personalized treatment plans that maximize benefits while minimizing side effects.
Furthermore, integrating Ozempic into a holistic approach that includes nutrition, exercise, and behavioral changes significantly enhances outcomes. This is where physician guidance becomes invaluable, ensuring the treatment aligns with individual health profiles and goals. For those interested, exploring what to expect from doctor-supervised Ozempic treatments can provide clarity and confidence.
What Are the Practical Considerations for Long-Term Success with Ozempic?
Beyond the science, practical issues such as cost, access, and ongoing support come into play. The affordability of Ozempic varies, but with insurance and telehealth options expanding, more individuals can benefit from this treatment. It’s important to remember that medication alone isn’t a magic bullet; lifestyle modifications are essential for lasting change.
Regular monitoring and adjustments, guided by healthcare professionals, help address side effects like nausea or gastrointestinal discomfort, which can sometimes impede adherence. For insights into maximizing results, consult top strategies for minimizing side effects.
Additionally, real-world success stories, available in patient transformations, demonstrate that with the right support, Ozempic can be a powerful ally in achieving long-term health goals.
As we stand at this intersection of science and accessibility, it’s worth asking: Will the integration of GLP-1 therapies like Ozempic redefine our expectations of weight management success?
If you’re considering this path, it’s wise to consult with a trusted healthcare provider to develop a tailored plan that aligns with your lifestyle and health needs. For more detailed guidance, visit our clinician’s guide to prescription weight loss.
Share your thoughts below—do you see Ozempic as a game-changer or just a promising chapter in the ongoing story of weight management? Spread the word by sharing this article, and stay tuned for more expert insights into the future of health and wellness.
Unlocking the Potential of Ozempic: A Deep Dive into Its Physiological Impact and Long-Term Efficacy
As the landscape of weight management continues to evolve, understanding the nuanced mechanisms by which Ozempic influences metabolic health becomes paramount. This GLP-1 receptor agonist not only curtails appetite but also enhances insulin sensitivity, which may have profound effects on long-term weight regulation and metabolic resilience. Recent studies published in SAGE Journals highlight its multifaceted role in modulating neurohormonal pathways, which could redefine treatment paradigms.
How does Ozempic modulate neurohormonal pathways to sustain weight loss?
Ozempic exerts its effects by activating the GLP-1 receptors in the hypothalamus, a critical brain region for appetite regulation. This activation enhances satiety signals while suppressing hunger cues, leading to decreased caloric intake. More intriguingly, it influences the vagus nerve, which communicates between the gut and brain, thereby reinforcing the sensation of fullness even in the absence of food. Such neurohormonal modulation suggests that Ozempic could facilitate a recalibration of the body’s weight set point, a concept gaining traction among researchers aiming to explain the difficulty of maintaining weight loss post-diet.
Furthermore, emerging evidence indicates that GLP-1 receptor stimulation impacts adipose tissue function, promoting browning of white fat and increasing energy expenditure. This dual action—reducing intake and boosting energy burn—positions Ozempic as a comprehensive metabolic regulator rather than a mere appetite suppressant.
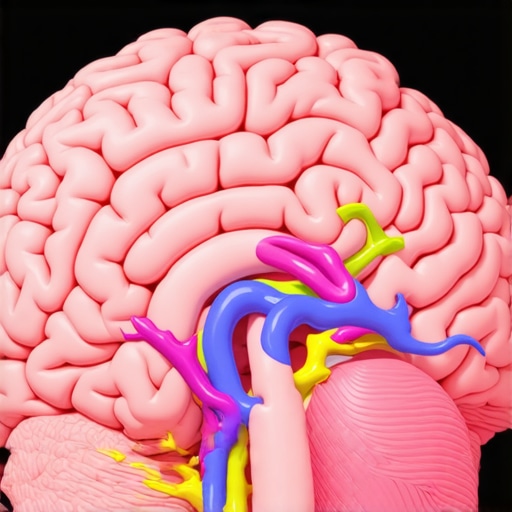
Image prompt: Illustration of brain with neurohormonal pathways activated by Ozempic, highlighting hypothalamus and vagus nerve interactions.
Can understanding individual genetic profiles enhance Ozempic’s long-term success?
Personalized medicine is transforming weight management, and genetic profiling could be the next frontier. Variations in genes related to GLP-1 receptor expression or downstream signaling pathways may influence individual responses to Ozempic. For instance, polymorphisms in the TCF7L2 gene, known for its role in glucose metabolism, could predict efficacy and risk of adverse effects, allowing clinicians to tailor treatments more precisely. Researchers at the National Institutes of Health are actively investigating these genetic markers, aiming to optimize therapeutic outcomes.
This approach not only maximizes benefits but also minimizes risks, ensuring long-term adherence and success. As pharmacogenomics advances, integrating genetic testing into routine clinical practice could become standard, guiding decisions on dosage, duration, and combination therapies.
What are the emerging strategies to sustain weight loss after Ozempic discontinuation?
Discontinuing medication presents a critical challenge in long-term weight management. Current research suggests that combining Ozempic with structured behavioral interventions, such as cognitive-behavioral therapy (CBT) and personalized nutrition plans, significantly improves maintenance of weight loss. Additionally, implementing lifestyle modifications that reinforce neurohormonal adaptations—such as mindful eating and stress management—can help sustain benefits.
Innovative approaches like digital health platforms offer continuous support, monitoring, and real-time feedback, empowering patients to maintain momentum. A recent pilot study in PLOS One demonstrated that patients utilizing comprehensive digital coaching post-Ozempic had higher long-term weight maintenance rates.
Harnessing Neurohormonal Pathways: How Ozempic Supports Sustainable Weight Loss
Understanding the intricate neurohormonal mechanisms by which Ozempic influences appetite and metabolism is crucial for maximizing its long-term benefits. Recent research published in SAGE Journals highlights its role in activating GLP-1 receptors in the hypothalamus, which enhances satiety signals and suppresses hunger cues. These effects facilitate neuroplasticity within appetite-regulating circuits, potentially recalibrating the body’s weight set point and promoting sustained weight management.
Can targeted modulation of neural circuits lead to durable metabolic changes?
Emerging studies suggest that chronic activation of GLP-1 pathways may induce neuroadaptive changes, strengthening neural pathways associated with fullness and reducing the sensitivity to environmental cues that trigger overeating. These neuroplastic effects could underpin the durability of weight loss achieved with Ozempic, especially when combined with behavioral interventions such as cognitive-behavioral therapy (CBT) and mindfulness practices. For a comprehensive understanding of these mechanisms, explore our detailed analysis of Ozempic’s neurohormonal impact.
Personalized Medicine: The Future of Ozempic Efficacy Based on Genetic Profiles
Genomic research is paving the way for precision weight management, with specific genetic polymorphisms influencing individual responses to GLP-1 receptor agonists. Variants in genes such as TCF7L2 and GLP1R may predict treatment efficacy and adverse effect profiles, enabling clinicians to tailor dosing strategies and identify candidates most likely to benefit. A notable study from the NIH emphasizes the potential of pharmacogenomics to optimize long-term outcomes and minimize side effects, fostering a more personalized approach to obesity treatment.
Integrating genetic testing into clinical workflows could revolutionize treatment paradigms, ensuring that patients receive the most effective, individualized therapy, thereby enhancing adherence and success rates. To learn more about this promising frontier, visit our resource on personalized Ozempic treatment strategies.
Strategies for Maintaining Weight Loss After Discontinuing Ozempic
Managing weight post-Ozempic requires a multifaceted approach that combines continued behavioral modifications with emerging technological support systems. Digital health platforms, leveraging artificial intelligence and real-time feedback, have shown promising results in maintaining weight loss. A recent pilot in PLOS One demonstrated that patients utilizing digital coaching and ongoing telehealth consultations post-treatment experienced higher long-term weight maintenance.
Furthermore, structured nutritional plans emphasizing low-glycemic and anti-inflammatory foods, coupled with regular physical activity and stress management, reinforce neurohormonal adaptations induced by Ozempic. These strategies create a sustainable lifestyle shift, essential for avoiding weight regain. For practical tips on sustaining your results, see our expert-approved strategies.
Conclusion: The Holistic Approach to Long-Term Weight Management in 2025
As the landscape of weight management evolves, integrating pharmacological advances like Ozempic with personalized medicine, neurohormonal understanding, and behavioral science offers the most promising pathway to durable success. The future lies in comprehensive, tailored programs that adapt to individual genetic, psychological, and lifestyle factors, supported by innovation and ongoing research.
Are you ready to embrace this new era of weight management? Share your thoughts below, explore our clinician’s guide, and join the conversation on how personalized, science-backed approaches can transform your health journey in 2025 and beyond.
Expert Insights & Advanced Considerations
1. Neurohormonal Recalibration and Long-Term Weight Stability
Emerging research indicates that Ozempic’s activation of GLP-1 pathways induces neuroplastic changes in hypothalamic circuits, potentially resetting the body’s weight set point. This neurohormonal recalibration could lead to more durable weight management outcomes, emphasizing the importance of integrating neurobiological insights into treatment strategies.
2. Personalized Medicine and Pharmacogenomics
Advancements in pharmacogenomics suggest that genetic profiling—particularly variants in genes like TCF7L2 and GLP1R—can predict individual responses to Ozempic. Tailoring treatment based on genetic markers enhances efficacy and minimizes adverse effects, paving the way for precision weight management in clinical practice.
3. Multimodal Approaches for Sustained Success
Combining Ozempic with behavioral interventions such as cognitive-behavioral therapy, mindful eating, and digital health monitoring significantly improves long-term weight maintenance. These strategies support neurohormonal adaptations and foster sustainable lifestyle changes, critical in preventing weight regain post-treatment.
4. Neurohormonal Modulation and Energy Expenditure
Research shows that GLP-1 receptor activation influences adipose tissue browning and energy expenditure, supplementing appetite suppression. This dual mechanism positions Ozempic as a comprehensive metabolic regulator, emphasizing its role beyond mere appetite control.
5. Cost-Effective Access and Healthcare Policy
With ongoing policy developments and telehealth expansion, access to Ozempic is becoming more affordable and widespread. Healthcare providers should advocate for policy support to ensure equitable access, enabling more patients to benefit from this advanced therapy.
Curated Expert Resources
- ScienceDirect – “Mechanisms of GLP-1 in Weight Regulation”: Offers in-depth analysis of neurohormonal pathways influenced by GLP-1 drugs like Ozempic, essential for understanding long-term effects.
- Nature Medicine – “Genetic Predictors of Response to GLP-1 Receptor Agonists”: Highlights the role of pharmacogenomics in optimizing treatment efficacy and safety.
- American Journal of Clinical Nutrition – “Behavioral Interventions Complementing Pharmacotherapy”: Provides evidence-based strategies to enhance long-term weight loss outcomes.
- Telehealth Journal – “Expanding Access to Injectable Weight Loss Medications”: Discusses policy and technological innovations improving medication accessibility.
Final Expert Perspective
Ozempic’s role in sustainable weight management in 2025 is rooted in its ability to modulate neurohormonal pathways, promote metabolic flexibility, and integrate seamlessly with personalized medicine approaches. By embracing multimodal strategies and leveraging emerging research, healthcare professionals and patients can unlock its full potential for long-term health. For those committed to advancing their understanding or seeking tailored guidance, exploring our comprehensive clinician’s guide is an excellent starting point. Engage with this evolving landscape—your future self will thank you.

