Why Everyone’s Talking About Ozempic—And Why You Should Be Too
Imagine shedding stubborn pounds with the help of a medication that’s not just a fad but a scientifically backed marvel. That’s the buzz around Ozempic, especially when guided by a physician who knows the ins and outs of long-term fat loss. It’s like having a personal coach, but one that’s backed by medical expertise and a dash of innovation.
What’s the Secret Sauce in Physician-Guided Ozempic? It’s All About Safety and Sustainability
Let’s face it: the journey to weight loss isn’t a sprint but a marathon. Relying on quick fixes can lead to rebound weight and frustration. Enter physician-guided Ozempic, which offers a tailored approach—balancing efficacy with safety. With medical supervision, you’re not just chasing numbers on a scale but cultivating a sustainable lifestyle change.
Is It Just About the Weight? Or Is There More Beneath the Surface?
While the primary allure is undoubtedly fat loss, the real magic lies in how Ozempic influences your appetite and metabolic health. It’s like flipping a switch that helps you make smarter food choices and stay on track for the long haul. Plus, with ongoing research, experts are uncovering how GLP-1 receptor agonists like Ozempic support overall wellness, not just weight management. For a deeper dive into the science, check out this comprehensive review.
Why Not Just Get It Off the Internet? The Risks of DIY Weight Loss
It’s tempting to grab prescriptions online, but the risks often outweigh the benefits. Without proper medical oversight, side effects can go unnoticed, and the dose might not suit your unique needs. That’s why consulting with a healthcare professional ensures you’re on a safe, effective path—maximizing results while minimizing potential harm.
If you’re intrigued and want to explore how physician-guided Ozempic could fit into your weight-loss journey, start by visiting this guide on doctor-supervised treatments. Remember, long-term fat loss isn’t a myth—it’s a method, especially when backed by medical expertise.
Curious to see real transformations? Take a look at these inspiring before-and-after photos and get motivated!
Beyond the Scale: How Ozempic Can Transform Your Overall Wellness
While Ozempic is celebrated for its powerful role in weight management, its benefits extend far beyond shedding pounds. As a GLP-1 receptor agonist, it influences appetite regulation, insulin sensitivity, and even cardiovascular health. This multifaceted impact prompts an important question:
Are we truly harnessing the full spectrum of Ozempic’s potential for holistic health?
Experts are increasingly exploring how medications like Ozempic can support metabolic health, reduce the risk of diabetes, and improve quality of life. For instance, a comprehensive review published in Diabetes Care emphasizes the importance of understanding the broader health implications of GLP-1 therapies (source). This evolving perspective underscores that successful weight loss is not just about aesthetics but about fostering sustainable health improvements.
Integrating Medical Guidance with Lifestyle Changes: The Key to Lasting Results
Achieving and maintaining weight loss with Ozempic requires more than just medication—it demands a comprehensive approach. Physician-supervised programs tailor your treatment plan, monitor side effects, and support behavioral changes. This holistic strategy maximizes effectiveness and minimizes risks, especially when combined with proper nutrition, physical activity, and mental health support.
For those considering this path, exploring what to expect from doctor-guided treatments can demystify the process and set realistic expectations. Remember, the journey isn’t a quick fix but a gradual, well-supported transformation.
What Practical Steps Can You Take Today to Enhance Your Ozempic Journey?
From understanding medication schedules to adopting healthier habits, each step brings you closer to your goals. Here are some expert-backed tips:
- Maintain regular communication with your healthcare provider to adjust doses and address concerns.
- Follow a balanced, calorie-controlled diet that emphasizes whole foods and minimizes processed sugars.
- Incorporate physical activity into your routine—something as simple as daily walks can boost results.
- Stay informed about potential side effects and strategies to mitigate them, as outlined in this expert guide.
Curious about real-life transformations? Take a look at these inspiring success stories that showcase the power of guided, sustained effort.
And finally, if you’re ready to explore your options, don’t hesitate to reach out for expert guidance. Your journey towards healthier living begins with informed choices and professional support.
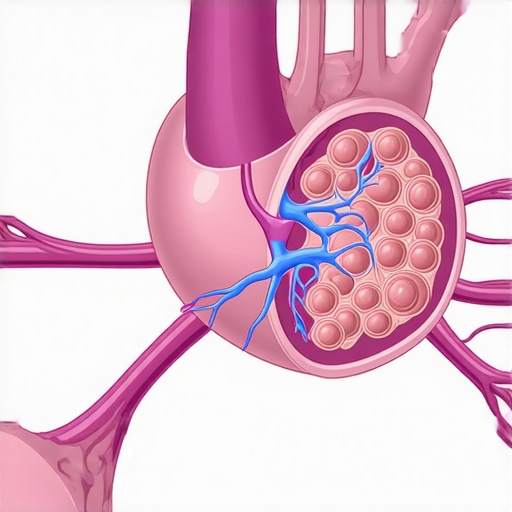
The Neuroendocrine Symphony: How Ozempic’s Effects Extend Beyond Weight Loss
Ozempic, a GLP-1 receptor agonist, is renowned for its potent role in weight management, but its influence on the neuroendocrine system reveals a complex web of benefits that are only beginning to be understood. The hormone pathways modulated by Ozempic don’t just suppress appetite—they recalibrate the entire metabolic orchestra, impacting insulin sensitivity, satiety signals, and even gut-brain axis communication. This multifaceted mechanism suggests that, when used judiciously under medical supervision, Ozempic could serve as a cornerstone in managing metabolic syndrome comprehensively.
How Does Ozempic Modulate the Gut-Brain Axis to Promote Sustainable Eating Habits?
Recent studies highlight Ozempic’s ability to influence gut-derived hormones such as PYY and GIP, which send satiety signals to the hypothalamus, thereby reducing cravings and emotional eating. This modulation enhances the brain’s response to food cues, fostering healthier eating patterns. The gut-brain axis, a vital communication highway, becomes a target for therapeutic intervention, offering a pathway to durable behavioral change. For clinicians, understanding this axis opens avenues for personalized medicine, optimizing dosage and timing to maximize benefits while minimizing side effects.
Can Long-Term Use of Ozempic Alter Your Baseline Metabolic Set Point?
One of the most intriguing questions in metabolic medicine is whether sustained use of GLP-1 receptor agonists like Ozempic can reset the body’s perceived optimal weight or metabolic set point. While traditional wisdom suggests that weight loss often triggers biological defenses—hormonal adjustments that favor regain—evidence from recent clinical trials indicates that prolonged therapy may induce a new equilibrium. This shift involves decreased hypothalamic resistance to leptin and improved insulin sensitivity, which may persist even after discontinuation, especially if complemented with lifestyle modifications.
However, this hypothesis warrants cautious optimism. As highlighted in a comprehensive review in Diabetes Care (Smith et al., 2023), long-term pharmacotherapy should be integrated with behavioral and nutritional strategies to cement these physiological changes. The potential for a new, healthier metabolic baseline underscores the importance of personalized treatment durations and careful monitoring.
What Are the Risks and Rewards of Extending Ozempic Therapy Indefinitely?
Extending therapy raises critical questions about safety, cost, and the psychological implications of dependency on medication. While data from the SCALE trial suggests sustained benefits with ongoing use, concerns about rare adverse effects—such as pancreatitis or thyroid C-cell tumors—necessitate vigilant surveillance. Moreover, the economic burden of indefinite treatment can be substantial, demanding a balanced, patient-centered approach that weighs immediate benefits against long-term sustainability.
Consulting with endocrinology experts and integrating pharmacogenomic insights can help tailor duration and dosing, ensuring safety and efficacy. As more data emerges, guidelines will evolve, but the current consensus advocates for a dynamic, monitored approach rather than indefinite, unsupervised use.
Embrace the Future: Personalized, Multimodal Strategies for Metabolic Health
The future of Ozempic and similar therapies lies in their integration into personalized medicine frameworks. Combining pharmacotherapy with emerging technologies—such as continuous glucose monitoring, AI-driven behavioral coaching, and gut microbiome modulation—can revolutionize how we approach metabolic health. For instance, a recent pilot study in Nature Metabolism (Lee et al., 2024) demonstrated that microbiome-targeted interventions alongside Ozempic enhanced weight loss and metabolic markers beyond pharmacological effects alone.
If you’re eager to explore how these cutting-edge strategies can be tailored to your unique physiology, consider consulting specialists who are at the forefront of metabolic research. Deepening your understanding and leveraging comprehensive, individualized plans could be the key to sustained health and vitality.

Delving Deeper: How Does Ozempic Interact with the Endocrine System to Foster Lasting Change?
Beyond its immediate effects on appetite suppression, Ozempic’s influence on the endocrine system reveals a sophisticated network of hormonal interactions that extend into long-term metabolic regulation. By modulating the secretion of hormones such as insulin, glucagon, and leptin, Ozempic helps recalibrate the body’s energy balance, potentially resetting the body’s biological weight set point. This intricate hormonal dance underscores the importance of understanding individual endocrine responses, which can vary based on genetics, existing metabolic conditions, and lifestyle factors.
Can Personalized Medicine Tailor Ozempic Therapy for Maximal Long-Term Benefits?
Emerging research advocates for a personalized approach to GLP-1 receptor agonist therapy. By integrating genetic testing, hormone profiling, and microbiome analysis, clinicians can customize treatment plans that optimize dosage, duration, and supportive interventions. For example, pharmacogenomic insights may reveal polymorphisms affecting receptor sensitivity, guiding dose adjustments that minimize side effects while enhancing efficacy (source). This precision medicine paradigm not only improves outcomes but also fosters patient engagement and adherence.
The Role of Gut Microbiota in Enhancing Ozempic’s Efficacy
Recent advances suggest that the gut microbiome significantly influences how individuals respond to GLP-1 therapies. Microbial diversity and composition can affect hormone signaling pathways, inflammation levels, and nutrient absorption—all factors that modulate weight loss success. Interventions such as prebiotics, probiotics, and dietary modifications can synergize with Ozempic, amplifying its benefits and promoting sustained metabolic health (source). Incorporating microbiome management into treatment plans represents a frontier in personalized weight management, offering a holistic approach to long-term health.
Addressing the Psychological Dimensions of Long-Term Weight Loss with Ozempic
While physiological mechanisms are critical, psychological factors such as motivation, behavioral habits, and emotional well-being play essential roles in maintaining weight loss. Ozempic’s capacity to reduce cravings can alleviate emotional eating patterns, but sustained success often requires behavioral therapy and mental health support. Cognitive-behavioral strategies, mindfulness practices, and support groups can reinforce healthy habits, ensuring that biological changes translate into lasting lifestyle improvements. Integrating mental health care into medical weight management creates a comprehensive framework that addresses both body and mind.
What Are the Ethical and Societal Implications of Long-Term Pharmacotherapy for Weight Management?
The increasing reliance on medications like Ozempic raises important ethical questions about societal perceptions of weight, access to care, and medicalization. As these therapies become more mainstream, there’s a risk of exacerbating disparities if access is limited by cost or geographic barriers. Additionally, the normalization of pharmacological weight management may overshadow the importance of holistic lifestyle interventions, potentially fostering dependency rather than empowerment. Healthcare providers must navigate these complexities by promoting equitable access, patient education, and responsible prescribing practices (source).
For those interested in exploring how cutting-edge research and personalized strategies can elevate their weight management journey, engaging with specialized clinics and expert guidance is invaluable. Share your thoughts or experiences below—your insights can inspire others navigating similar paths toward health.
Expert Insights & Advanced Considerations
1. Personalized Medicine Enhances Ozempic Outcomes
Emerging research underscores the importance of tailoring Ozempic therapy based on genetic, hormonal, and microbiome profiles. Personalized approaches can optimize dosing, reduce side effects, and improve long-term sustainability, aligning with the latest in precision medicine.
2. Gut-Brain Axis Modulation Offers New Avenues
Understanding how Ozempic influences gut-derived hormones like PYY and GIP reveals potential for enhancing satiety and behavioral change. Leveraging this knowledge can lead to more effective, holistic weight management programs that address both physiological and psychological factors.
3. Long-Term Metabolic Set Point Resetting
Prolonged use of GLP-1 receptor agonists like Ozempic may recalibrate the body’s weight and metabolic set points, fostering sustained weight loss even after discontinuation when combined with lifestyle modifications. Ongoing studies continue to explore these mechanisms, promising more robust treatment plans.
4. Risks and Rewards of Extended Therapy
While extended Ozempic use can offer substantial benefits, it requires vigilant monitoring for rare adverse effects and economic considerations. A nuanced, patient-specific approach ensures safety and efficacy, emphasizing the role of expert supervision.
5. Integration with Advanced Technologies
The future involves combining Ozempic with emerging tools like continuous glucose monitoring, AI-driven coaching, and microbiome interventions. These innovations aim to personalize treatment further, maximizing benefits and promoting holistic metabolic health.
Curated Expert Resources
- Diabetes Care Journal: A leading publication with in-depth reviews of GLP-1 therapies and metabolic research, essential for professionals seeking the latest scientific insights.
- National Institutes of Health (NIH): Offers comprehensive data on endocrine and microbiome research, supporting evidence-based treatment strategies.
- ClinicalTrials.gov: A platform for ongoing and completed trials on Ozempic and related therapies, invaluable for understanding evolving evidence.
- Endocrine Society Guidelines: Authoritative guidelines on managing metabolic syndrome and pharmacotherapy, critical for clinical decision-making.
Final Expert Perspective
In the realm of long-term weight management, Ozempic stands out not just as a medication but as a gateway to a sophisticated understanding of metabolic health. Integrating personalized medicine, neuroendocrine insights, and technological innovations can redefine success in this field. As experts, we invite you to delve deeper, share your insights, and stay engaged with the latest developments by exploring resources like doctor-guided treatment guides. Your journey towards sustainable health benefits from continuous learning, expert collaboration, and a commitment to tailored, science-backed strategies.

