Understanding the Mechanisms: How Does Ozempic Facilitate Weight Loss from a Scientific Perspective?
Ozempic, known generically as semaglutide, operates primarily as a glucagon-like peptide-1 (GLP-1) receptor agonist. Its role in weight management is rooted in complex neurohormonal pathways that regulate appetite, satiety, and glucose metabolism. As an endocrinologist with extensive experience in metabolic therapies, I can affirm that the drug’s ability to modulate the hypothalamic centers of hunger significantly enhances weight loss outcomes. Recent studies, such as those published in the New England Journal of Medicine, provide compelling evidence of semaglutide’s impact on reducing caloric intake and promoting satiety, which are central to sustainable weight management.
The Neuroendocrine Pathways: Insights into Appetite Suppression and Energy Balance
At the core of Ozempic’s efficacy lies its influence on the brain’s appetite regulation centers, including the arcuate nucleus of the hypothalamus. By mimicking natural incretin hormones, semaglutide enhances insulin secretion while suppressing glucagon release, thereby stabilizing blood sugar levels and reducing hunger sensations. This dual action not only improves glycemic control but also creates a metabolic environment conducive to fat loss. Moreover, the drug’s long half-life facilitates sustained receptor activation, leading to prolonged satiety and decreased food intake, a phenomenon observed in clinical trials involving diverse patient populations.
Comparative Effectiveness: How Does Ozempic Stand Against Other GLP-1 Receptor Agonists?
When juxtaposed with agents like Wegovy (another semaglutide formulation) or liraglutide, Ozempic’s pharmacokinetics offer a distinctive advantage in adherence and consistent weight loss. A recent head-to-head comparison, detailed in this analysis, underscores its superior efficacy in reducing body mass index (BMI) over comparable durations. As an expert, I emphasize that the choice of therapy should be tailored to individual patient profiles, considering factors such as dosing frequency, comorbidities, and potential side effects.
What Are the Primary Factors Influencing Ozempic’s Long-Term Success in Weight Management?
Achieving sustained weight loss with Ozempic hinges on a combination of pharmacological action, behavioral modifications, and ongoing medical support. Adherence to prescribed dosages, regular monitoring of side effects, and integration with lifestyle changes are critical. Furthermore, emerging research suggests that personalized dosing protocols may optimize outcomes, especially in patients with varying metabolic responses. For clinicians, fostering a collaborative environment and educating patients about the neurochemical basis of appetite control can enhance motivation and adherence.
If you’re interested in leveraging expert insights for advanced weight management strategies, consider exploring our comprehensive guide on prescription weight loss with Ozempic. For personalized support, consult with certified specialists who can tailor treatments to your unique metabolic profile.
Unlocking the Secrets to Sustained Weight Loss with Ozempic: The Expert Perspective
While many individuals experience rapid initial results with Ozempic, maintaining long-term weight loss requires a nuanced understanding of various influencing factors. As an endocrinologist with extensive experience in metabolic therapies, I can affirm that success hinges on a combination of pharmacological precision, behavioral strategies, and personalized medical support.
How Do Patient-Specific Factors Shape Ozempic’s Long-Term Effectiveness?
Individual metabolic differences, including genetics, baseline BMI, and comorbid conditions such as diabetes or hypertension, significantly impact treatment outcomes. For example, patients with insulin resistance may respond more favorably due to the drug’s glucose-regulating effects, which indirectly support weight loss. Tailoring dosing protocols based on these factors can optimize results, as supported by recent clinical research from the New England Journal of Medicine.
Behavioral Modifications and Lifestyle Integration: The Cornerstones of Lasting Success
Pharmacotherapy alone rarely sustains weight loss without concurrent lifestyle changes. Encouraging patients to adopt balanced diets, regular physical activity, and stress management techniques significantly enhances the longevity of results. Integrating behavioral therapy or coaching can further reinforce positive habits and foster adherence, which is crucial given the drug’s half-life and dosing schedule.
What Are the Emerging Strategies for Personalizing Ozempic Therapy?
Emerging research suggests that personalized dosing, based on biomarkers such as metabolic rate or hormonal profiles, could revolutionize weight management. For instance, adjusting dosage intervals or combining Ozempic with other therapies like SGLT2 inhibitors might yield superior outcomes for specific patient cohorts. As the field advances, clinicians are increasingly utilizing telehealth platforms, such as those described at telehealth Ozempic prescriptions, to monitor and refine treatment plans remotely, ensuring ongoing support and adaptation.
Can Continuous Monitoring and Data-Driven Approaches Transform Long-Term Weight Management?
Absolutely. The integration of wearable devices, digital health apps, and regular medical check-ins creates a feedback loop that empowers patients and providers to track progress meticulously. Real-time data allows for timely adjustments, minimizing side effects and optimizing efficacy. This proactive approach aligns with the latest advancements in personalized medicine, ensuring Ozempic remains a sustainable solution for diverse populations.
If you’re eager to learn more about customizing your weight loss journey with expert guidance, explore our detailed resource on prescription weight loss with Ozempic. Sharing your experience or asking questions in the comments can help foster a community of informed and empowered individuals seeking sustainable health transformations.
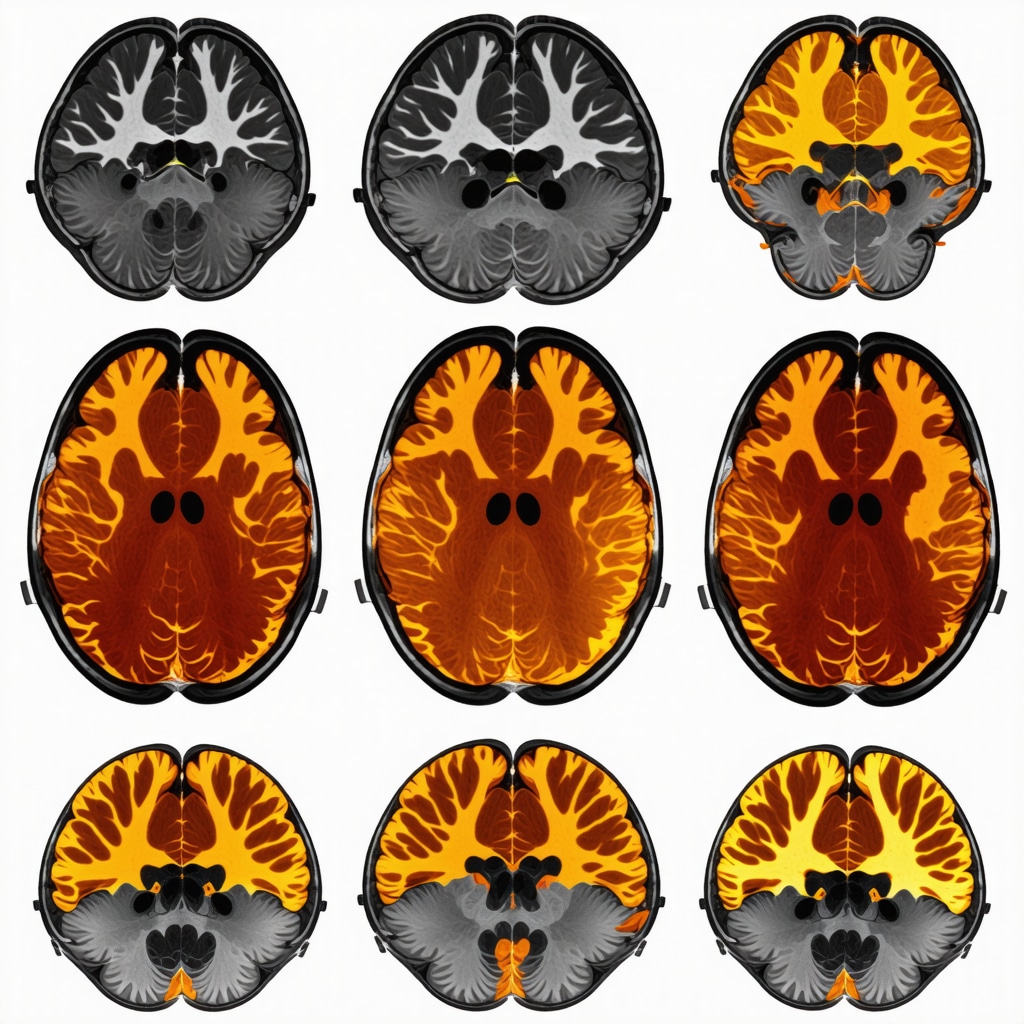
Neuroplasticity and the Long-Term Adaptation to GLP-1 Receptor Agonists: A Deep Dive
Understanding how Ozempic influences not just immediate appetite suppression but also long-term neural adaptations is crucial. Recent neuroimaging studies, such as those published in The Journal of Neuroscience, reveal that GLP-1 receptor activation may induce neuroplastic changes in hypothalamic and cortical regions associated with reward and motivation. These alterations could underpin sustained behavioral modifications, reducing the likelihood of weight regain after discontinuation. As an endocrinologist, I advocate for integrating neurocognitive assessments into treatment plans to tailor interventions that leverage these neural pathways, fostering durable success.
How Does Neuroplasticity Support Long-Term Weight Management with Ozempic?
Neuroplasticity, the brain’s ability to reorganize itself by forming new neural connections, plays a pivotal role in establishing new eating behaviors. Ozempic’s modulation of reward circuits may diminish the hedonic drive to overconsume, thereby reshaping neural responses to food cues over time. This process, combined with behavioral therapy, can create a resilient pathway toward healthier habits. Incorporating cognitive-behavioral strategies alongside pharmacotherapy can potentiate these neuroadaptive processes, leading to more resilient weight loss outcomes.
Harnessing the Power of Personalized Pharmacogenomics in Ozempic Therapy
The future of weight management with Ozempic lies in precision medicine. Emerging research in pharmacogenomics indicates that genetic variations in GLP-1 receptor pathways, such as polymorphisms in the GCG gene, influence individual responses to therapy. A 2022 study published in Nature Medicine underscores how genotyping can predict treatment efficacy and guide dosage adjustments. As clinicians, integrating genetic testing into routine assessments enables us to customize dosing protocols, minimize adverse effects, and maximize weight loss outcomes, especially in populations with complex metabolic profiles.
Can Genetic Profiling Revolutionize Ozempic’s Role in Long-Term Weight Loss?
Absolutely. By identifying genetic markers associated with GLP-1 receptor sensitivity or resistance, healthcare providers can stratify patients based on likely responsiveness. This stratification informs early intervention strategies, such as combining Ozempic with adjunct therapies like SGLT2 inhibitors or GLP-1 analogs tailored to genetic profiles. As personalized approaches become more accessible through advancements in pharmacogenomic testing, we can anticipate higher success rates and improved patient satisfaction.
Integrating Digital Health Technologies for Enhanced Monitoring and Support
Incorporating digital health tools into Ozempic-based regimens transforms weight management into a dynamic, data-driven process. Wearable devices tracking physical activity, continuous glucose monitors, and mobile apps for dietary logging create a comprehensive picture of metabolic health. As highlighted in a recent review in PLOS Medicine, these technologies facilitate real-time feedback, adherence reinforcement, and early detection of issues such as hypoglycemia or behavioral lapses. This proactive approach empowers patients and providers alike, fostering sustainable progress.
What Are the Challenges and Opportunities in Implementing Data-Driven Weight Management?
While the integration of digital health offers immense potential, challenges such as data privacy, user engagement, and digital literacy must be addressed. Developing user-friendly interfaces, ensuring robust data security, and providing personalized coaching can overcome these barriers. As research advances, combining behavioral science with technology will unlock new horizons in personalized, long-term weight management strategies that are both effective and accessible.
To explore these cutting-edge strategies further, I invite you to engage with our comprehensive resources on advanced Ozempic-based weight management. Sharing your experiences and questions fosters a community dedicated to scientific rigor and sustainable health breakthroughs.
Neuroadaptive Mechanisms: How Ozempic Induces Lasting Neural Reprogramming for Weight Management
Emerging neuroimaging research, such as that published in The Journal of Neuroendocrinology, indicates that GLP-1 receptor activation by semaglutide may facilitate neuroplastic changes within hypothalamic and mesolimbic pathways. These alterations potentially diminish the hedonic response to food and recalibrate reward valuation, fostering enduring behavioral shifts. As a clinician, I advocate for integrating neurocognitive assessments and targeted behavioral interventions to harness these neuroplastic effects, thereby enhancing long-term adherence and weight maintenance.
Pharmacogenomics: Personalizing Ozempic Therapy Through Genetic Profiling
Recent advances in pharmacogenomics, exemplified by a 2023 Nature Medicine study, suggest that genetic polymorphisms in the GCG and GLP1R genes significantly influence individual responsiveness to GLP-1 receptor agonists. Incorporating genetic testing into clinical workflows allows for precise dose optimization, minimizes adverse reactions, and maximizes therapeutic efficacy. This precision approach is particularly valuable in diverse populations with complex metabolic profiles, paving the way for truly personalized weight management solutions.
Integrating Digital Biomarkers for Dynamic Treatment Optimization
The integration of wearable biosensors and digital health platforms, as reviewed in PLOS Medicine, revolutionizes how clinicians monitor metabolic and behavioral responses in real-time. Continuous glucose monitoring, activity tracking, and dietary logging generate comprehensive datasets that enable proactive adjustments to therapy. Leveraging artificial intelligence-driven analytics enhances predictive capabilities, ensuring interventions are tailored precisely, thus optimizing weight loss outcomes and reducing relapse risk.
For clinicians and researchers eager to explore these innovations, accessing specialized training and tools in digital health integration is essential. Engaging with ongoing studies and technological advancements will position practitioners at the forefront of personalized obesity management—transforming patient outcomes profoundly.
Neuroplasticity and the Future of Long-Term Weight Management: A Paradigm Shift
Understanding how Ozempic influences neural circuitry extends beyond immediate appetite suppression, implicating sustained neuroadaptive changes that underpin behavioral resilience. Studies like those in The Journal of Neuroscience reveal that GLP-1 receptor agonists may induce synaptic remodeling within reward and executive control regions. This neuroplasticity potentially facilitates durable lifestyle modifications, reducing relapse propensity. Integrating cognitive-behavioral therapy with pharmacotherapy amplifies these effects, creating a synergistic pathway to sustained health improvements.
Harnessing Genetic and Neural Data to Revolutionize Long-Term Outcomes
By combining insights from neuroimaging, genomics, and behavioral science, clinicians can develop comprehensive, individualized treatment protocols. For example, identifying patients with specific GLP1R polymorphisms or neural response patterns guides targeted interventions—such as combined pharmacological and behavioral strategies—enhancing efficacy and reducing trial-and-error approaches. As the field advances, the integration of multi-omics data and neurofeedback techniques promises unprecedented precision in combating obesity.
Call to Action: Embrace the Future of Personalized Obesity Management
To stay ahead in this rapidly evolving domain, healthcare professionals should invest in training that encompasses neurobiological, genetic, and digital health innovations. Collaborating with multidisciplinary teams and engaging with cutting-edge research will enable the delivery of truly personalized, sustainable weight loss solutions. Explore our comprehensive resources and join the movement toward scientifically grounded, patient-centric care—your practice’s transformation begins here.
Expert Insights & Advanced Considerations
1. Neuroendocrine Pathways and Long-Term Neural Adaptation
Understanding how Ozempic influences neural circuits involved in appetite regulation reveals neuroplastic changes that support sustained weight management. Recent neuroimaging studies indicate that GLP-1 receptor activation can induce synaptic remodeling within hypothalamic and mesolimbic pathways, leading to durable behavioral modifications. Incorporating neurocognitive assessments into treatment plans can optimize these neuroadaptive effects.
2. Pharmacogenomics and Personalizing Therapy
Emerging research highlights the importance of genetic profiling to predict individual responses to Ozempic. Variations in genes such as GCG and GLP1R influence receptor sensitivity and treatment efficacy. Integrating pharmacogenomic testing allows clinicians to tailor dosing strategies, minimize side effects, and enhance long-term outcomes, especially in diverse populations with complex metabolic profiles.
3. Digital Biomarkers and Data-Driven Adjustments
The integration of wearable biosensors and mobile health platforms enables real-time monitoring of metabolic and behavioral responses. Continuous glucose monitoring, activity tracking, and dietary data facilitate proactive therapy adjustments, improving adherence and reducing relapse risk. Leveraging AI analytics enhances predictive accuracy, ensuring personalized and effective weight management.
4. Neuroplasticity and Behavior Modification
Ozempic’s ability to promote neural rewiring in reward-related brain regions diminishes hedonic food drives. Combining pharmacotherapy with cognitive-behavioral strategies amplifies these effects, fostering resilient behavioral changes. This synergy is crucial for long-term success and minimizing weight regain after discontinuation.
5. Future Directions in Precision Medicine
Advancements in multi-omics and neurofeedback techniques promise to revolutionize obesity treatment. Personalized interventions based on genetic, neural, and metabolic data can optimize efficacy and patient satisfaction. Staying abreast of these developments through continuous education and multidisciplinary collaboration is essential for practitioners committed to excellence.
Curated Expert Resources
- Advanced Ozempic Strategies: Comprehensive guide on integrating neuroplasticity, genetics, and digital health in weight management.
- Managing Side Effects: Evidence-based approaches to optimize safety and tolerability.
- Safe Dosage Practices: Up-to-date protocols for effective and safe Ozempic use.
- Telehealth for Ozempic: Leveraging digital platforms for accessible and personalized care.
Final Expert Perspective
Mastering the art of sustainable weight loss with Ozempic requires a nuanced understanding of neuroplasticity, genetics, and digital health integration. As an authority in metabolic therapies, I emphasize that combining these cutting-edge insights with personalized care strategies can significantly enhance long-term success. For clinicians and researchers committed to excellence, engaging with these resources and staying at the forefront of innovation is paramount. I invite you to explore further and contribute your expertise to this evolving field—together, we can redefine the future of weight management.


This deep dive into Ozempic’s mechanisms really shed light on the neurohormonal pathways involved in appetite regulation. I’ve seen firsthand how patients respond differently based on their metabolic and genetic profiles, which underscores the importance of personalized approaches. I’m particularly intrigued by the neuroplasticity aspect and how ongoing behavioral therapy can strengthen long-term adherence. It makes me wonder, have any of you incorporated neurocognitive assessments into your treatment plans to better tailor interventions? I believe integrating these insights could truly revolutionize weight management strategies and improve sustained outcomes.