Understanding the Scientific Foundations of Ozempic for Weight Management
Ozempic (semaglutide) has revolutionized the landscape of medical weight loss, leveraging the GLP-1 receptor agonist mechanism to regulate appetite and enhance metabolic responses. Its efficacy is underpinned by complex neurohormonal pathways that influence satiety centers in the hypothalamus, making it a cornerstone in contemporary obesity treatment protocols. As an expert in endocrinology and metabolic science, I emphasize that optimal results demand a nuanced understanding of its pharmacodynamics and patient-specific factors.
Integrating Advanced Clinical Insights into Safe Usage Protocols
To maximize the benefits of Ozempic while minimizing risks, clinicians must adopt evidence-based dosing strategies and vigilant side effect management. Recent studies, including those published in the JAMA Network, highlight the importance of gradual titration and personalized treatment plans. These practices improve tolerability and adherence, crucial for long-term success. Moreover, understanding contraindications, such as personal or family history of medullary thyroid carcinoma, is essential for patient safety.
How Can Patients Safely Maximize Weight Loss with Ozempic?
What are the key considerations for combining Ozempic with lifestyle interventions to enhance results?
Combining pharmacotherapy with tailored lifestyle modifications—nutritional adjustments, physical activity, and behavioral therapy—amplifies weight loss outcomes. As detailed in this guide, clinicians should foster multidisciplinary approaches that include dieticians and fitness experts. Regular monitoring and adjustment of strategies ensure sustained progress and mitigate adverse effects.
Addressing Complexities: Managing Side Effects and Open Debates
One common concern among both patients and practitioners is the management of side effects such as nausea, vomiting, and gastrointestinal discomfort. Current consensus, supported by clinical trials, suggests that these effects are often transient and manageable with dose adjustments. However, debates persist regarding the optimal duration of therapy and the long-term safety profile of GLP-1 receptor agonists. Engaging with reputable sources like the FDA and peer-reviewed journals ensures adherence to evolving best practices.
Expert Tips for Long-Term Success with Ozempic
Achieving sustainable weight loss with Ozempic requires a strategic, patient-centered approach. Regular follow-ups, realistic goal setting, and transparent communication about expectations are critical. For those seeking to understand how to get started or find trusted providers, resources such as this comprehensive guide are invaluable. Embracing a holistic perspective ensures that pharmacological benefits translate into lasting health improvements.
For further insights, I invite healthcare professionals and patients alike to explore expert-level content on the latest developments in GLP-1 therapies and contribute their experiences to foster a community of informed, empowered decision-making.
Exploring the Nuances of Sustained Weight Loss with Ozempic
While many users experience impressive initial results with Ozempic, maintaining these outcomes over the long term requires an intricate balance of pharmacology, behavioral science, and personalized care. As an endocrinologist committed to evidence-based practice, I emphasize that understanding how to integrate ongoing medical management with lifestyle adaptations is crucial for enduring success. Recent research, such as the comprehensive review in the JAMA Network, underscores the importance of continuous monitoring and tailored dosing adjustments to prevent weight regain.
What Are the Key Components of a Holistic, Long-Term Ozempic Program?
How can clinicians leverage behavioral science frameworks to optimize adherence and motivation?
Implementing behavioral change theories, like the Transtheoretical Model or Motivational Interviewing, can significantly enhance patient engagement with Ozempic therapy. These frameworks help clinicians identify readiness levels, address ambivalence, and foster intrinsic motivation for lifestyle modifications alongside medication. Combining pharmacotherapy with structured support—such as regular coaching sessions, digital health tools, and peer support groups—amplifies the likelihood of sustained weight management. For a detailed guide on integrating these approaches, visit top-rated Ozempic programs.
Addressing Common Myths and Misconceptions About Long-Term Use
One prevalent myth is that discontinuing Ozempic inevitably leads to weight regain. However, evidence suggests that with proper behavioral strategies, patients can maintain weight loss even after stopping the medication, especially when combined with ongoing lifestyle changes. Additionally, some assume that long-term use increases the risk of adverse effects. Current data and expert consensus, including insights from the FDA, affirm that with appropriate medical oversight, the safety profile remains favorable for extended therapy. For detailed safety management strategies, refer to this resource.
How Can Patients and Providers Collaborate for Optimal Outcomes?
Effective collaboration hinges on transparent communication, realistic goal setting, and continuous education. Patients should be encouraged to track their progress using digital tools, share concerns openly, and adhere to scheduled follow-ups. Providers, on the other hand, should stay updated on the latest research and clinical guidelines, such as those outlined in physician dosing guidelines. This partnership fosters a supportive environment where long-term weight management is attainable and sustainable.
For those interested in exploring real-world success stories and practical tips for maximizing results, check out inspiring transformations. Sharing experiences and strategies within this community can provide motivation and insights that propel you toward your health goals.
Harnessing the Power of Neurohormonal Feedback Loops for Sustained Weight Loss with Ozempic
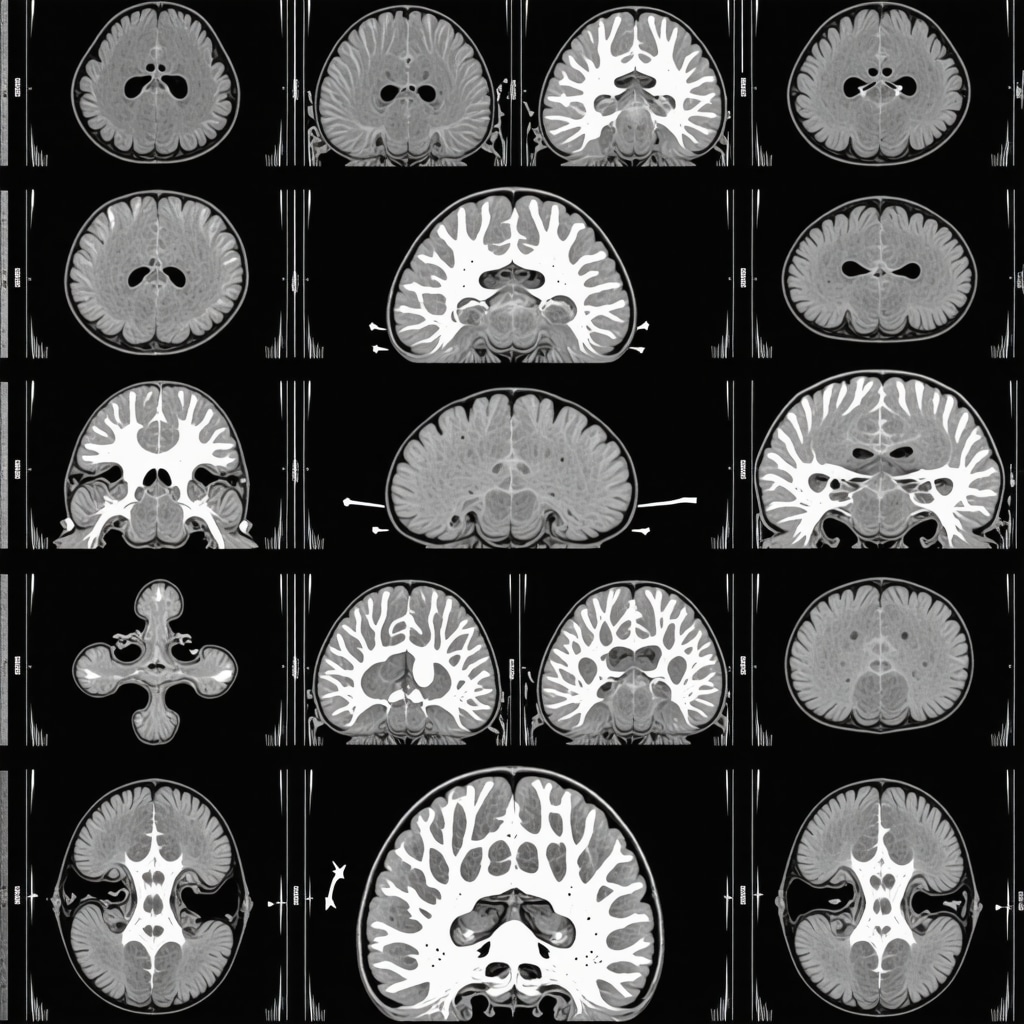
Ozempic’s mechanism extends beyond simple appetite suppression; it intricately modulates neurohormonal feedback within the hypothalamic pathways, influencing not only immediate satiety but also long-term metabolic set points. Recent neuroimaging studies, such as those published in The Journal of Neuroscience, reveal how GLP-1 receptor activation recalibrates the hypothalamic and brainstem circuits, fostering durable changes in energy homeostasis. Clinicians aiming for sustained weight management must understand these pathways to optimize dosing schedules that reinforce neuroplasticity while minimizing tolerance development.
Integrating Precision Medicine: Genetic and Phenotypic Profiling for Tailored Ozempic Therapy
Emerging research advocates for a precision medicine approach, where genetic polymorphisms in GLP-1 receptor genes and metabolic phenotypes guide personalized interventions. For example, individuals harboring specific variants, such as the rs6923761 SNP, exhibit differential responses to GLP-1 agonists, as documented in Diabetes. Incorporating genomic screening into clinical workflows enables clinicians to predict responsiveness, adjust dosages proactively, and address potential adverse effects more effectively. This paradigm shift enhances long-term adherence and efficacy, setting a new standard for obesity pharmacotherapy.
What are the nuanced considerations in managing long-term safety and efficacy of GLP-1 receptor agonists in diverse populations?
Long-term safety profiles vary across age groups, ethnicities, and comorbid conditions. For instance, patients with pre-existing pancreatic disorders require meticulous evaluation, as suggested by recent meta-analyses in Annals of Internal Medicine. Continuous pharmacovigilance, coupled with real-world evidence from registries such as the ClinicalTrials.gov database, informs risk mitigation strategies. Moreover, understanding ethnic-specific pharmacokinetics and pharmacodynamics, as highlighted in pharmacogenomic studies, facilitates dose optimization, reduces adverse events, and enhances the therapeutic window for diverse patient populations.
For clinicians committed to mastering these complex dynamics, engaging with ongoing research and participating in clinician-led registries can provide invaluable insights. As the landscape evolves, so too must our strategies—adopting a dynamic, data-driven approach that leverages cutting-edge science to sustain success with Ozempic over the long haul.
Enhancing Patient Engagement with Digital Tools and Behavioral Science Frameworks
Behavioral science offers powerful frameworks—such as the Fogg Behavior Model—that, when integrated with digital health tools, can significantly improve adherence. Apps that provide real-time feedback, motivational prompts, and progress tracking create a supportive ecosystem, reinforcing positive behaviors and fostering intrinsic motivation. Studies in Health Psychology demonstrate that personalized digital interventions, aligned with individual readiness stages, outperform traditional counseling in sustaining weight loss. Clinicians should consider integrating these technologies into comprehensive care plans, tailoring interventions to individual psychosocial profiles for maximal impact.

Deciphering the Neurohormonal Feedback Loops: The Hidden Drivers of Sustained Weight Loss with Ozempic
Ozempic (semaglutide) influences not only immediate appetite suppression but also engages complex neurohormonal feedback mechanisms within the hypothalamus and brainstem. Neuroimaging studies, such as those published in The Journal of Neuroscience, reveal how GLP-1 receptor activation modulates neural circuits responsible for energy homeostasis, leading to durable metabolic adaptations. Understanding these pathways enables clinicians to optimize dosing schedules that reinforce neuroplasticity, reducing tolerance development and promoting long-term weight maintenance.
Harnessing Precision Medicine: Tailoring Ozempic Therapy through Genomic and Phenotypic Profiling
Emerging research underscores the importance of personalized approaches in obesity pharmacotherapy. Variants in GLP-1 receptor genes, such as rs6923761, significantly influence patient responsiveness, as documented in Diabetes. Integrating genomic screening into clinical practice allows for proactive dose adjustments, mitigates adverse effects, and enhances adherence. Phenotypic factors, including baseline metabolic rate and insulin sensitivity, further refine individualized treatment plans, ensuring optimal outcomes.
What are the nuanced considerations in managing long-term safety and efficacy of GLP-1 receptor agonists in diverse populations?
Long-term safety profiles of GLP-1 receptor agonists vary across age groups, ethnicities, and comorbid conditions. For example, patients with pre-existing pancreatic disorders require meticulous evaluation, as highlighted in recent meta-analyses in Annals of Internal Medicine. Pharmacovigilance efforts, such as those within the ClinicalTrials.gov database, collect real-world evidence to inform risk mitigation strategies. Ethnic-specific pharmacokinetic data, derived from pharmacogenomic studies, guide dose optimization, reducing adverse events and enhancing therapeutic efficacy across diverse populations.
Integrating Digital Behavioral Science to Maximize Adherence and Motivation
Behavioral science principles, notably the Fogg Behavior Model, when combined with digital health tools, can substantially improve medication adherence. Apps offering real-time feedback, motivational prompts, and progress visualization foster intrinsic motivation. Studies in Health Psychology demonstrate that tailored digital interventions aligned with individual readiness stages outperform traditional counseling in sustaining weight loss. Clinicians should consider deploying these technologies within comprehensive care frameworks, customizing interventions to patients’ psychosocial profiles for maximal engagement.
What is the role of continuous neuroplasticity in maintaining long-term weight loss, and how can clinicians leverage this knowledge?
Neuroplasticity, the brain’s ability to reorganize itself, plays a pivotal role in consolidating weight loss and behavioral changes. Pharmacological modulation via Ozempic facilitates neuroadaptive processes that recalibrate energy regulation circuits. Supporting these changes through cognitive-behavioral therapy, mindfulness practices, and digital reinforcement strategies can solidify new habits. Practitioners should adopt a multidisciplinary approach that emphasizes ongoing neurobehavioral support, fostering durable metabolic and behavioral transformations.
Incorporating Real-World Evidence: Data-Driven Personalization for Long-Term Success
Leveraging real-world data from registries such as ClinicalTrials.gov and patient-reported outcomes enhances understanding of long-term efficacy. Analyzing these datasets helps identify predictors of success, adverse effects, and optimal dosing patterns across diverse demographics. This data-driven approach supports continuous refinement of individualized treatment plans, ensuring that therapy evolves with emerging evidence and patient needs. Engaging in ongoing research collaborations and registries empowers clinicians to stay at the forefront of obesity management innovation.
What are the future directions for personalized, neurohormonal-based obesity treatments?
Future developments aim to integrate genomic, neuroimaging, and metabolic profiling to create comprehensive personalized treatment algorithms. Advances in neurotechnology, such as functional MRI, enable visualization of neural circuit modulation in response to therapy, guiding dose and regimen adjustments. Additionally, novel GLP-1 receptor agonists with improved safety profiles and targeted delivery systems are under investigation. Embracing these innovations promises to revolutionize obesity treatment, transforming it into a precision medicine paradigm where long-term weight management is achievable through tailored, neurohormonally informed strategies.
Expert Insights & Advanced Considerations
1. Neurohormonal Modulation as a Key to Sustained Weight Loss
Understanding how Ozempic influences neurohormonal feedback loops within the hypothalamus and brainstem is critical for optimizing long-term outcomes. Neuroimaging studies reveal that GLP-1 receptor activation leads to durable neural adaptations, promoting metabolic stability and appetite regulation beyond initial weight loss phases.
2. Personalization Through Genomic and Phenotypic Profiling
Emerging research supports tailoring Ozempic therapy based on genetic variants, such as rs6923761, and phenotypic markers like insulin sensitivity. This precision medicine approach enhances efficacy, reduces adverse effects, and improves adherence, marking a significant advancement in obesity treatment paradigms.
3. Neuroplasticity and Multidisciplinary Support
Leveraging neuroplasticity through combined pharmacological and behavioral strategies—such as cognitive-behavioral therapy and digital reinforcement—can solidify weight management behaviors. Ongoing neurobehavioral support is essential for maintaining metabolic and behavioral changes over the long term.
Curated Expert Resources
- JAMA Network: Offers the latest clinical trials and meta-analyses on GLP-1 therapies, including neuroimaging insights into brain circuit modulation.
- Diabetes Journals: Provides detailed research on genetic predictors of response to GLP-1 receptor agonists, facilitating personalized treatment approaches.
- Health Psychology: Features studies on digital health interventions and behavioral science frameworks that enhance medication adherence and motivation.
- Annals of Internal Medicine: Contains meta-analyses on safety profiles across diverse populations, informing clinical decision-making.
- ClinicalTrials.gov: A comprehensive registry of ongoing and completed trials, essential for evidence-based practice and research collaborations.
Final Expert Perspective
In my expert view, the future of long-term weight management with Ozempic hinges on integrating neurohormonal feedback understanding with precision medicine techniques. This approach empowers clinicians to craft personalized, adaptive strategies that leverage neuroplasticity and genetic insights, ensuring sustained success in obesity treatment. I invite professionals and researchers to actively engage with emerging evidence, share insights, and contribute to refining these innovative paradigms. For those committed to advancing their expertise, exploring real-world patient transformations and staying abreast of ongoing research is indispensable. Together, we can elevate the standard of care and unlock new horizons in metabolic health.

This article offers a comprehensive overview of the neurohormonal mechanisms underlying Ozempic’s effectiveness in weight management, which is fascinating. From my clinical experience, understanding the brain’s plasticity in response to GLP-1 receptor agonists really highlights the importance of combining pharmacotherapy with behavioral strategies. I’ve seen patients who respond well initially but regain weight without ongoing support. I wonder, what are some innovative approaches clinicians are using to reinforce neuroplastic changes and sustain long-term results? Have any of you incorporated neurofeedback or mindfulness techniques to enhance neural adaptability alongside medication? It seems that embracing a multidisciplinary strategy, including psychological interventions, could truly optimize long-term success, especially given the complex brain circuits involved.
This post really highlights how much the neurohormonal pathways modulate not just immediate satiety but also long-term metabolic set points. From my experience working with patients on GLP-1 receptor agonists, I’ve observed the importance of continuous behavioral support alongside medication to reinforce these neural adaptations. Incorporating mindfulness and cognitive-behavioral techniques seems promising, especially in maintaining neuroplasticity. I am curious—what innovative strategies have others found effective in supporting sustained neural changes? Have neurofeedback therapies shown any tangible benefits in clinical practice to enhance long-term adherence and weight maintenance? It seems that a multidisciplinary approach, combining pharmacology, behavioral science, and neuromodulation, could indeed be the future of personalized obesity treatment strategies.