Why Everyone’s Talking About Ozempic in the Weight Loss World
Step into any health forum, scroll through social media, or chat with your neighbor and you’ll hear whispers—no, more like shouts—about Ozempic. This GLP-1 weight loss drug has become the darling of fat loss conversations, stealing the spotlight from other contenders. But why exactly does Ozempic dominate in this crowded arena? Let’s peel back the curtain on this injectable superstar.
Not All GLP-1s Are Created Equal: The Ozempic Edge
GLP-1 receptor agonists, a fancy term for a class of drugs that mimic a gut hormone to control appetite and blood sugar, have surged in popularity for weight management. Yet, among them, Ozempic (semaglutide) stands tall. It’s not just the marketing muscle—Ozempic boasts a proven track record of significant fat loss and improved metabolic health.
Patients report a remarkable reduction in cravings and a feeling of fullness that genuinely changes their relationship with food. Unlike some weight loss drugs that feel like a rollercoaster, Ozempic offers a smoother ride with once-weekly dosing, making it a favorite for those seeking convenience alongside effectiveness.
Is It Just Hype, or Does Ozempic Really Outperform the Competition?
Great question. Clinical trials and real-world patient stories consistently show Ozempic’s superiority in curbing appetite and promoting fat loss compared to other GLP-1 options. A pivotal study published in The New England Journal of Medicine highlighted weight reductions averaging nearly 15% of body weight over 68 weeks—a game-changer in obesity treatment.
So, it’s not just smoke and mirrors; Ozempic’s fat-burning credentials are backed by serious science.
From Clinical Trials to Real Life: The Ozempic Journey
What’s truly fascinating is how patients feel during and after treatment. Many share transformative stories, noting how Ozempic helped break through stubborn weight plateaus and empowered healthier lifestyle choices. For those curious about the journey, real patient transformations offer inspiring proof that this drug isn’t magic—it’s medicine working hand-in-hand with commitment.
Thinking about jumping on the Ozempic bandwagon? It’s wise to explore doctor-supervised programs which ensure safe and effective use tailored to your health profile.
Ready to Share Your Ozempic Story or Curious to Learn More?
Weight loss journeys are deeply personal, and Ozempic’s rise has sparked a vibrant community eager to share insights and experiences. Have you tried Ozempic or another GLP-1 drug? Drop your thoughts below or dive into our repository of expert tips and patient stories to fuel your knowledge and motivation.
Tailoring Ozempic Dosage for Maximum Fat Loss: The Physician’s Art
While Ozempic’s once-weekly injection schedule offers convenience, the magic truly lies in personalized dosing strategies. Physicians often begin treatment with a low starting dose to minimize side effects and gradually increase it, optimizing fat loss while prioritizing patient safety. This nuanced approach ensures that weight loss is sustainable, and patients maintain a positive experience throughout their journey.
Adjusting the dose isn’t a one-size-fits-all game; it requires continual monitoring and patient feedback. For a detailed guide on how providers fine-tune Ozempic dosing for best results, explore physician-prescribed Ozempic dosage tips. This resource underscores how tailored care can dramatically improve outcomes and reduce adverse effects.
Managing Side Effects: A Crucial Component of Successful Weight Loss
Although Ozempic is remarkably effective, side effects like nausea, vomiting, and constipation can deter adherence. Understanding these reactions and employing expert management techniques enable patients to stay on track. For example, gradual dose escalation and timing injections with meals are practical tactics clinicians recommend.
Clinicians also emphasize the importance of open communication to promptly address any discomfort. This collaborative approach between patient and provider fosters adherence and long-term success, as detailed in navigating Ozempic side effects in weight loss programs.
What Are the Latest Innovations in Ozempic Weight Loss Programs for 2024?
As the weight loss landscape evolves, so do the strategies incorporating Ozempic. Recent advancements include integrating telehealth platforms for remote monitoring, combining Ozempic with personalized nutrition plans, and utilizing digital tools to track progress beyond the scale. Clinics offering these advanced programs emphasize customization, addressing not just weight but holistic metabolic health.
For instance, advanced Ozempic weight loss programs deliver personalized plans that dynamically adapt to patient responses, incorporating behavioral coaching and lifestyle modifications. This multi-faceted approach leverages Ozempic’s pharmacological benefits alongside sustainable habits.
Evidence-Based Insights: What Trusted Research Says
According to a comprehensive review published in The Lancet Diabetes & Endocrinology, semaglutide (the active ingredient in Ozempic) stands out for its efficacy in inducing significant weight loss with a favorable safety profile. The review highlights that patient-centered dosing and side effect management are key drivers of treatment success, reinforcing the clinical strategies discussed above.
This authoritative source further cements Ozempic’s role as a cornerstone in modern obesity management, emphasizing that thoughtful clinical application maximizes benefits while mitigating risks.
Join the Ozempic Conversation: Share Your Experience or Explore More
Have you embarked on the Ozempic journey or are considering it? Your insights could illuminate the path for others navigating this weight loss avenue. Share your experiences or questions in the comments below, and if you’re eager to deepen your understanding, visit our clinician’s guide to prescription weight loss with Ozempic to explore expert advice and patient success stories.
Precision Tuning: How Experts Customize Ozempic Dosing to Unlock Peak Fat Loss
The journey to optimal weight loss with Ozempic transcends the simple act of following a prescribed dose. Seasoned clinicians recognize that metabolic individuality demands a tailored approach, meticulously adjusting the semaglutide dose based on patient-specific factors such as insulin sensitivity, gastrointestinal tolerance, and baseline appetite regulation. This dynamic titration process often involves incremental dose escalations beyond standard protocols under close supervision to harness the full anorectic potential of Ozempic without tipping into intolerable side effects.
For patients presenting with insulin resistance or metabolic syndrome, some physicians employ a strategy of dose intensification combined with adjunctive lifestyle counseling, creating a synergistic effect that magnifies fat loss. Conversely, those with heightened susceptibility to gastrointestinal discomfort may benefit from a slower titration schedule paired with antiemetic strategies—highlighting the necessity for personalized regimens rather than a “one-size-fits-all” methodology.
Integrating Ozempic with Emerging Metabolic Therapies: A Multi-Modal Approach
Recent clinical discourse increasingly explores combining Ozempic with other metabolic interventions such as low-dose amylin analogs or SGLT2 inhibitors, aiming to address complex pathophysiologies underlying obesity. Such combination therapies are still in investigational phases but show promise in potentiating weight loss outcomes by targeting complementary hormonal pathways.
Moreover, integrating Ozempic treatment with cutting-edge digital therapeutics—ranging from AI-driven diet monitoring apps to wearable devices tracking metabolic biomarkers—enables a real-time feedback loop. This empowers patients and clinicians to adapt interventions responsively, enhancing adherence and efficacy.
How Does Semaglutide Influence Central Nervous System Appetite Regulation Beyond Peripheral Effects?
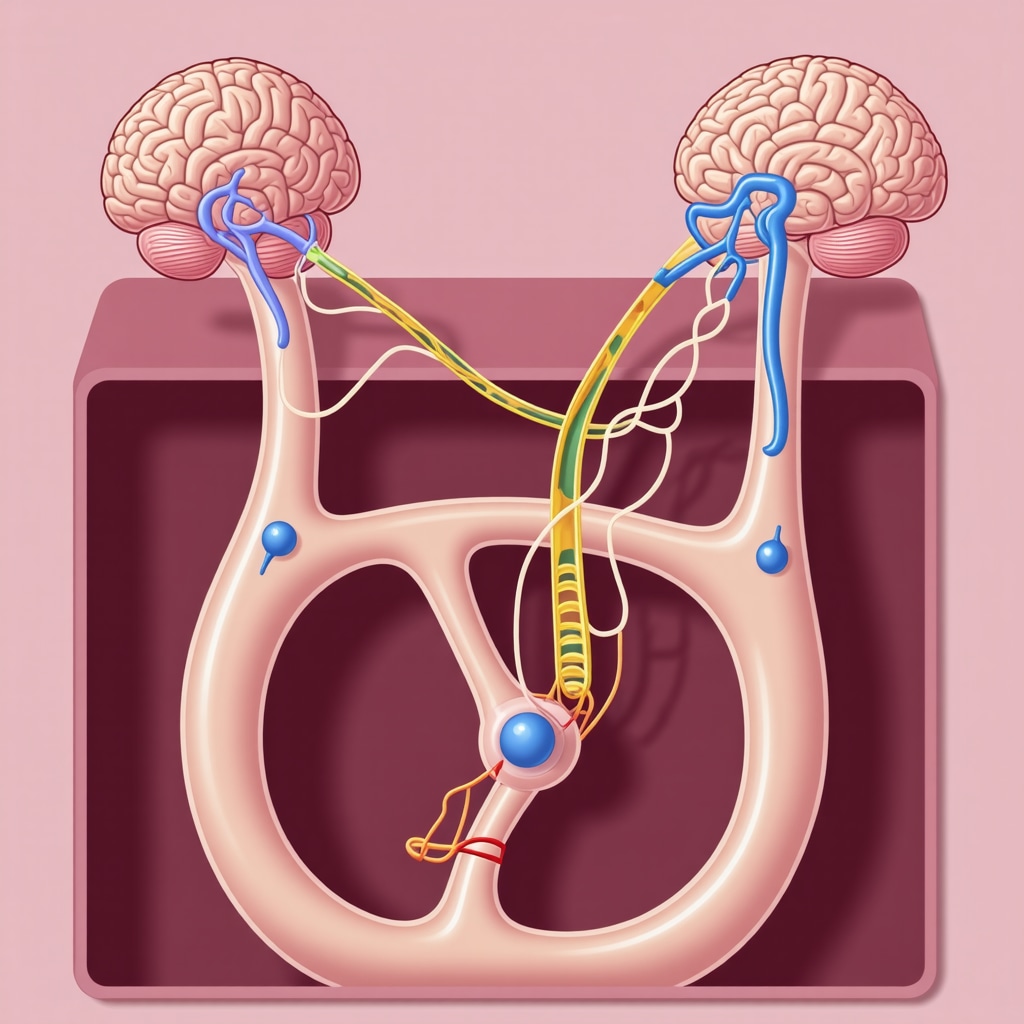
Semaglutide’s mechanism of action extends into the central nervous system, where it modulates key hypothalamic nuclei involved in hunger and satiety signaling. By crossing the blood-brain barrier, semaglutide binds GLP-1 receptors in the arcuate nucleus, triggering neuronal pathways that reduce orexigenic neuropeptides and enhance anorexigenic signals. This dual peripheral and central modulation distinguishes Ozempic from older weight loss agents that primarily exert peripheral effects.
Understanding this neuroendocrine interaction is critical for clinicians, as it explains the drug’s ability to recalibrate dysfunctional appetite networks often seen in obesity—offering a biologically grounded rationale for its sustained efficacy.
For a comprehensive neuropharmacological overview, see the detailed analysis published in Nature Reviews Endocrinology, which elaborates on semaglutide’s central nervous system actions and clinical implications.
Addressing Patient Concerns: Long-Term Safety and Sustainable Weight Maintenance
While Ozempic’s efficacy in initial weight reduction is well-documented, patients frequently inquire about the sustainability of results and long-term safety profiles. Current longitudinal studies suggest that continued semaglutide administration is necessary to maintain weight loss, as cessation often leads to weight regain, underscoring the chronic nature of obesity management.
Concerns regarding pancreatic and thyroid safety have been extensively studied, with large-scale data showing no significant increased risk when dosing is carefully managed. Nonetheless, vigilant monitoring remains a cornerstone of therapy, particularly in patients with preexisting pancreatic or thyroid conditions.
Engage with Expert Resources to Elevate Your Ozempic Experience
Delving deeper into the nuances of Ozempic therapy can dramatically improve outcomes. If you’re considering or currently on Ozempic, we encourage you to consult specialized clinician resources and participate in patient forums where advanced dosing strategies and real-world experiences are shared.
For personalized guidance and to explore the latest research-driven protocols, visit our Advanced Ozempic Strategies & Expert Insights page and join a community committed to mastering the science of sustainable weight loss.
Decoding Semaglutide’s Central Nervous System Mastery: Beyond Peripheral Appetite Suppression
While Ozempic’s ability to reduce appetite and improve glycemic control is well-recognized, its profound impact on the brain’s hunger circuits reveals a sophisticated neuroendocrine choreography. Semaglutide crosses the blood-brain barrier to engage GLP-1 receptors within the hypothalamic arcuate nucleus, a pivotal center orchestrating energy balance. This interaction suppresses orexigenic neuropeptides like neuropeptide Y and agouti-related peptide, while enhancing anorexigenic signals such as pro-opiomelanocortin, effectively recalibrating dysfunctional appetite pathways commonly altered in obesity.
This central nervous system modulation accounts for Ozempic’s sustained appetite suppression and distinguishes it from older peripheral-acting agents, underpinning its superior clinical outcomes. Understanding these mechanisms is critical for clinicians tailoring treatment to patients facing complex metabolic challenges.
For a detailed neuropharmacological exploration, see the comprehensive review in Nature Reviews Endocrinology, which elucidates semaglutide’s CNS actions and their implications for obesity therapy.
How Can Integrative Digital Tools Amplify Ozempic’s Effectiveness in Personalized Weight Management?
The convergence of pharmacotherapy and digital health is reshaping weight loss paradigms. Advanced telehealth platforms now enable continuous remote monitoring of patient adherence, side effects, and metabolic markers, facilitating dynamic dose adjustments and behavioral interventions tailored in real-time.
Complementary AI-driven nutrition apps and wearable biosensors empower patients to visualize progress and receive personalized feedback, reinforcing motivation and lifestyle adherence. Such integration transforms Ozempic treatment from a static regimen into a responsive, patient-centered journey.
Exploring these innovations further, telehealth Ozempic prescriptions offer a glimpse into how modern technology elevates clinical care and patient engagement.
Expert Voices: Navigating Long-Term Safety and Maintenance Strategies with Ozempic
Long-term weight maintenance remains a pivotal concern in obesity management. Experts emphasize that sustained use of semaglutide is often necessary to preserve fat loss, given the chronic and relapsing nature of obesity as a metabolic disease.
Safety data from extensive cohorts reveal no significant increase in pancreatic or thyroid adverse events under careful clinical oversight, reassuring both clinicians and patients. Nevertheless, individualized risk monitoring and open dialogue remain paramount to preempt complications and optimize adherence.
Clinicians recommend combining Ozempic therapy with behavioral counseling and periodic metabolic assessments to reinforce durable lifestyle changes, minimizing risk of weight regain after dose tapering or discontinuation. For comprehensive guidance, consult our clinician’s guide to prescription weight loss with Ozempic.
Join the Conversation: Share Your Advanced Insights or Questions on Ozempic’s Evolving Role
Ozempic’s growing prominence invites ongoing dialogue among patients, clinicians, and researchers. Have you integrated digital tools with your Ozempic regimen or navigated complex dosing challenges? Your expertise and experiences can enrich this community’s collective knowledge.
Drop your comments below or connect with us via contact us to explore tailored support and expert resources. Together, we can unlock new frontiers in precision weight management.
Expert Insights & Advanced Considerations
Precision Dosing Is the Cornerstone of Effective Ozempic Therapy
Clinicians emphasize that individualized dose titration based on metabolic markers, gastrointestinal tolerance, and patient feedback is critical to unlocking Ozempic’s full fat loss potential while minimizing side effects. This nuanced personalization distinguishes successful long-term outcomes from transient results.
Integrating Digital Health Tools Enhances Patient Engagement and Treatment Success
Combining Ozempic with telehealth monitoring, AI-driven nutrition apps, and wearable biosensors creates a dynamic feedback ecosystem. This allows real-time adjustments and behavioral coaching that reinforce adherence and optimize weight management beyond pharmacology alone.
Semaglutide’s Central Nervous System Effects Redefine Appetite Regulation Models
Beyond peripheral GLP-1 receptor activation, semaglutide modulates hypothalamic pathways to suppress orexigenic neuropeptides and enhance satiety signals. This dual mechanism explains its superior and sustained appetite control compared to older agents acting peripherally.
Long-Term Therapy and Multimodal Approaches Are Essential for Sustainable Weight Management
Obesity’s chronic nature necessitates continued Ozempic administration alongside lifestyle and behavioral interventions. Emerging combination therapies targeting complementary metabolic pathways are promising future directions for comprehensive treatment.
Expert Communication and Side Effect Management Drive Adherence
Open dialogue regarding nausea, constipation, or other side effects and strategic dose escalation protocols empower patients to maintain therapy, crucial for achieving and sustaining clinically meaningful fat loss.
Curated Expert Resources
- The Lancet Diabetes & Endocrinology Review: An authoritative source detailing semaglutide’s efficacy and safety profile, pivotal for understanding clinical applications (link).
- Nature Reviews Endocrinology Neuropharmacology Overview: A comprehensive analysis of semaglutide’s central nervous system mechanisms, enriching clinician insight (link).
- Physician-Prescribed Ozempic Guidelines: Practical strategies for safe and effective dosing tailored to patient needs.
- Managing Ozempic Side Effects: Evidence-based approaches to enhance adherence through side effect mitigation.
- Telehealth Ozempic Prescriptions: Insights on leveraging digital health for improved treatment outcomes.
Final Expert Perspective
Ozempic’s ascendancy in medical weight loss is no accident; it reflects a sophisticated interplay of pharmacology, neuroscience, and personalized medicine. Understanding semaglutide’s central and peripheral actions alongside tailored dosing strategies and integrative digital tools equips clinicians and patients to optimize fat loss sustainably. As weight management evolves, embracing these evidence-based insights ensures Ozempic’s role as a cornerstone therapy is both effective and enduring.
We invite healthcare professionals and informed patients alike to engage with these advanced perspectives, share experiences, and explore our clinician’s guide to prescription weight loss with Ozempic for deeper expertise. Together, we can advance precision obesity care to new heights.

