Welcome to the Future of Weight Loss: Telehealth & Ozempic in 2025
Imagine a world where getting your Ozempic prescription is as simple as a few clicks, and you can do it safely with trusted telehealth services. Well, in 2025, that world is not just a dream—it’s a reality! As a columnist who’s followed the evolution of medical tech, I’ve seen how telemedicine has revolutionized weight management, making safe, doctor-supervised Ozempic treatments more accessible than ever.
Why Telehealth Is the Game-Changer for Ozempic Access
Gone are the days when you had to schedule in-person visits, endure long waits, or worry about counterfeit prescriptions. Today, reputable telehealth providers ensure you receive authentic medication under proper medical supervision. This shift not only enhances safety but also empowers individuals to take control of their weight loss journeys with confidence.
Picking the Right Telehealth Service: More Than Just Convenience
Not all telehealth platforms are created equal. Some excel in providing comprehensive assessments, while others focus on quick prescriptions—sometimes at a cost to safety. The key is finding a service that combines medical expertise with a user-friendly experience. For example, trusted providers often offer detailed health evaluations, personalized treatment plans, and ongoing support, making sure your Ozempic journey is both safe and effective.
Are All Telehealth Services Created Equal When It Comes to Ozempic?
Absolutely not! It’s essential to do your homework. Look for platforms with qualified physicians, transparent pricing, and positive reviews. And don’t forget to verify if they comply with FDA guidelines, which is critical for ensuring you’re getting genuine medication. For more on how to find reliable sources, check out this comprehensive guide.
This year, the trend is clear: safe, physician-prescribed Ozempic via telehealth is no longer a novelty but a standard. It’s all about bridging the gap between convenience and safety, ensuring everyone can access effective weight-loss solutions without unnecessary risks.
If you’re eager to explore the top-rated clinics or learn more about the science behind Ozempic’s effectiveness, there’s a treasure trove of info waiting for you on our site. Dive into real patient transformations and discover how real people are achieving their goals.
So, are you ready to embrace the future of weight management? Share your thoughts or experiences with telehealth Ozempic prescriptions below—your story might inspire someone else’s journey!
Unlocking the Potential of Telehealth for Long-Term Weight Management in 2025
As telehealth continues to evolve, so does its role in facilitating safe and effective weight loss treatments like Ozempic. The convenience of virtual consultations allows individuals to access expert medical guidance from the comfort of their homes, reducing barriers such as travel time and appointment waitlists. This seamless integration of technology and healthcare is transforming the landscape of weight management, making physician-supervised Ozempic treatments more accessible than ever before.
Choosing the Right Telehealth Platform for Your Weight Loss Journey
With numerous telehealth providers available, selecting a trustworthy platform is crucial. Look for services that employ licensed physicians with expertise in endocrinology or obesity medicine, ensuring your treatment plan is personalized and safe. Transparency in pricing and adherence to FDA guidelines are also essential indicators of reputable providers. For detailed guidance on how to identify reliable sources, explore this comprehensive guide.
What Are the Key Factors That Make a Telehealth Ozempic Service Safe and Effective?
Safety and efficacy hinge on several critical elements: qualified medical oversight, detailed health assessments, and ongoing support. A top-tier telehealth service conducts thorough evaluations to determine if Ozempic is suitable for you, considering your medical history and potential side effects. Moreover, continuous monitoring helps adjust dosages and address any adverse reactions promptly. This proactive approach aligns with best practices outlined by experts like the American Society of Metabolic and Bariatric Surgery, emphasizing the importance of medical supervision for long-term success (ASMB guidelines).

Have you explored telehealth options for your weight loss journey yet? Share your experiences or ask questions below—your insights could help others navigate their path to health!
Harnessing AI and Data Analytics to Personalize Telehealth Ozempic Protocols
As telehealth platforms continue to integrate sophisticated AI algorithms, clinicians can now tailor Ozempic regimens with unprecedented precision. These systems analyze a multitude of patient data—from genetic markers to lifestyle patterns—facilitating a nuanced approach that optimizes efficacy while minimizing risks. According to a recent study published in Nature Digital Medicine, machine learning models are increasingly capable of predicting individual responses to GLP-1 receptor agonists, paving the way for truly personalized obesity treatments (source).
What Are the Challenges in Implementing AI-Driven Personalization in Telehealth?
Despite its promise, integrating AI into telehealth for weight management poses significant hurdles. Data privacy concerns are paramount, especially when handling sensitive health information. Ensuring that algorithms are free from biases and are transparent in their decision-making processes remains a critical issue. Moreover, the clinician’s role shifts from sole decision-maker to an interpreter of complex data outputs, necessitating advanced training and oversight. As noted by the FDA’s Digital Health Center, regulatory frameworks are evolving to address these challenges, emphasizing the importance of rigorous validation and accountability.
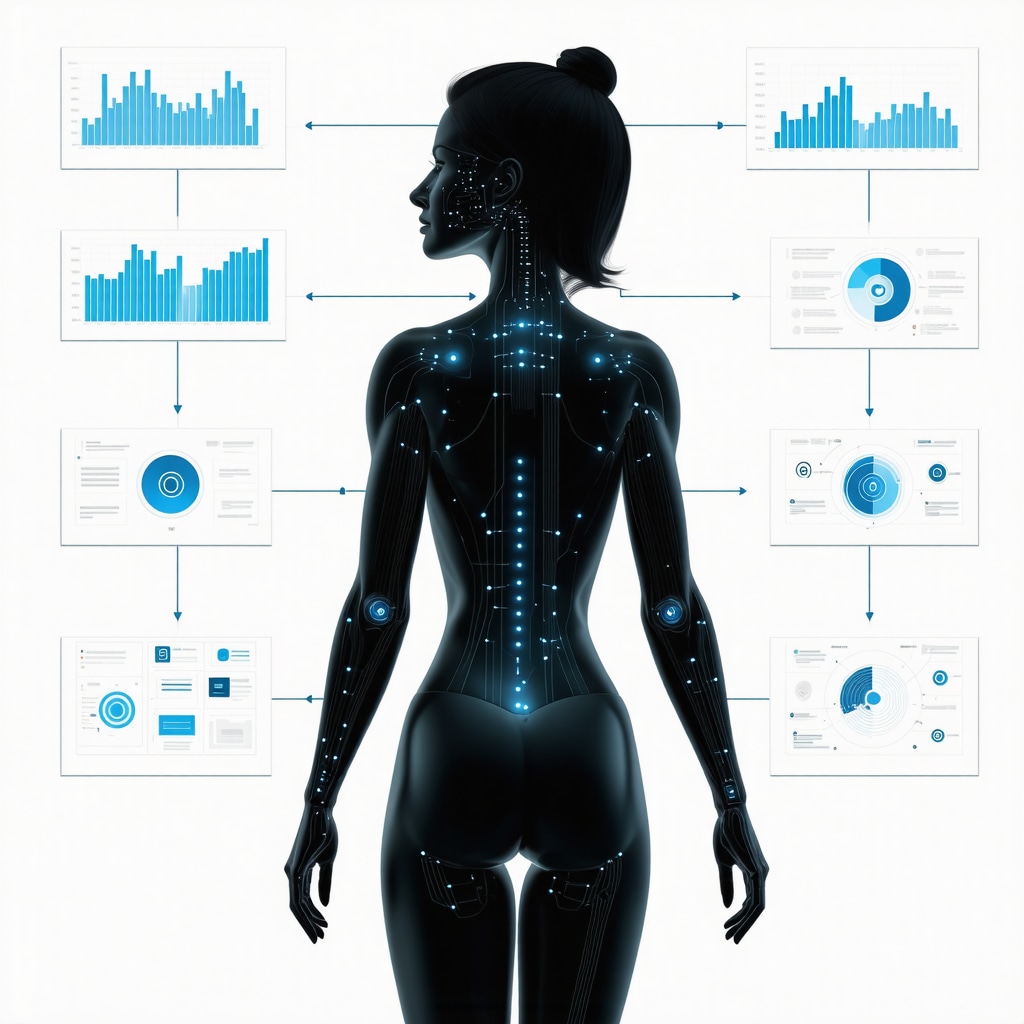
Integrating AI into telehealth requires a visual understanding of data flow and decision-making pathways. An illustrative diagram showing the interaction of patient data, AI algorithms, and clinician oversight could clarify this complex ecosystem.
Long-Term Outcomes and Monitoring: Beyond the Prescription
While initiating Ozempic therapy via telehealth is a milestone, maintaining long-term success demands continuous engagement. Telemonitoring devices, such as smart scales, glucose monitors, and wearable activity trackers, are becoming integral. These tools feed real-time data into telehealth platforms, allowing clinicians to adjust doses proactively and address side effects promptly. A 2024 report from the American Society of Metabolic and Bariatric Surgery underscores the importance of comprehensive monitoring protocols to sustain weight loss and metabolic health.
How Can Data-Driven Monitoring Improve Long-Term Outcomes in Telehealth-Led Weight Management?
Data-driven monitoring enhances patient adherence and early intervention, reducing the likelihood of complications. For example, fluctuations in blood glucose levels or unexpected weight plateaus can trigger timely clinical responses, preventing setbacks. Incorporating predictive analytics, clinicians can identify patients at risk of relapse or adverse effects before they manifest clinically. This proactive approach aligns with emerging best practices, emphasizing that successful telehealth Ozempic programs are inherently dynamic, responsive, and patient-centered.
Unlocking AI’s Potential for Truly Personalized Weight Loss Plans via Telehealth
In 2025, the integration of artificial intelligence into telehealth platforms marks a revolutionary leap forward in customizing Ozempic regimens. Advanced machine learning algorithms now analyze extensive datasets, including genetic profiles, metabolic markers, and lifestyle habits, enabling clinicians to design highly individualized treatment protocols. This precision medicine approach not only enhances efficacy but also minimizes adverse effects, setting a new standard for obesity management. An authoritative source, Nature Digital Medicine, emphasizes that AI-driven personalization is transforming the landscape of weight-loss therapies, making treatments more effective and patient-centered.
What Are the Challenges in Implementing AI-Driven Personalization in Telehealth?
Despite its promise, deploying AI in telehealth for weight management faces hurdles like ensuring data privacy, preventing algorithmic biases, and maintaining transparency in decision-making processes. Regulatory bodies such as the FDA’s Digital Health Center are evolving frameworks to address these issues, demanding rigorous validation and accountability from developers. Clinicians must also be trained to interpret AI outputs effectively, shifting their role from sole decision-makers to data interpreters, which underscores the importance of interdisciplinary expertise in this emerging landscape.
Visualize the complex data flow in AI-enhanced telehealth with a diagram illustrating patient data input, AI analysis, and clinician oversight—highlighting the seamless integration of technology and personalized care.
Enhancing Long-Term Outcomes with Real-Time Data Monitoring in Telehealth
Beyond initiating treatment, maintaining sustained weight loss necessitates continuous engagement and monitoring. Smart devices like wearable fitness trackers, glucose sensors, and smart scales feed real-time data into telehealth systems, allowing clinicians to proactively adjust Ozempic dosages and address side effects. According to the American Society of Metabolic and Bariatric Surgery, comprehensive monitoring protocols are vital for long-term success, ensuring that weight management efforts are responsive and adaptable.
How Can Data-Driven Monitoring Improve Long-Term Outcomes in Telehealth-Led Weight Management?
Real-time data enhances adherence, facilitates early intervention, and reduces the risk of setbacks. Predictive analytics identify patients at risk of weight regain or side effects before they manifest, enabling timely clinical responses. This proactive strategy aligns with emerging best practices, emphasizing that effective telehealth programs are dynamic, responsive, and tailored to individual needs. For more insights, explore this comprehensive guide.
Expert Insights & Advanced Considerations
1. The Integration of AI Enhances Personalization
Advanced telehealth platforms leverage AI to analyze extensive patient data, enabling truly individualized Ozempic treatments. This approach maximizes efficacy while minimizing adverse effects, representing a significant leap forward in precision medicine for weight management.
2. Regulatory Evolution Ensures Safer Telehealth Practices
As digital health regulations evolve, they foster greater accountability and validation for telehealth providers. This regulatory framework is crucial for maintaining high safety standards and building trust among patients seeking physician-supervised Ozempic treatments.
3. Long-term Monitoring is Critical for Sustained Success
Incorporating real-time data from wearable devices and telemonitoring tools allows clinicians to proactively manage treatment, adjust dosages, and address side effects promptly. This dynamic monitoring strategy is essential for long-term weight management success in a digital environment.
4. The Shift Toward Holistic, Data-Driven Care
Future telehealth models focus on integrating behavioral, nutritional, and medical data, creating a comprehensive approach that supports sustained weight loss. This holistic perspective aligns with the latest scientific insights into obesity management.
5. Ethical and Privacy Considerations Must Evolve in Tandem
As AI and data analytics become central, safeguarding patient privacy and ensuring algorithmic transparency are paramount. Ongoing dialogue among regulators, clinicians, and technologists will shape ethical standards for these innovative treatments.
Curated Expert Resources
- American Society of Metabolic and Bariatric Surgery (ASMBS): Offers guidelines and research on comprehensive obesity management, emphasizing safety and long-term outcomes.
- Nature Digital Medicine: Publishes cutting-edge studies on AI and personalized medicine, providing insights into technological advancements shaping telehealth.
- FDA Digital Health Center: Provides evolving regulatory frameworks and validation standards critical for AI-driven telehealth innovations.
- Obesity Medicine Association: Offers clinical best practices and protocols for integrating telehealth tools into weight management programs.
Final Expert Perspective
In 2025, the landscape of weight management via telehealth, especially with medications like Ozempic, is transforming through strategic integration of AI, robust regulation, and holistic data-driven care. These developments promise safer, more effective, and personalized treatments, but they also demand vigilant attention to ethical standards and patient privacy. As an industry leader or healthcare professional, embracing these innovations with a nuanced understanding will be key to driving sustainable success in obesity treatment. Engage with these resources, share your insights, and stay ahead of the curve—your expertise can shape the future of digital weight management.
