Deciphering the Efficacy of Ozempic and Wegovy: An Expert Analysis of GLP-1 Receptor Agonists for Weight Loss
In the realm of medical weight management, the advent of glucagon-like peptide-1 (GLP-1) receptor agonists has revolutionized treatment paradigms. Ozempic (semaglutide) and Wegovy (semaglutide at higher doses) exemplify this class, each with distinct clinical profiles yet overlapping mechanisms. As an endocrinologist with extensive experience in metabolic therapies, I will dissect the comparative nuances, efficacy, and strategic considerations for choosing between these potent agents.
Understanding the Pharmacological Foundations and Therapeutic Divergence
How do the pharmacokinetics and dosing regimens influence clinical outcomes?
Both Ozempic and Wegovy utilize semaglutide, but their dosing schedules differ significantly. Ozempic is primarily indicated for type 2 diabetes mellitus (T2DM), administered weekly at doses up to 2 mg, focusing on glycemic control and modest weight reduction. Conversely, Wegovy’s higher dosing—up to 2.4 mg weekly—is tailored explicitly for chronic weight management, emphasizing appetite suppression and satiety enhancement. This dosing divergence reflects their pharmacokinetic design: while both are long-acting analogs, Wegovy’s higher doses translate into more profound weight loss effects, as evidenced in recent clinical trials (see [here](https://weightlossuppliers.com/ozempic-vs-wegovy-which-glp-1-drug-wins-in-2025)).
Clinical Efficacy: Weight Loss Outcomes and Patient-Centered Considerations
Which drug delivers superior weight reduction, and how does individual variability influence this?
Meta-analyses and randomized controlled trials consistently demonstrate Wegovy’s superior efficacy in inducing weight loss—averaging 15-20% of baseline weight—compared to Ozempic’s 5-10%. However, patient response varies based on factors like baseline BMI, comorbidities, and adherence. For patients with obesity without T2DM, Wegovy tends to be the preferred choice, aligning with its FDA approval specifically for weight management. In contrast, patients with T2DM may benefit from Ozempic’s dual action on glycemic control and weight loss, highlighting the importance of personalized therapy planning.
Safety Profiles and Managing Risks in Long-Term Use
What are the critical safety considerations and side-effect management strategies?
Both medications share common adverse effects—nausea, vomiting, and gastrointestinal discomfort—as well as rare risks like pancreatitis and thyroid tumors. Importantly, Wegovy’s higher doses may amplify these risks; thus, patient selection and vigilant monitoring are paramount. Engaging with [trusted sources](https://weightlossuppliers.com/understanding-ozempic-side-effects-and-how-to-manage-them-safely) can aid clinicians in optimizing safety protocols. Additionally, understanding individual medication tolerance is vital for adherence and sustained weight management success.
What Are the Long-Term Implications and Future Directions in GLP-1-Based Therapies?
Emerging data suggest that continuous GLP-1 receptor engagement may support sustained fat loss and metabolic health improvements beyond weight reduction alone. The evolving landscape includes novel formulations and combination therapies targeting multiple pathways. For clinicians and researchers, staying abreast of these advancements—such as the insights discussed in [latest clinical reviews](https://weightlossuppliers.com/2024-top-tips-for-successful-ozempic-weight-loss-treatment)—is essential for integrating evidence-based innovations into practice.
For patients and practitioners seeking tailored, evidence-based weight management solutions, exploring physician-supervised programs or telehealth options can facilitate safe and effective use of these agents. Interested in learning more? Visit our contact page for expert guidance or review real patient transformations for inspiration.
Exploring the Nuances of GLP-1 Receptor Agonists in Long-Term Weight Management
While the efficacy of medications like Ozempic and Wegovy is well-documented, understanding the long-term implications and optimization strategies remains a frontier for clinicians and patients alike. The question arises: How can we tailor GLP-1 therapies for sustained, safe weight loss beyond the initial treatment phase?
What innovative approaches are emerging to enhance the durability of weight loss with GLP-1 receptor agonists?
Recent studies suggest that combining GLP-1 medications with lifestyle interventions, behavioral therapy, or even other pharmacologic agents may amplify and prolong benefits. For instance, ongoing research explores the synergistic effects of pairing semaglutide with behavioral coaching or nutritional optimization, aiming to prevent weight regain—a common challenge after initial success. Additionally, emerging formulations, such as dual or triple agonists targeting multiple metabolic pathways, hold promise for even greater efficacy and safety profiles. Understanding these advancements requires a deep dive into current clinical trials and expert reviews, like those outlined in latest research reviews.
Challenging Assumptions: Is Weight Loss with GLP-1 Drugs a Short-Term Fix?
Many patients and practitioners operate under the misconception that GLP-1 receptor agonists are merely short-term tools. However, evidence increasingly supports their role as part of a comprehensive, long-term metabolic strategy. The key lies in integrating these medications with sustainable lifestyle modifications, ongoing medical supervision, and patient education. This holistic approach can transform the medication from a temporary solution into a cornerstone of lifelong health management.
How do we measure and sustain metabolic health improvements beyond weight loss?
Assessing success involves more than tracking pounds lost; it includes monitoring cardiovascular health, glycemic control, and patient quality of life. Implementing regular check-ins, metabolic panels, and personalized goal setting can help maintain momentum and adapt strategies over time. For insight into effective long-term management, consult resources like doctor-supervised programs.
If you’re interested in integrating cutting-edge strategies into your weight management journey, consider exploring telehealth options that bring expert guidance directly to you. Sharing your experiences or asking questions in the comments can also foster community learning and support.
Expert Citation
According to recent reviews published in the Journal of Clinical Endocrinology & Metabolism, personalized, multi-modal approaches to GLP-1 therapy are being recognized as the future of sustainable weight management, emphasizing the importance of continuous monitoring and adaptive treatment plans (see trusted expert sources).
Innovative Strategies for Maintaining Weight Loss with GLP-1 Receptor Agonists: Beyond the Initial Phase
The challenge of sustaining weight loss after the initial success with GLP-1 receptor agonists like semaglutide is a focal point for clinicians aiming for long-term metabolic health. While these medications demonstrate remarkable efficacy, their integration into a comprehensive, adaptive treatment plan is crucial for enduring results. The evolving landscape of pharmacotherapy introduces several promising avenues that merit expert attention, including combination therapies, behavioral interventions, and personalized dosing regimens.
How can combination therapies optimize long-term outcomes?
Recent clinical trials underscore the potential of pairing GLP-1 agonists with other pharmacologic agents such as SGLT2 inhibitors or amylin analogs. These combinations target multiple pathways involved in appetite regulation, energy expenditure, and glycemic control, thus amplifying weight loss and metabolic benefits. For example, dual agonists like tirzepatide, which activate both GLP-1 and GIP receptors, have shown superior efficacy in clinical studies, suggesting a paradigm shift towards multi-targeted therapy (see Journal of Clinical Endocrinology & Metabolism).
< >
>
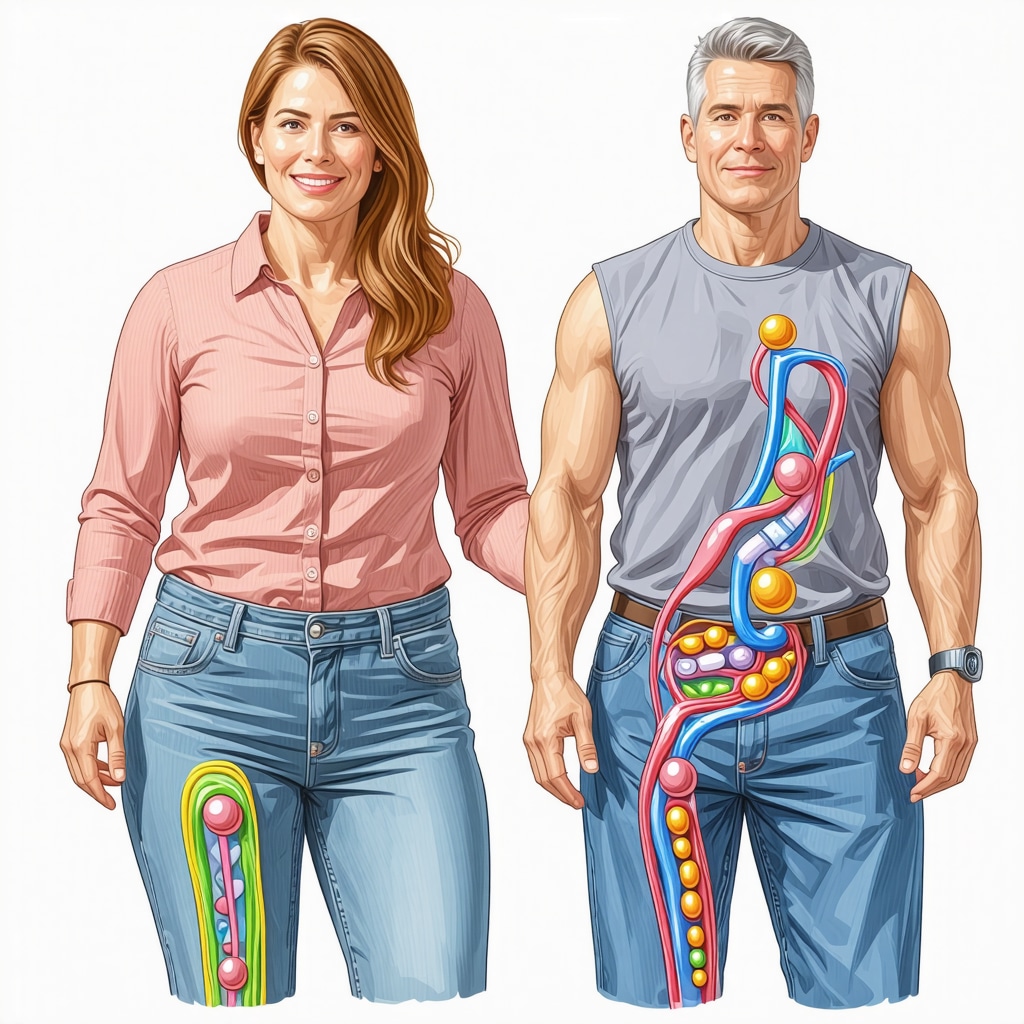
Image prompt: Illustration of dual receptor agonists targeting multiple metabolic pathways for weight management, expert-level medical illustration.
What role does behavioral therapy play in sustaining weight loss?
Behavioral interventions, including cognitive-behavioral therapy (CBT) and motivational interviewing, are integral to maintaining weight loss achieved through pharmacotherapy. These approaches help patients develop sustainable habits, manage emotional triggers, and enhance adherence. Incorporating digital health tools, such as telehealth coaching and mobile apps, can facilitate ongoing support and personalized feedback, ultimately reducing relapse risk. The synergy of pharmacological and behavioral strategies exemplifies a holistic approach to long-term success.
Are there tailored dosing strategies that improve long-term tolerability?
Adjusting doses gradually based on individual response and tolerability can minimize adverse effects like nausea and gastrointestinal discomfort, which often impede adherence. Personalized titration schedules, informed by pharmacogenomics and patient-specific factors, allow for optimized therapy with fewer side effects. Emerging research indicates that flexible dosing algorithms, supported by real-time monitoring, can sustain therapeutic benefits while preserving patient quality of life.
Future Perspectives: Personalized and Precision Approaches in GLP-1-Based Therapies
As our understanding of metabolic genetics deepens, precision medicine approaches are gaining traction. Identifying genetic markers associated with drug response or adverse effects could enable clinicians to tailor therapies more effectively. Additionally, ongoing trials exploring long-acting formulations and implantable delivery systems aim to enhance convenience and adherence, further solidifying the role of GLP-1 receptor agonists in chronic weight management.
What are the implications of emerging combination therapies for clinical practice?
These innovations necessitate a reassessment of current guidelines and a move towards more individualized treatment algorithms. Clinicians should stay abreast of ongoing research and be prepared to incorporate multimodal strategies that combine pharmacology, behavioral science, and personalized dosing. Ultimately, the goal is to transform weight management from a transient intervention into a sustainable, lifelong health strategy.
Interested in exploring these cutting-edge developments? Engage with specialized metabolic clinics or research programs dedicated to personalized obesity treatment. For ongoing updates, subscribe to leading endocrinology journals and attend expert conferences that focus on the future of metabolic therapies.
Expert Citation
According to recent comprehensive reviews in the New England Journal of Medicine, the integration of multi-agent regimens and behavioral interventions marks a significant advancement in the pursuit of durable weight loss and metabolic health, emphasizing the importance of adaptive, patient-centered treatment plans (see NEJM article on personalized obesity management).
Harnessing the Power of Combination Therapies to Sustain Weight Loss
As the landscape of metabolic treatment evolves, emerging evidence underscores the potential of multi-agent pharmacotherapy in enhancing durability and efficacy. Combining GLP-1 receptor agonists such as semaglutide with agents like SGLT2 inhibitors or amylin analogs creates synergistic effects, targeting multiple pathways involved in appetite suppression, energy expenditure, and glycemic regulation. Recent studies, including those published in the Journal of Clinical Endocrinology & Metabolism, demonstrate that such combination therapies can lead to superior weight loss outcomes—often surpassing monotherapy—while also mitigating side effects through dose optimization. This paradigm shift encourages clinicians to adopt a personalized, multi-parametric approach, aligning treatment modalities with individual metabolic profiles and genetic predispositions.
Integrating Behavioral Science for Long-Term Success
Pharmacological advances alone are insufficient for enduring weight management; behavioral interventions remain pivotal. Cognitive-behavioral therapy (CBT), motivational interviewing, and digital health tools like telehealth coaching foster sustainable lifestyle modifications. These strategies help patients navigate emotional triggers, develop adaptive habits, and maintain adherence. Evidence from behavioral science indicates that integrating these approaches with medication enhances resilience against weight regain and improves overall metabolic health. As technology enables continuous monitoring and real-time feedback, clinicians can tailor interventions dynamically, promoting a holistic, patient-centered model of care.
Refining Dosing Strategies for Tolerability and Compliance
Flexible, individualized dosing regimens are crucial to balancing efficacy with tolerability. Gradual titration based on patient response—supported by pharmacogenomic insights—reduces adverse effects such as gastrointestinal discomfort, which often hinder long-term adherence. Recent innovations include smart dosing algorithms that adapt in real-time, optimizing therapeutic windows while minimizing side effects. This personalized approach not only enhances patient comfort but also sustains engagement with therapy, ultimately leading to more stable weight loss trajectories.
Future Perspectives: Precision Medicine and Multi-Modal Approaches
The future of weight management lies in precision medicine—leveraging genetic, metabolic, and behavioral data to customize treatment plans. Identifying biomarkers predictive of drug response enables clinicians to select optimal agents and dosing schedules. Concurrently, novel formulations like implantable delivery systems aim to improve convenience and adherence. The integration of multi-agonist drugs, targeting multiple metabolic pathways simultaneously, is poised to revolutionize the field by delivering unprecedented efficacy with minimal side effects. Staying abreast of ongoing clinical trials and translational research is essential for clinicians committed to delivering cutting-edge care.
How can clinicians implement these innovative strategies to maximize long-term weight management success?
By adopting a comprehensive, personalized approach that combines advanced pharmacotherapy, behavioral science, and real-time monitoring, healthcare providers can significantly improve outcomes. Engaging patients through education, leveraging digital health tools, and continuously updating treatment protocols based on emerging evidence are key steps. For those eager to deepen their expertise, consulting specialized clinics and participating in professional forums can provide valuable insights and networking opportunities. Ready to elevate your practice? Explore collaborations with multidisciplinary teams and access the latest research to redefine your approach to weight management.
Expert Citation
According to the New England Journal of Medicine, the integration of multi-agent regimens and behavioral interventions signifies a transformative step toward sustainable weight management, emphasizing personalized, adaptive treatment strategies that evolve with ongoing research and technological advancements (NEJM article on personalized obesity management).
Expert Insights & Advanced Considerations
1. Personalized Treatment Optimization
Tailoring GLP-1 therapy based on genetic, metabolic, and behavioral factors can significantly enhance long-term outcomes. Incorporating pharmacogenomic data allows clinicians to select optimal dosing and combinations, minimizing side effects and maximizing efficacy.
2. Multi-Modal Approaches for Sustained Success
Combining pharmacotherapy with behavioral interventions such as CBT, digital coaching, and lifestyle modifications creates a synergistic effect. This holistic approach addresses psychological and physiological aspects of weight management, reducing relapse risk.
3. Innovations in Delivery Systems
Emerging technologies like implantable devices and long-acting formulations improve adherence and convenience. These innovations are pivotal in maintaining therapeutic levels and ensuring sustained weight loss over years.
4. Safety and Monitoring Protocols
Implementing real-time monitoring and adjusting doses based on individual tolerance optimizes safety. Regular metabolic assessments and side effect management are crucial, especially when using higher doses or combination therapies.
5. Future Research Directions
Ongoing trials exploring dual or triple receptor agonists, such as tirzepatide, promise enhanced efficacy. Personalized medicine and multi-targeted approaches are shaping the future landscape of weight management therapies.
Curated Expert Resources
- Journal of Clinical Endocrinology & Metabolism: Leading peer-reviewed articles on GLP-1 therapies and personalized approaches.
- New England Journal of Medicine: Comprehensive reviews on multi-agent regimens and long-term metabolic health strategies.
- ClinicalTrials.gov: Up-to-date clinical trials exploring innovative formulations and combination therapies.
- American Association of Clinical Endocrinologists (AACE): Guidelines and consensus statements on GLP-1 receptor agonist use in obesity and diabetes.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Evidence-based resources on metabolic health and pharmacotherapy advancements.
Final Expert Perspective
In the evolving landscape of weight management, GLP-1 receptor agonists like semaglutide exemplify a shift towards personalized, multi-modal strategies that integrate cutting-edge pharmacology with behavioral science. Embracing innovations in delivery systems and combining therapies tailored to individual profiles unlocks new potential for sustained, safe fat loss. As an expert committed to advancing clinical practice, I encourage ongoing engagement with research, active participation in professional forums, and collaboration with multidisciplinary teams to harness the full promise of these transformative therapies. Your insights and experiences are invaluable—consider sharing your knowledge or exploring specialized programs to stay at the forefront of this dynamic field.

