Unlocking the True Potential of Ozempic for Sustainable Weight Loss
In the rapidly evolving landscape of medical weight management, Ozempic has emerged as a revolutionary GLP-1 receptor agonist that offers not just glucose control but also significant weight loss benefits. However, maximizing the success of Ozempic weight loss programs requires more than just adherence to medication; it demands an integrative approach anchored in expert guidance, personalized strategies, and a deep understanding of the drug’s mechanisms.
Synergizing Lifestyle Modifications with Ozempic Therapy
While Ozempic (semaglutide) pharmacologically aids appetite suppression and improves metabolic efficiency, pairing it with tailored lifestyle changes exponentially enhances outcomes. Experts emphasize the importance of adopting a balanced nutritional plan that prioritizes whole foods, fiber-rich vegetables, and lean proteins to complement Ozempic’s gastrointestinal effects, reducing common side effects like nausea. Incorporating consistent physical activity, even moderate-intensity exercises such as walking or swimming, fosters improved insulin sensitivity and accelerates fat oxidation.
How Can Personalized Medical Supervision Elevate Ozempic Outcomes?
Medical supervision is paramount in navigating dosage titration, monitoring side effects, and optimizing weight loss timelines. Physician-led programs facilitate individualized dosing schedules that minimize adverse effects and align with patient-specific metabolic responses. According to expert clinical protocols, gradual dose escalation, paired with ongoing assessment, ensures safety and maximizes fat loss efficiency over the typical 12 to 16-week treatment windows (source). Furthermore, supervised care allows integration of behavioral counseling and psychological support, addressing emotional eating patterns that pharmacotherapy alone cannot resolve.
Leveraging Data-Driven Tracking to Sustain Progress
Objective tracking tools—ranging from digital weight logs to continuous glucose monitors—empower patients and clinicians to make informed adjustments. Monitoring weight trajectories, appetite fluctuations, and metabolic markers enables dynamic fine-tuning of Ozempic programs, preventing plateaus and ensuring long-term adherence. Experts advocate for weekly progress reviews combined with patient education on interpreting their metrics, fostering a proactive mindset and accountability.
Mitigating Side Effects through Expert-Recommended Practices
Gastrointestinal discomfort is the most common barrier to adherence. Expert advice recommends gradual dose titration, meal timing adjustments, and hydration strategies to alleviate symptoms. Additionally, patient education on recognizing and managing side effects prevents premature discontinuation, a critical factor in successful weight loss with Ozempic (learn more).
Exploring Integrative Support: Beyond Medication
Incorporating adjunct therapies such as nutritional counseling, mindfulness-based stress reduction, and sleep optimization can profoundly influence outcomes. Stress and poor sleep quality trigger hormonal imbalances that undermine weight loss efforts; thus, a holistic approach addressing these domains complements Ozempic’s pharmacodynamics for enhanced efficacy.
Ready to elevate your weight loss journey with expert-led Ozempic programs? Discover clinics offering physician-supervised treatments that tailor plans to your unique needs and lifestyle.
Reflecting on My Journey: The Power of Medical Supervision and Personalization
When I first started my Ozempic weight loss journey, I assumed that simply taking the medication would be enough to see results. However, it quickly became clear that the real magic happened when my treatment was closely supervised by an experienced physician. This personalized medical supervision allowed for careful dose adjustments and helped me navigate side effects effectively. The gradual titration process made the initial nausea manageable, and having a healthcare professional to consult regularly gave me confidence and kept me motivated.
What surprised me was how much the behavioral support integrated into the program influenced my habits. Addressing emotional eating and stress through counseling complemented the medication’s effects, making sustainable lifestyle changes more achievable. This holistic approach, emphasized by many experts, was a game changer in my weight loss journey (source).
Tracking Progress: More Than Just Numbers on a Scale
One of the most empowering aspects of my experience was learning to track my progress systematically. Using a digital weight log combined with occasional blood sugar monitoring helped me understand how my body responded to both the medication and lifestyle changes. It was fascinating to see patterns emerge — like appetite fluctuations tied to certain meals or activity levels — which guided adjustments in my routine.
Weekly reviews with my doctor transformed data into actionable insights. This dynamic feedback loop prevented discouragement from plateaus and allowed for timely tweaks in dosing and diet. For anyone embarking on a similar path, embracing data-driven tracking can turn weight loss from a frustrating guessing game into a manageable, informed process.
Have You Ever Wondered How Integrating Mindfulness Could Enhance Your Ozempic Experience?
Stress and sleep quality are often overlooked factors that profoundly impact weight management. Personally, incorporating mindfulness practices and prioritizing restful sleep made a noticeable difference. When stress levels were high, my cravings intensified, and weight loss stalled despite medication adherence. Mindfulness-based stress reduction techniques helped me regain control over emotional eating triggers.
Moreover, experts point out that poor sleep disrupts hormones critical for appetite regulation, undermining pharmacological efforts like Ozempic (NCBI study on sleep and weight). This holistic perspective encourages combining medication with lifestyle strategies addressing mental and physical well-being.
Practical Tips From My Experience With Ozempic
- Communicate openly with your healthcare provider about side effects and progress.
- Embrace gradual dose increases to minimize discomfort.
- Incorporate balanced meals rich in fiber and protein to support appetite control.
- Stay hydrated and adjust meal timing to ease gastrointestinal symptoms.
- Integrate moderate physical activity you enjoy to boost metabolism.
- Use tracking tools to monitor patterns and celebrate milestones.
- Explore mindfulness and stress reduction techniques to support emotional balance.
If you’re considering Ozempic or already on this journey, I invite you to share your experiences or questions in the comments below. Your stories can inspire others and create a community of support. Also, feel free to explore expert-led Ozempic treatment plans that offer personalized care tailored to your lifestyle.
Decoding the Pharmacokinetics of Ozempic: How Timing and Dosage Impact Weight Loss Efficacy
Understanding the intricate pharmacokinetics of Ozempic (semaglutide) is crucial for tailoring treatment that maximizes weight loss while minimizing adverse effects. Ozempic’s long half-life—approximately 7 days—allows for once-weekly dosing, but individual metabolic rates, renal function, and injection timing can influence drug plasma levels and, consequently, therapeutic outcomes. Expert clinicians emphasize that dose titration schedules must consider these pharmacodynamic nuances to sustain appetite suppression without triggering excessive gastrointestinal distress.
For example, administering Ozempic on the same day each week stabilizes steady-state concentrations, reducing variability that can affect hunger signals and glycemic control. Moreover, dose escalation is ideally staggered over several weeks—commonly starting at 0.25 mg for four weeks before increasing to 0.5 mg and potentially up to 1 mg or higher depending on patient response. This graduated approach aligns with the drug’s receptor binding dynamics, optimizing satiety pathways in the hypothalamus and gut-brain axis.
What are the Advanced Clinical Indicators Used to Personalize Ozempic Dosage Beyond Standard Protocols?
Beyond weight and HbA1c levels, cutting-edge personalization incorporates biomarkers such as fasting insulin, C-peptide levels, and even genetic polymorphisms affecting GLP-1 receptor sensitivity. For instance, patients with insulin resistance characterized by elevated HOMA-IR scores may require more aggressive titration combined with adjunct metabolic therapies. Additionally, continuous glucose monitoring (CGM) data provide real-time feedback on glycemic excursions, informing dynamic dose adjustments to optimize weight loss without compromising safety.
Clinicians also assess patient-reported outcomes, including satiety scales and gastrointestinal tolerance, to individualize regimens effectively. This integrative biomarker and behavioral data approach transcends one-size-fits-all dosing, embodying precision medicine principles that elevate Ozempic efficacy in complex metabolic profiles (source: PubMed Central on GLP-1 pharmacogenomics).
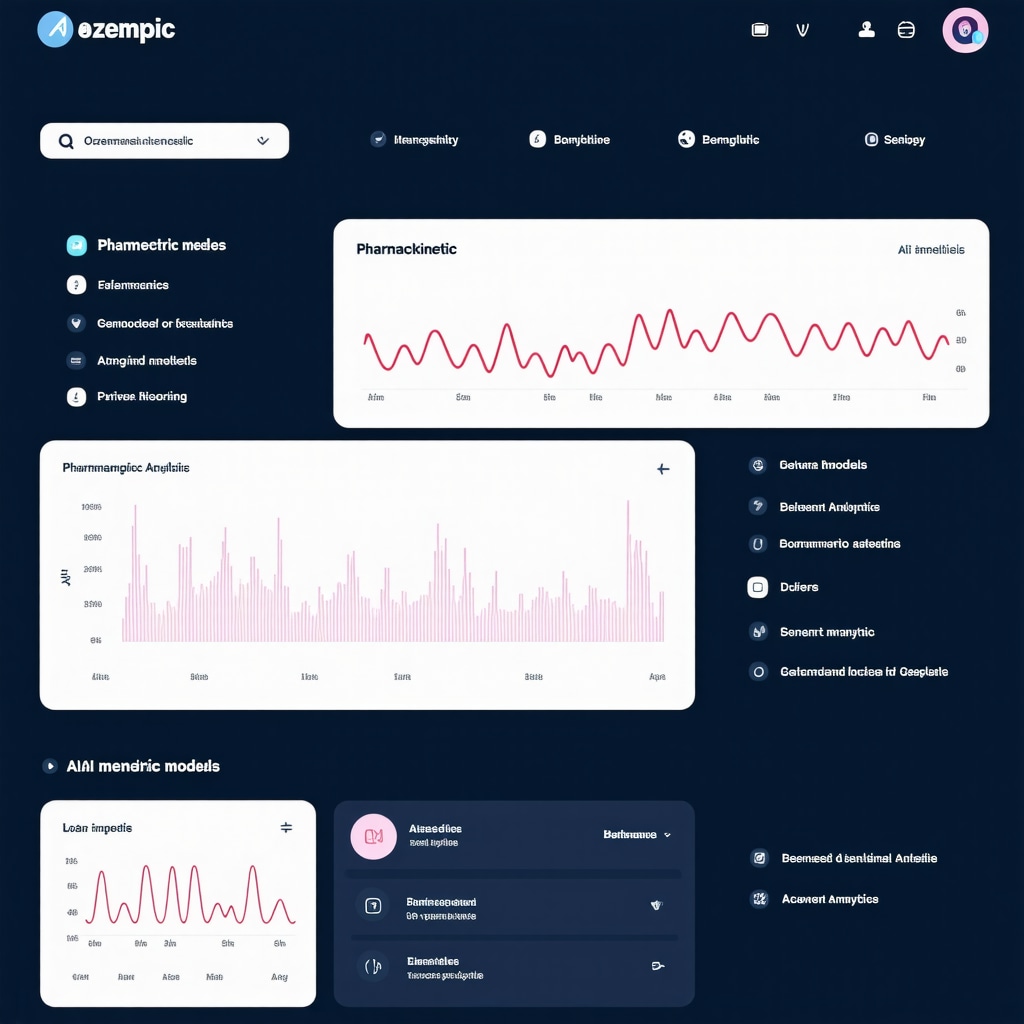
Harnessing Digital Health Platforms: The Future of Ozempic Weight Loss Monitoring
Digital health innovations are revolutionizing how patients and providers engage with Ozempic therapy. Mobile apps integrated with smart scales, dietary trackers, and symptom diaries provide granular insights into daily fluctuations in appetite, mood, and physical activity. These platforms facilitate asynchronous communication, enabling clinicians to intervene promptly when side effects arise or plateaus occur.
Machine learning algorithms analyze longitudinal data streams to predict weight loss trajectories and identify behavioral patterns that correlate with success or failure. For example, early detection of declining adherence or rising hunger signals can trigger automated motivational prompts or clinician outreach. This proactive model transforms passive treatment into an interactive, adaptive journey tailored to each patient’s evolving needs.
Integrative Nutraceuticals and Complementary Therapies: Enhancing Ozempic’s Mechanistic Synergy
Emerging research suggests that certain nutraceuticals may potentiate Ozempic’s weight loss effects by modulating overlapping metabolic pathways. For instance, supplements like berberine and omega-3 fatty acids exhibit insulin-sensitizing and anti-inflammatory properties that complement GLP-1 receptor activation. Additionally, probiotics targeting gut microbiota composition may enhance the gut-brain axis signaling, further amplifying appetite regulation.
Complementary therapies such as acupuncture and vagal nerve stimulation are under investigation for their potential to influence autonomic pathways involved in hunger and satiety. While these adjuncts require more robust clinical validation, they represent promising avenues for comprehensive, multi-modal weight management strategies integrated with pharmacotherapy.
Addressing Complex Patient Scenarios: Tailoring Ozempic Use in Comorbid Conditions
Patients with multifaceted health profiles—such as those with concomitant cardiovascular disease, chronic kidney disease, or psychiatric disorders—necessitate nuanced Ozempic management approaches. For example, in cardiovascular risk reduction, Ozempic’s benefits extend beyond glycemic control to include improved lipid profiles and blood pressure modulation, but dosing must be cautiously optimized to avoid hypotension or renal stress.
Moreover, psychiatric comorbidities like depression or anxiety may influence treatment adherence and appetite regulation, requiring integrated behavioral health support. Collaborative care models involving endocrinologists, cardiologists, and mental health professionals ensure that Ozempic therapy is harmonized within the broader therapeutic context, maximizing safety and efficacy.
How Can Ozempic Therapy Be Safely Integrated in Patients with Complex Multimorbidity Without Compromising Outcomes?
Expert consensus recommends comprehensive baseline assessments including renal function tests, cardiac evaluation, and mental health screenings. Close monitoring during titration phases allows for early detection of adverse interactions or symptom exacerbations. Utilizing multidisciplinary teams ensures that pharmacologic and non-pharmacologic interventions are synergistically aligned, tailoring Ozempic therapy to individual risk profiles and enhancing holistic health outcomes (JACC on GLP-1 receptor agonists in cardiovascular disease).
For those navigating the complexities of weight loss with comorbidities, engaging with expert-led, personalized Ozempic programs provides a pathway to optimized care and sustained success.
If you’re serious about transcending standard weight loss approaches, consider consulting specialized clinics offering comprehensive Ozempic management strategies tailored to your unique metabolic and health landscape.
Deciphering Patient Variability: Genetic and Metabolic Nuances Influencing Ozempic Response
Recent advancements in pharmacogenomics have illuminated how genetic polymorphisms modulate GLP-1 receptor sensitivity, thereby affecting individual responsiveness to Ozempic. Variants in genes such as GLP1R and TCF7L2 contribute to heterogeneity in treatment outcomes, necessitating precision medicine tactics that transcend conventional dosing paradigms. Metabolic factors like hepatic steatosis and adipose tissue distribution further complicate therapeutic efficacy, underscoring the need for comprehensive metabolic phenotyping when designing personalized weight loss regimens.
Innovative Monitoring Technologies: Harnessing AI-Driven Analytics for Real-Time Therapeutic Optimization
Artificial intelligence-powered platforms are revolutionizing Ozempic management by integrating multifactorial datasets, including biometric, behavioral, and pharmacokinetic parameters. Predictive modeling algorithms facilitate anticipatory adjustments in dosing schedules, preemptively mitigating side effects such as gastrointestinal discomfort and glycemic variability. This dynamic, data-centric approach empowers clinicians to refine interventions continuously, thereby sustaining weight loss momentum and enhancing patient adherence.
What Are the Latest Evidence-Based Protocols for Combining Ozempic with Emerging Metabolic Modulators?
Contemporary clinical trials are investigating synergistic regimens pairing Ozempic with novel agents like dual GIP/GLP-1 receptor agonists (e.g., tirzepatide) and SGLT2 inhibitors to amplify metabolic benefits. These combination therapies aim to target complementary pathways governing appetite, insulin sensitivity, and energy expenditure. Expert consensus emphasizes meticulous titration and vigilant monitoring to balance efficacy with tolerability, particularly in populations with complex comorbidities. For detailed insights, refer to the New England Journal of Medicine review on metabolic combination therapies.
Integrating Psychoneuroendocrinology Insights: Addressing Neurohormonal Drivers of Weight Regain
Weight recidivism remains a formidable challenge in Ozempic treatment courses, often driven by neurohormonal adaptations such as leptin resistance and hypothalamic inflammation. Cutting-edge interventions incorporating cognitive-behavioral therapy alongside pharmacotherapy are demonstrating promise in modulating hypothalamic-pituitary-adrenal axis dysregulation. This integrative model facilitates sustainable behavior change by attenuating stress-induced hyperphagia and optimizing neuroendocrine milieu to support pharmacologic appetite suppression.
Strategizing Long-Term Maintenance: Transitioning from Pharmacotherapy to Lifestyle Autonomy
As patients approach weight loss stabilization, transitioning from Ozempic dependence to autonomous lifestyle management is critical. Structured tapering protocols combined with ongoing behavioral support mitigate rebound weight gain risks. Emphasis on nutritional resilience, physical activity habituation, and psychosocial reinforcement fosters durable metabolic adaptations. Expert-led maintenance programs often incorporate periodic pharmacologic boosters aligned with biomarker feedback to sustain outcomes.
The Role of Gut Microbiome Modulation in Enhancing Ozempic’s Weight Loss Mechanisms
Emerging evidence implicates the gut microbiota as a pivotal modulator of GLP-1 activity and systemic metabolism. Prebiotic and probiotic interventions tailored to enrich short-chain fatty acid-producing bacterial strains can potentiate Ozempic-induced satiety and glycemic control. Personalized microbiome profiling enables targeted dietary and supplement strategies that complement pharmacotherapy, representing a frontier in integrative obesity management.
Are you ready to elevate your weight loss strategy through these advanced, evidence-backed approaches? Engage with expert clinicians who integrate cutting-edge science and personalized care to revolutionize your Ozempic experience.
Frequently Asked Questions (FAQ)
What is Ozempic and how does it aid weight loss?
Ozempic is a prescription medication containing semaglutide, a GLP-1 receptor agonist originally developed for type 2 diabetes. It facilitates weight loss by suppressing appetite through central nervous system pathways, slowing gastric emptying, and enhancing insulin sensitivity, thereby reducing caloric intake and improving metabolic efficiency.
How important is medical supervision during Ozempic therapy?
Medical supervision is critical for safe and effective Ozempic use. It guides personalized dose titration to minimize side effects, monitors metabolic responses, and integrates behavioral support to address psychological factors influencing weight loss, ensuring a tailored and sustainable treatment plan.
Can lifestyle changes enhance the effectiveness of Ozempic?
Yes. Combining Ozempic with a balanced diet rich in fiber and lean proteins, regular physical activity, stress management, and adequate sleep synergistically enhances weight loss outcomes by supporting appetite regulation, improving insulin sensitivity, and mitigating side effects.
What are common side effects and how can they be managed?
The most common side effects are gastrointestinal symptoms such as nausea, vomiting, and diarrhea. Gradual dose escalation, meal timing adjustments, hydration, and open communication with healthcare providers help mitigate these effects and improve adherence.
How does genetic variability affect Ozempic response?
Genetic polymorphisms in GLP-1 receptor and related metabolic genes influence individual responsiveness to Ozempic. Pharmacogenomic profiling allows clinicians to personalize dosing and anticipate efficacy, moving toward precision medicine in weight management.
What role do digital health technologies play in Ozempic treatment?
Digital platforms and AI-driven analytics enable real-time monitoring of weight, appetite, glycemic control, and adherence patterns. These tools facilitate dynamic dose adjustments, early identification of challenges, and enhanced patient engagement in their treatment journey.
Is Ozempic safe for patients with comorbid conditions?
With expert multidisciplinary evaluation and monitoring, Ozempic can be safely used in patients with cardiovascular disease, kidney impairment, or psychiatric disorders. Personalized regimens and integrated behavioral health support optimize outcomes while minimizing risks.
Can Ozempic be combined with other metabolic therapies?
Emerging evidence supports combining Ozempic with agents like dual GIP/GLP-1 agonists or SGLT2 inhibitors to amplify metabolic benefits. Such combinations require careful titration and monitoring to balance efficacy with tolerability.
How is long-term weight maintenance managed after Ozempic?
Maintenance involves structured tapering protocols, sustained lifestyle modifications, behavioral support, and periodic pharmacologic boosters if needed. This comprehensive approach prevents weight regain and promotes metabolic resilience.
How does gut microbiome modulation enhance Ozempic’s effects?
Targeting the gut microbiota through prebiotics and probiotics can potentiate GLP-1 activity and appetite regulation, complementing Ozempic’s pharmacodynamics and offering a promising adjunct in personalized obesity management.
Trusted External Sources
- American Diabetes Association (ADA): Provides authoritative guidelines on GLP-1 receptor agonists, including semaglutide, detailing clinical efficacy, safety profiles, and patient management strategies.
- National Institutes of Health (NIH) PubMed Central: Hosts peer-reviewed studies on pharmacogenomics, weight loss mechanisms, and integrative therapies related to Ozempic, supporting evidence-based personalization.
- Journal of the American College of Cardiology (JACC): Offers in-depth analysis of cardiovascular implications and safety considerations for GLP-1 agonists in patients with comorbid conditions.
- New England Journal of Medicine (NEJM): Features cutting-edge clinical trials on metabolic combination therapies and emerging pharmacological approaches complementing Ozempic.
- National Center for Biotechnology Information (NCBI): Provides comprehensive research on neuroendocrine and psychoneuroendocrinology factors influencing weight loss and maintenance with GLP-1 therapies.
Conclusion
Ozempic represents a paradigm shift in sustainable weight management, leveraging GLP-1 receptor agonism to effectively suppress appetite and improve metabolic health. However, its true potential is unlocked through an expert-guided, integrative approach that personalizes dosing, synergizes lifestyle modifications, and harnesses advanced monitoring technologies. Addressing genetic variability, comorbidities, and neurohormonal factors further refines treatment efficacy and safety. As digital health innovations and adjunct nutraceuticals evolve, they promise to enhance Ozempic’s therapeutic landscape. For patients and clinicians committed to transformative weight loss journeys, embracing these comprehensive strategies is essential. Engage with specialized medical teams and explore evidence-based Ozempic programs to maximize your results and sustain long-term health improvements. Share your experiences, ask questions, and delve into related expert content to empower your weight loss success today.


What struck me most from this detailed guide is the emphasis on the combination of Ozempic therapy with personalized medical supervision and lifestyle changes. From my experience helping friends navigate similar weight loss treatments, medication by itself rarely leads to lasting success. The idea of integrating behavioral counseling and mindfulness, along with consistent tracking of progress, really resonates. I believe this holistic approach can help people stay motivated and overcome the common barriers like side effects or plateaus.
I’m curious whether others have found digital tracking tools, like apps or wearable devices, indispensable in managing their Ozempic journey? The post discusses AI-driven analytics and data-driven dose adjustments—have you noticed a clear difference in results when using these technologies compared to more traditional monitoring? Also, balancing moderate exercise with dietary changes while handling side effects can feel tricky; what are some of your practical strategies that helped keep you consistent without feeling overwhelmed? Insights from personal stories could really enrich our shared understanding of what works best alongside Ozempic.
I completely agree that medical supervision is a cornerstone in successfully navigating Ozempic treatment. Based on my experience, the gradual dose titration under professional guidance not only minimizes nausea and other GI side effects but also instills confidence to stick with the therapy long-term. Regarding the question about digital tracking tools, I’ve found that integrating wearable devices and apps provides invaluable insights that simply weren’t accessible before. For instance, tracking daily activity alongside meal logging helped me and my clinician identify specific patterns where appetite spikes aligned with stress or low sleep quality—which the post highlights as critical factors. This data allowed for precise behavioral adjustments and even medication timing tweaks. I do think, however, that one challenge remains balancing consistent moderate exercise with side effects, especially when those side effects can sap energy. Personally, I found that low-impact activities like swimming or yoga were sustainable ways to stay active without overwhelming my system. Has anyone else found particular exercise routines or timing strategies that mesh well with their Ozempic treatment? Additionally, how do others manage the psychological aspects, like stress-induced cravings, alongside these data-driven approaches? Sharing these nuances might help deepen our collective understanding.
This post really highlights how essential personalized medical supervision and lifestyle integration are when using Ozempic for weight loss. I’ve read that the pharmacokinetics of semaglutide, especially its long half-life, means that timing your injections consistently is crucial to maintaining steady plasma levels. In my experience, working closely with a healthcare provider to tailor the dosing schedule and monitor biomarkers like fasting insulin has made a significant difference in outcomes. Also, tracking appetite and energy fluctuations through digital apps helped me identify patterns that guided my diet and activity adjustments effectively. I found that moderate exercises, like brisk walking or swimming, were sustainable even during some of the nausea phases, especially when done at times that didn’t interfere with my digestion. Have others found particular times of day or types of activity that work best for them during the initial titration phase? Moreover, with so many advanced tools available, do you think that integrating AI-driven data analysis can really boost long-term adherence and success, or does it sometimes add a layer of complication? Interested to hear your thoughts—especially from those who’ve experienced both approaches.
I really appreciate the detailed emphasis on combining Ozempic therapy with personalized supervision and lifestyle changes. From what I have observed, the personalized dose titration process is crucial not just in reducing side effects but also in building patient trust and commitment to the treatment plan. One aspect that particularly stands out is the use of data-driven tracking — not just for weight but also for appetite and metabolic markers. This proactive monitoring helps identify not only plateaus but subtle shifts in the body’s response, enabling timely adjustments.
In my own experience supporting a family member, integrating mindfulness and stress reduction techniques was invaluable. Stress often triggered emotional eating episodes that no medication alone could control. It showed me how a holistic approach addressing psychological and physiological factors works better than any single intervention.
That being said, I wonder about the practical challenges some people face when trying to juggle lifestyle changes alongside the common gastrointestinal side effects of Ozempic. Has anyone found effective ways to maintain consistent physical activity when nausea or fatigue strike? Also, how do you balance rigorous tracking without feeling overwhelmed or obsessed? It would be great to hear about practical, sustainable strategies that others have employed to stay consistent and motivated throughout the journey.