Why Ozempic Is the Talk of the Town in Medical Weight Loss Circles
Ever stumbled upon a weight loss solution that feels like it’s more science fiction than science fact? Ozempic, a GLP-1 receptor agonist originally designed for type 2 diabetes, has been stealing the spotlight for its surprising prowess in medical weight loss programs. But what makes this injectable medication a game-changer for sustainable weight management? Let’s dive into this fascinating narrative that’s reshaping how we think about fat loss.
From Blood Sugar to Body Fat: The Unexpected Journey of Ozempic
Ozempic’s journey from a diabetes drug to a weight loss superstar is a testament to the evolving landscape of medical treatments. By mimicking the body’s natural hormones that regulate appetite and digestion, Ozempic helps curb hunger, leading to fewer calories consumed without the usual battle of willpower. This hormone-based approach synergizes beautifully with medically supervised weight loss programs, creating an environment where the body and mind align toward healthier habits.
Could Ozempic Be the Missing Link in Long-Term Weight Loss Success?
Here’s the rub: many fad diets and quick fixes falter because they don’t address the underlying biological drivers of appetite and metabolism. Ozempic, on the other hand, steps directly into those biological conversations. It slows gastric emptying and modulates insulin response, making the process of losing weight feel less like punishment and more like a natural recalibration. This is why medical weight loss clinics emphasize physician-prescribed Ozempic treatments as a cornerstone of sustainable programs.
Real Talk: What Does the Research Say?
According to a landmark study published in the New England Journal of Medicine, patients using Ozempic showed significant weight loss compared to placebo, with improved cardiovascular markers. This isn’t just about shedding pounds; it’s about enhancing overall health metrics, which is the holy grail for medical weight loss programs aiming for sustainability rather than quick fixes.
Putting Ozempic Into the Mix: A Clinician’s Perspective
Integrating Ozempic effectively requires more than just a prescription. It involves tailored nutrition plans, coaching, and regular monitoring to manage side effects and maximize results. Clinics offering doctor-supervised Ozempic treatments provide this holistic framework, ensuring patients don’t just lose weight but keep it off. This multidisciplinary approach is the secret sauce behind sustainable success stories.
Thinking Beyond the Scale: How Does Ozempic Change the Weight Loss Mindset?
It’s not just about numbers on a scale; it’s about rewriting the story we tell ourselves about food, hunger, and control. Ozempic gives patients a fighting chance to break free from the cycle of cravings and emotional eating, fostering a healthier relationship with food. When paired with behavioral support, it’s a one-two punch that transforms both body and mindset.
Curious about how Ozempic could fit into your own journey? Don’t just take my word for it—explore detailed guides on prescription weight loss with Ozempic and discover firsthand accounts and expert advice that can illuminate your path.
So, what are your thoughts? Have you or someone you know experienced the Ozempic effect? Share your stories and questions below—let’s get the conversation rolling!
Addressing Common Concerns: How Safe Is Ozempic for Long-Term Use?
One of the most pressing questions for patients and clinicians alike is the safety profile of Ozempic during extended treatment periods. While the medication offers promising weight loss benefits, understanding potential side effects and managing them proactively is crucial. Research indicates that common adverse effects include gastrointestinal symptoms such as nausea, vomiting, and diarrhea, which tend to diminish over time as the body adapts. More serious concerns, although rare, involve pancreatitis and thyroid C-cell tumors, underscoring the importance of thorough medical supervision throughout treatment.
Medical weight loss clinics that provide doctor-supervised Ozempic treatments emphasize the necessity of personalized dosing schedules and ongoing monitoring to mitigate risks and enhance patient safety. This tailored approach ensures each patient’s unique health status guides their therapeutic journey, optimizing outcomes while minimizing complications.
The Synergy of Ozempic and Lifestyle: Why Medication Alone Isn’t Enough
Ozempic’s pharmacological effects create a powerful foundation, but sustainable weight loss demands more than medication. Integrating a balanced diet, regular physical activity, and behavioral support forms the pillars of an effective program. Research from the National Institutes of Health highlights how combining GLP-1 receptor agonists with lifestyle interventions yields superior weight loss outcomes compared to medication alone.
Clinicians often recommend structured meal planning and exercise regimens alongside Ozempic therapy to reinforce metabolic benefits and promote muscle preservation. This comprehensive strategy addresses the multifactorial nature of obesity, tackling hormonal imbalances, energy expenditure, and psychological factors simultaneously.
What Emerging Trends Are Shaping the Future of Ozempic-Based Weight Loss?
As we look ahead, the integration of telehealth services and personalized medicine is revolutionizing how patients access and benefit from Ozempic. Telehealth platforms streamline prescription management and provide continuous support, making treatment more accessible and convenient. Furthermore, advances in pharmacogenomics may soon enable clinicians to predict individual responses to Ozempic, further customizing therapy for maximal efficacy.
For readers intrigued by this evolving landscape, exploring telehealth Ozempic prescriptions offers insight into how technology is enhancing patient care and adherence. Meanwhile, understanding the nuances of safe dosage practices remains pivotal as more individuals embark on this transformative journey.
We’d love to hear your experiences or questions about integrating Ozempic into weight loss plans. Share your thoughts or suggestions for topics you’d like us to cover—your insights help build a knowledgeable and supportive community!
Decoding the Pharmacodynamics of Ozempic: Beyond Appetite Suppression
While Ozempic’s primary mechanism as a GLP-1 receptor agonist centers on appetite regulation and delayed gastric emptying, recent studies reveal a more intricate pharmacodynamic profile. It modulates central nervous system pathways, influencing reward circuits associated with food intake, thereby reducing hedonic eating behaviors that often undermine weight loss efforts. Moreover, Ozempic’s impact on insulin sensitivity and pancreatic beta-cell function contributes to improved metabolic flexibility, which is crucial for sustainable fat loss in individuals with insulin resistance.
How Does Ozempic Influence Neuroendocrine Pathways to Sustain Weight Loss?
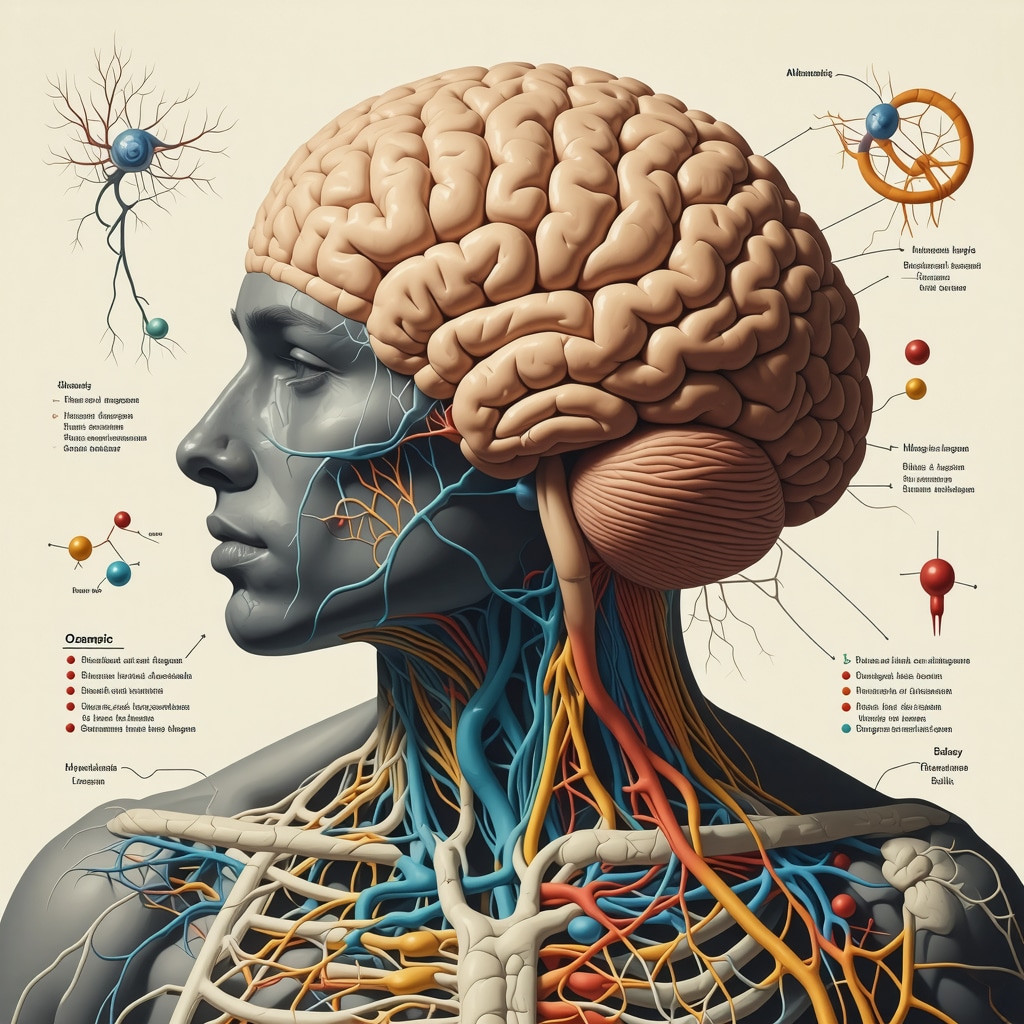
Ozempic’s action extends to the hypothalamus and brainstem, areas integral to energy homeostasis. By enhancing GLP-1 receptor signaling in these brain regions, it promotes satiety and reduces caloric intake, but it also attenuates stress-induced hyperphagia. This neuroendocrine modulation suggests that Ozempic not only suppresses physical hunger but also mitigates psychological triggers for overeating, offering a dual-pronged approach to weight control.
Personalized Dosing Strategies: Tailoring Ozempic for Optimal Efficacy and Minimal Side Effects
One size does not fit all when it comes to Ozempic dosing. Emerging clinical protocols advocate for titration schedules customized to patient metabolic profiles, comorbid conditions, and tolerance levels. Slow uptitration can minimize gastrointestinal side effects, enhancing adherence. Furthermore, integrating pharmacogenomic data enables clinicians to anticipate individual drug metabolism rates and receptor sensitivity, refining dosage for maximal therapeutic benefit.
Incorporating continuous glucose monitoring and metabolic biomarkers into patient assessments allows real-time adjustments, fostering a dynamic treatment environment. Such personalized approaches are gaining traction in cutting-edge medical weight loss clinics and are supported by evidence from recent trials published in Obesity Reviews.
Understanding Patient Variability: Why Some Respond Better to Ozempic Than Others
Inter-individual variability in response to Ozempic is influenced by genetic, environmental, and behavioral factors. Polymorphisms in GLP-1 receptor genes and differences in gut microbiota composition have been implicated in differential drug efficacy. Additionally, the presence of concurrent medications, psychological stressors, and lifestyle habits can modulate treatment outcomes.
Clinicians emphasize the importance of comprehensive baseline assessments encompassing genomic screening, dietary patterns, and psychological profiling to predict responsiveness and customize intervention strategies. This holistic evaluation aligns with precision medicine paradigms and enhances long-term success rates.
What Role Does Gut Microbiota Play in Modulating Ozempic’s Weight Loss Effects?
Emerging research underscores the gut microbiome as a pivotal mediator of metabolic health and drug response. Ozempic may induce shifts in microbial populations that favor short-chain fatty acid production, improving insulin sensitivity and reducing systemic inflammation. Conversely, an unfavorable microbiota composition might blunt these benefits, necessitating adjunct therapies such as prebiotics or probiotics to optimize outcomes.
Integrative Approaches: Combining Ozempic with Behavioral and Nutritional Modifications for Holistic Success
Medical weight loss is most successful when pharmacotherapy is embedded within a robust framework of lifestyle changes. Cognitive-behavioral therapy (CBT) tailored to address eating behaviors, stress management, and motivation significantly enhances the efficacy of Ozempic. Nutritional counseling focused on macronutrient balance and glycemic load supports metabolic adaptations and preserves lean muscle mass during caloric restriction.
Clinics pioneering integrative models report higher patient retention and satisfaction, highlighting the necessity of multidisciplinary teams including endocrinologists, dietitians, and psychologists. This synergy ensures that weight loss transcends mere numbers and fosters enduring health improvements.
For those intrigued by advancing their understanding or embarking on an Ozempic-supported weight loss journey, exploring expert-curated resources and consulting with specialized medical weight loss professionals can illuminate personalized pathways to success. Engage with our community or reach out with your questions—expert guidance is just a conversation away.
Decoding Ozempic’s Neuroendocrine Impact: A New Paradigm in Appetite and Reward Processing
Beyond its well-known role in appetite suppression, Ozempic engages intricate neuroendocrine pathways that reshape how the brain perceives hunger and reward. By activating GLP-1 receptors in the hypothalamus and brainstem, it not only enhances satiety signals but also modulates the mesolimbic reward system, reducing the hedonic appeal of high-calorie foods. This dual mechanism is crucial for patients struggling with emotional or stress-induced eating, often a formidable barrier in long-term weight management.
Recent neuroimaging studies, such as those discussed in Neuropsychopharmacology, highlight how GLP-1 receptor agonists like Ozempic alter dopamine pathways, attenuating cravings and promoting healthier eating choices. This emerging evidence underscores Ozempic’s potential to recalibrate not just physical hunger but also the psychological drivers of overeating.
How Can Personalized Pharmacogenomics Enhance Ozempic’s Effectiveness in Diverse Patient Populations?
Inter-individual variability in Ozempic response remains a critical challenge, with genetic polymorphisms influencing receptor sensitivity and metabolic handling. Integrating pharmacogenomic profiling into clinical practice offers a promising avenue for tailoring dosing regimens and maximizing efficacy while minimizing adverse effects. For example, patients with certain GLP-1 receptor gene variants may require adjusted titration schedules or adjunct therapies to achieve optimal results.
Moreover, advances in biomarker-driven approaches facilitate real-time monitoring of metabolic responses, enabling dynamic dose adjustments. Clinics specializing in personalized Ozempic care are pioneering these strategies, marrying precision medicine with comprehensive behavioral and nutritional support.
Integrative Models: Why Combining Ozempic with Behavioral Interventions Is Imperative for Lasting Transformation
Ozempic’s pharmacodynamics set the stage, but sustainable weight loss demands a holistic approach. Embedding cognitive-behavioral therapy (CBT), mindfulness practices, and tailored nutritional plans amplifies therapeutic outcomes by addressing psychological and lifestyle factors that medication alone cannot resolve. This multidisciplinary synergy fosters resilience against relapse and reinforces positive habit formation.
Evidence from the National Institutes of Health confirms that patients receiving combined pharmacologic and behavioral interventions achieve superior weight loss maintenance compared to those relying solely on medication. This integrated model exemplifies why top-tier medical weight loss clinics prioritize a team-based approach, ensuring care extends beyond the prescription pad.
Interested in delving deeper into how to optimize your Ozempic journey with expert-backed, personalized strategies? Visit our comprehensive clinician’s guide to prescription weight loss with Ozempic and connect with a community dedicated to transformative health.
Have you explored personalized approaches or behavioral supports alongside Ozempic? Share your experiences or questions below — your insights enrich our collective understanding and inspire others on this path!
Expert Insights & Advanced Considerations
Integrating Pharmacogenomics for Personalized Ozempic Dosing
Recent advances emphasize tailoring Ozempic therapy based on genetic markers influencing GLP-1 receptor sensitivity and metabolic profiles. Utilizing pharmacogenomic data allows clinicians to optimize dosing schedules to maximize efficacy while reducing side effects, moving beyond one-size-fits-all prescriptions toward precision medicine in weight management.
Neuroendocrine Modulation Beyond Appetite Suppression
Ozempic’s impact extends to brain reward circuits, attenuating hedonic eating by modulating dopamine pathways. This dual action on physical hunger and psychological drivers is crucial for addressing emotional eating patterns, a common stumbling block in long-term weight loss success.
Synergistic Effects of Behavioral Interventions with Ozempic
Embedding cognitive-behavioral therapy and nutritional counseling alongside Ozempic enhances patient adherence and sustains metabolic adaptations. This integrative approach addresses psychological triggers and lifestyle factors, reinforcing positive habits and improving retention in medical weight loss programs.
Gut Microbiota as a Mediator of Ozempic Response
Emerging research highlights the influence of gut microbiome composition on Ozempic’s metabolic effects. Modulating microbiota through probiotics or prebiotics may optimize therapeutic outcomes, suggesting a promising adjunctive strategy in personalized weight loss regimens.
Curated Expert Resources
- New England Journal of Medicine: Landmark studies on GLP-1 receptor agonists providing robust clinical evidence on efficacy and cardiovascular benefits.
- National Institutes of Health Publications: Comprehensive reviews on integrating pharmacotherapy with behavioral and lifestyle modifications for obesity management.
- Neuropsychopharmacology Journal: Cutting-edge neuroimaging research elucidating Ozempic’s effects on brain reward pathways and appetite regulation.
- Prescription Weight Loss with Ozempic: A Clinician’s Guide: In-depth resource for medical professionals on best practices in dosing, monitoring, and behavioral integration.
- Medical Weight Loss Clinics: Personalized Ozempic Care Experience: Insights into multidisciplinary care models that maximize patient outcomes.
Final Expert Perspective
Ozempic represents a paradigm shift in medical weight loss, not merely by suppressing appetite but by engaging complex neuroendocrine and metabolic pathways that facilitate sustainable fat reduction. The convergence of personalized medicine, behavioral health integration, and emerging microbiome science positions Ozempic as a cornerstone of advanced obesity management strategies. For clinicians and patients alike, embracing these multidimensional insights fosters a more effective and enduring weight loss journey.
To deepen your expertise or initiate a tailored Ozempic-supported program, explore our clinician’s guide and connect with specialists who can help translate these advanced concepts into practical, safe, and impactful care. Your insights and experiences are invaluable—consider sharing them to enrich our evolving community focused on transformative health.


I found this post incredibly insightful, especially regarding how Ozempic not only aids in appetite regulation but also impacts neuroendocrine pathways that influence food reward and emotional eating. As someone who has struggled with emotional overeating, understanding these mechanisms gives me hope that a combination of medication and behavioral support can truly offer a sustainable solution. I’m curious—have any of you experienced a different response based on your gut microbiota composition or genetic factors? Thoughts on how to optimize treatment with these considerations in mind? Also, the potential of personalized dosing and microbiome modulation seems promising for increasing efficacy and reducing side effects. It makes me wonder, what are some practical steps patients can take to support their microbiome during such treatments? Would love to hear more personal experiences or insights from others navigating this journey.
This post really highlights how promising Ozempic is as part of a comprehensive weight management plan. I’ve seen firsthand in my practice how integrating medication with lifestyle changes—like personalized nutrition and behavioral therapy—can make a huge difference in long-term success. It’s fascinating to consider how neuroendocrine pathways influence not just hunger but emotional eating as well. That said, I’m curious about how patients can best support their microbiome during treatment. Are there specific prebiotic or probiotic strategies that can enhance Ozempic’s effectiveness? I’ve read some studies suggesting gut health plays a crucial role in metabolic responses, so maintaining a healthy microbiota might be an underrated component of treatment. Also, considering individual variability, do others have insights on how genetic testing or microbiome profiling has influenced your treatment plans or outcomes? It seems that as personalized medicine advances, we’ll be able to tailor therapies even more effectively to each unique patient.