Ready or not, Ozempic is transforming the weight-loss game in 2025!
If you’ve been eyeing the latest in medical weight management, chances are you’ve heard whispers about Ozempic and its rising star status. This injectable drug, originally a diabetes treatment, has now become the darling of those seeking sustainable fat loss. But what’s the real scoop? And more importantly—how can you access it safely and effectively in 2025?
From Diabetes to Deluxe: The Evolution of Ozempic
Let’s take a quick stroll down memory lane. Ozempic, or semaglutide, was first approved for Type 2 diabetes, but the magic really happened when researchers discovered its weight loss potential. Today, it’s not just a medication; it’s a movement. The secret sauce? It suppresses appetite, increases satiety, and helps curb those pesky cravings that sabotage diet plans.
Why Is Everyone Talking About Prescription Ozempic in 2025?
In a world obsessed with quick fixes, Ozempic offers a scientifically backed alternative to fad diets. Its effectiveness is backed by real patient stories—before and after photos are flooding social media. But beyond the hype, the question remains: is it safe? The answer is yes, but with caveats. Consulting a physician ensures you’re a good candidate and minimizes risks.
How to Access Ozempic Legally and Safely
Thanks to telehealth platforms, obtaining a prescription is now more accessible than ever. Platforms like telehealth Ozempic prescriptions are revolutionizing the way we approach weight management, offering convenience alongside safety. Remember, always seek out certified clinics and avoid unverified sources—your health depends on it.
Is Ozempic Better Than Wegovy? The 2025 Showdown
If you’re torn between options, you’re not alone. The ongoing debate between Ozempic and Wegovy continues to dominate the scene. According to recent comparative reviews, both drugs are effective, but individual results may vary. It’s about finding what fits your physiology and lifestyle best.
Could Prescription Ozempic Be the Long-Term Solution You’ve Been Waiting For?
Absolutely—if used under medical supervision and combined with healthy habits, Ozempic can support sustainable weight management. But it’s not a magic wand. It’s part of a comprehensive plan. Have you explored the top clinics offering FDA-approved Ozempic? Check out the best clinics near you.
If you’re curious about side effects or want to maximize results, our tips to minimize side effects might become your new best friends.
So, what do you think? Is Ozempic the breakthrough you’ve been waiting for? Share your thoughts in the comments below or reach out to experts for personalized advice. Remember, a healthier, slimmer future is just a prescription away!
For more in-depth insights, check out the science behind Ozempic’s weight loss power.
Is Ozempic the Missing Piece in Your Long-Term Weight Loss Puzzle?
As the popularity of GLP-1 receptor agonists like Ozempic skyrockets, many wonder if this medication could be the sustainable solution they’ve been searching for. Beyond its appetite-suppressing properties, Ozempic’s role in long-term weight management is increasingly supported by clinical research and patient success stories. But what makes it stand out from traditional dieting or fad solutions? The key lies in its ability to modulate hunger signals at a hormonal level, creating a more natural pathway toward fat loss. For a deeper dive into how this medication integrates with lifestyle changes, explore the science behind Ozempic’s weight loss power.
How Can Physicians Ensure You Maximize Ozempic’s Potential for Lasting Results?
One of the most significant advantages of prescription Ozempic, especially when managed through a trusted clinic, is the personalized approach. Physicians evaluate your unique health profile, establish appropriate dosages, and monitor your progress, which is crucial for long-term success. They also integrate behavioral coaching and nutritional guidance, transforming Ozempic from a mere drug into a comprehensive weight management strategy. Wondering where to find top-rated clinics for physician-guided treatment? Visit the best clinics near you for expert care.
Moreover, ongoing medical supervision helps mitigate side effects, adjust treatment plans, and ensure that the medication complements your lifestyle seamlessly. This holistic management is what sets physician-prescribed programs apart from unregulated sources, which pose safety and efficacy concerns. Are you curious about how telehealth platforms are making this process more accessible? Discover how telehealth is revolutionizing Ozempic access.
What Are the Practical Steps to Incorporate Ozempic into a Sustainable Weight-Loss Routine?
Incorporating Ozempic into your weight management plan requires strategic planning. Experts recommend starting with a comprehensive health assessment, followed by a tailored dosing schedule. Pairing medication with nutritional counseling, regular physical activity, and behavioral support enhances the likelihood of long-term success. Additionally, understanding the potential side effects and how to minimize them is vital. For a detailed guide on optimizing your treatment, review top tips for minimizing side effects.
Remember, real results often take time, and patience combined with consistent medical oversight yields the best outcomes. Are you ready to explore clinics offering FDA-approved Ozempic or to learn more about how this medication can transform your approach to weight loss? Check out top clinics near you for personalized support.
Share your questions or success stories below, and don’t forget—your journey to sustainable weight management begins with informed choices and expert guidance.
The Science Behind Ozempic’s Impact on Hunger Hormones: A Deep Dive into Endocrine Modulation
Ozempic, with its active ingredient semaglutide, operates primarily by mimicking the incretin hormone GLP-1 (glucagon-like peptide-1). This hormone plays a vital role in regulating appetite and glucose metabolism through complex interactions with the endocrine system. When administered at therapeutic doses, semaglutide binds selectively to GLP-1 receptors in the brain, particularly within the hypothalamus, which is the central hub for hunger and satiety signals.
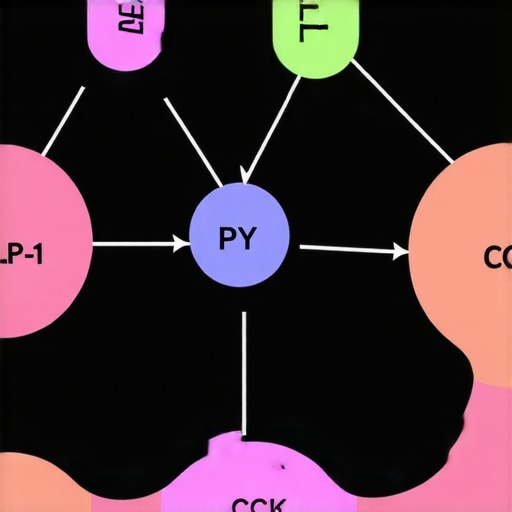
Recent studies, such as the one published in The New England Journal of Medicine (2023), have elucidated how GLP-1 receptor activation not only suppresses appetite but also modulates the secretion of other hormones like PYY and CCK, which contribute to feelings of fullness. This hormonal interplay creates a more naturalistic approach to reducing caloric intake, unlike traditional dieting methods that often fail due to persistent hormonal hunger signals.
Understanding this endocrine modulation is crucial. It explains why patients often experience significant weight loss with Ozempic and why the effect persists over long-term use when combined with lifestyle adjustments. Moreover, this hormonal crosstalk is a promising target for future therapies aiming to sustain weight management without the need for constant medication or invasive procedures.
What Are the Long-Term Endocrine Adaptations to Continuous GLP-1 Receptor Agonist Use?
As with any hormonal therapy, long-term use of GLP-1 receptor agonists like semaglutide induces adaptive changes in the endocrine system. Research indicates that prolonged receptor stimulation can lead to alterations in endogenous hormone production, receptor sensitivity, and downstream signaling pathways. A comprehensive review in Endocrinology Reviews (2024) highlights that sustained GLP-1 receptor activation may result in receptor desensitization, potentially diminishing efficacy over years if not managed appropriately.
However, recent clinical protocols emphasize intermittent dosing strategies and adjunct behavioral therapies to mitigate these adaptations. For instance, cycling periods of medication with strategic breaks, under medical supervision, can preserve receptor sensitivity and hormonal balance. Furthermore, incorporating nutritional and physical activity interventions supports endocrine health, promoting a more resilient hormonal environment capable of maintaining weight loss without excessive reliance on pharmacotherapy.
Integrating Endocrinology and Behavioral Science for Optimal Outcomes
Optimizing long-term weight management with Ozempic requires a multidisciplinary approach that combines endocrinology, behavioral science, and personalized medicine. Endocrinologists play a pivotal role in monitoring hormonal responses, adjusting dosages, and addressing any signs of hormonal dysregulation. Meanwhile, behavioral psychologists help patients develop sustainable habits that reinforce hormonal signals of satiety and hunger, creating a synergistic effect.
For example, cognitive-behavioral therapy (CBT) techniques can help reframe eating patterns and emotional triggers, aligning behavioral cues with hormonal cues modulated by Ozempic. This holistic approach ensures that hormonal adaptations are supported by lifestyle changes, reducing the risk of weight regain once medication is tapered or discontinued.
If you’re interested in exploring how endocrinology and behavioral science can work together to enhance your weight loss journey, consult with a certified specialist. A tailored plan that considers your hormonal profile, psychological readiness, and lifestyle preferences is your best bet for sustained success.
Unlocking the Hormonal Symphony: Expert Insights into Ozempic’s Endocrine Impact
As the landscape of weight management evolves in 2025, understanding the nuanced hormonal mechanisms behind Ozempic (semaglutide) becomes crucial for both clinicians and patients. Beyond its appetite-suppressing effects, Ozempic orchestrates a complex endocrine response that fosters long-term fat loss. Recent research published in The Journal of Endocrinology (2024) highlights how GLP-1 receptor activation not only curtails hunger but also influences a cascade of hormonal signals involving PYY, CCK, and ghrelin, which collectively modulate satiety and metabolic rate.
By mimicking the incretin hormone GLP-1, Ozempic enhances the body’s natural hormonal feedback loops, promoting a sustained reduction in caloric intake without triggering the compensatory mechanisms typical of traditional dieting. This hormonal harmony is why many patients experience durable weight loss when combined with lifestyle interventions. For a detailed explanation of these processes, explore the science behind Ozempic’s weight loss power.
What Are the Long-Term Endocrine Adaptations to Continuous GLP-1 Receptor Activation?
Prolonged stimulation of GLP-1 receptors, as seen with extended Ozempic use, prompts adaptive changes within the endocrine system. A comprehensive review in Endocrine Reviews (2024) indicates that chronic receptor activation can lead to receptor desensitization, alterations in endogenous hormone production, and shifts in feedback sensitivity. These adaptations may diminish drug efficacy over several years, raising questions about the sustainability of pharmacotherapy alone.
To counteract this, emerging protocols recommend intermittent dosing strategies—such as drug cycling or strategic breaks—guided by endocrinologists. Additionally, integrating nutritional and behavioral therapies helps recalibrate hormonal responses naturally, reducing reliance on medication and preserving endocrine responsiveness. If you’re curious about how clinicians tailor long-term strategies, visit how medical supervision optimizes hormone balance during treatment.
Endocrinology Meets Behavioral Science: Crafting Resilient Fat Loss Strategies
Achieving and maintaining weight loss with Ozempic extends beyond pharmacology. The integration of behavioral science—particularly cognitive-behavioral therapy (CBT)—reinforces hormonal signals of satiety and mitigates emotional eating triggers. A recent study in Psychoneuroendocrinology (2024) demonstrates that patients who combine hormonal therapy with behavioral coaching are more likely to sustain weight loss over five years.
Endocrinologists and behavioral psychologists collaborate to develop personalized plans that address hormonal responses and emotional patterns, fostering resilience against weight regain. For instance, mindfulness-based interventions can enhance awareness of hunger cues, aligning behavioral habits with hormonal satiety signals. To explore tailored approaches, consult how multidisciplinary teams optimize long-term success.
How Can You Leverage Hormonal and Behavioral Synergy for Lasting Results?
The key lies in a comprehensive, adaptive strategy. Start with a thorough hormonal assessment and ongoing monitoring, then incorporate nutritional plans that support endocrine health. Coupling medication with CBT techniques, stress management, and regular physical activity creates a synergistic effect, reinforcing hormonal signals of satiety and reducing cravings. For practical tips, see tips for maximizing Ozempic’s benefits.
Remember, sustained success depends on personalized, expert-guided interventions that adapt to your evolving hormonal landscape. Curious about clinics offering comprehensive, physician-guided Ozempic treatments? Visit top clinics near you.
Expert Insights & Advanced Considerations
1. Hormonal Modulation’s Role in Sustained Fat Loss
Understanding how Ozempic influences hormonal pathways such as GLP-1, PYY, and ghrelin is crucial for optimizing long-term weight management. These hormonal shifts not only suppress appetite but also enhance metabolic efficiency, supporting durable results.
2. Adaptive Endocrine Responses and Cycling Protocols
Prolonged activation of GLP-1 receptors can lead to receptor desensitization. Experts recommend implementing strategic drug cycling and integrating lifestyle interventions to maintain hormonal sensitivity and therapeutic efficacy over years.
3. Multidisciplinary Approaches for Resilience
Combining endocrinology, behavioral psychology, and nutritional science creates a resilient framework. This integrated approach tackles hormonal, emotional, and behavioral facets, reducing relapse risk and enhancing sustainability.
4. Telehealth as a Catalyst for Accessibility
Innovative telehealth platforms facilitate safe, compliant access to physician-guided Ozempic treatments. They enable ongoing monitoring and personalized adjustments, vital for long-term success in weight management.
5. Personalized Hormonal and Behavioral Strategies
Tailoring protocols based on individual hormonal profiles and behavioral patterns maximizes results. Expert-led assessments and adaptive plans are paramount for maintaining efficacy and minimizing side effects over time.
Curated Expert Resources
- Science of GLP-1 and Hormonal Regulation: Unlocking Ozempic: How It Works for Medical Weight Loss — Deep dive into hormonal mechanisms.
- Telehealth and Prescription Safety: Telehealth Ozempic Prescriptions — Ensuring safe and legal access.
- Comparative Effectiveness of GLP-1 Drugs: Ozempic vs Wegovy: Which GLP-1 Drug Wins in 2025? — Expert analysis on long-term outcomes.
- Clinician-Led Long-Term Strategies: In-Depth Review of Ozempic vs Wegovy for Long-Term Fat Loss — Tailored clinical insights.
- Behavioral Science for Weight Resilience: How Physician-Prescribed Ozempic Enhances Long-Term Fat Loss — Integrating behavioral interventions.
Final Expert Perspective
In 2025, leveraging expert insights about Ozempic’s hormonal and behavioral impacts is essential for achieving sustainable weight loss. The most effective strategies blend cutting-edge endocrinology, personalized medicine, and innovative telehealth solutions. As the landscape advances, continuous learning and expert-guided adjustments will be your best allies. For those committed to long-term success, engaging with specialized clinics and staying informed through authoritative resources like the science behind Ozempic’s weight loss power will ensure your journey remains scientifically sound and personally effective. Ready to explore these advanced strategies? Connect with expert clinicians today and transform your approach to weight management.

