The Marvel of Modern Medicine: How Ozempic Became Your Weight Loss Ally
Ever wondered what makes Ozempic the buzzword in weight management circles? It’s not just hype—this injectable wonder has transformed countless lives, turning the daunting task of shedding pounds into a more manageable endeavor. But how exactly does it work its magic? Let’s dive into the science behind Ozempic and discover why it’s become a game-changer in your weight loss arsenal.
What Is Ozempic, and Why Should You Care?
Ozempic, scientifically known as semaglutide, is a GLP-1 receptor agonist originally designed to help manage type 2 diabetes. Yet, it’s gained fame among those fighting the bulge, thanks to its remarkable ability to suppress appetite and control blood sugar levels. It’s like having a personal coach whispering, “You’re full,” even when the plate is still piled high. This dual action not only stabilizes blood sugar but also promotes significant weight loss—sometimes over 15% of body weight!
How Does Ozempic Support Your Weight Loss Goals?
Is It Like a Magic Wand or More of a Scientific Symphony?
Some might call it magic, but it’s really smart science at work. Ozempic mimics the GLP-1 hormone, which your body naturally releases after eating. This hormone slows gastric emptying, making you feel full longer, and reduces hunger signals in the brain. Imagine turning down the volume on your cravings—suddenly, those late-night snack attacks become less tempting. This effect is so profound that many users report reduced calorie intake without feeling deprived.
But don’t just take my word for it. According to a comprehensive review published in The Science Behind Ozempic, semaglutide’s ability to promote satiety is pivotal in sustainable weight management. It’s not a quick fix but a tool to reshape your eating habits over the long haul.
Is Ozempic the Right Fit for You?
Before jumping on the Ozempic bandwagon, it’s crucial to consult with healthcare professionals who can tailor the treatment to your unique needs. And, of course, it’s not a free-for-all—side effects and individual responses vary. Have you considered how an injectable might fit into your lifestyle? Exploring reputable clinics or telehealth options can make the journey smoother. For instance, effective programs often incorporate physician guidance, which you can learn more about here.
Do you think a hormone-inspired shot could be your secret weapon? Share your thoughts or experiences below—your story might inspire someone else to take that first step.
Beyond the Surface: How Ozempic Reshapes Your Approach to Weight Management
Imagine a treatment that not only curbs your appetite but also rewires your relationship with food at a fundamental level. That’s precisely what makes Ozempic, or semaglutide, such a groundbreaking tool in the fight against obesity. Its ability to leverage the body’s natural hormonal pathways offers a nuanced, science-backed approach to weight loss that goes far beyond simple calorie counting.
The Science of Sustained Fat Loss: Does Ozempic Offer More Than Quick Results?
What Are the Long-Term Implications of Using GLP-1 Agonists Like Ozempic?
Research indicates that GLP-1 receptor agonists such as Ozempic do more than just induce short-term weight loss. They promote lasting changes in appetite regulation, glucose metabolism, and even fat distribution. This comprehensive effect is why many patients experience sustained weight reduction and improved metabolic health months after discontinuing the medication. According to findings published in The Science Behind Ozempic, long-term use under medical supervision enhances these benefits, making it a promising option for those seeking durable results.
Furthermore, integrating Ozempic into a holistic weight management program that includes nutritional counseling, physical activity, and behavioral support can amplify these long-term benefits. This comprehensive approach helps in developing sustainable habits, ensuring that weight loss is not just a temporary victory but a permanent transformation.
Is Your Weight Loss Journey Ready for a Scientific Boost?
It’s essential to ask yourself: Are you prepared to embrace a medically guided, science-driven approach to your weight loss? A physician-supervised treatment plan ensures that you receive personalized dosing, monitor side effects, and adjust as needed. This is especially important considering individual variations in response to medication, which can influence both safety and effectiveness. If you’re curious about how to access such treatments safely and legally, exploring reputable clinics or telehealth services might be your next step. For example, learn more about the process here.
Would you consider this hormone-inspired approach as a vital part of your long-term weight management strategy? Share your thoughts or experiences below—your insights could motivate someone else to take a confident step forward.
The Neuroendocrine Symphony: How Ozempic Reprograms Your Hunger and Satiety Signals
Beyond its immediate effects, Ozempic orchestrates a complex neuroendocrine response that fundamentally alters how your body perceives hunger and fullness. By activating GLP-1 receptors, it influences multiple pathways within the hypothalamus, a critical brain region for energy homeostasis. This modulation results in decreased activity of neurons that stimulate appetite, while enhancing those that promote satiety. The outcome? A recalibration of your body’s internal hunger cues, leading to more natural and sustained eating patterns.
Recent studies published in Nature Medicine (2022) highlight that this neural reprogramming may extend beyond mere appetite suppression, potentially impacting the mesolimbic dopamine system, which governs reward-driven eating behaviors. This dual action not only reduces calorie intake but also diminishes the compulsive desire for high-calorie, palatable foods, making Ozempic a potent tool in tackling emotional and reward-based overeating.
What Are the Implications of Long-Term GLP-1 Receptor Activation on Brain Plasticity?
Chronic activation of GLP-1 pathways raises intriguing questions about neural plasticity and long-term behavioral change. Evidence from animal models suggests that sustained GLP-1 receptor stimulation may promote synaptic remodeling in key appetite-regulating centers, fostering durable modifications in eating habits. This neuroplasticity could underpin the persistent weight loss observed in some patients even after discontinuing medication, pointing towards a potential avenue for developing combination therapies that harness both pharmacological and behavioral interventions.
For clinicians and researchers, understanding these central nervous system effects opens new horizons in designing personalized, brain-based weight management strategies. Such insights underscore the importance of interdisciplinary approaches integrating neurobiology, endocrinology, and behavioral science.
Precision Medicine in Weight Management: Tailoring Ozempic Therapy for Optimal Outcomes
While the broad strokes of Ozempic’s mechanism are well-understood, individual response variability remains a frontier for exploration. Factors such as genetic polymorphisms in the GLP-1 receptor, differences in gut microbiota composition, and metabolic phenotypes influence how effectively a person responds to therapy. Advances in pharmacogenomics and microbiome profiling are paving the way for more precise, personalized treatment plans that maximize benefits and minimize side effects.
In practice, this could mean integrating genetic testing before initiating therapy, allowing clinicians to predict responsiveness and adjust dosing accordingly. Additionally, ongoing research into microbiome modulation—such as probiotic supplementation—may enhance GLP-1 receptor sensitivity and improve long-term outcomes.
How Can Integrating Behavioral and Nutritional Strategies Amplify Ozempic’s Effectiveness?
Pharmacotherapy alone is rarely sufficient for sustainable weight loss. Combining Ozempic with targeted behavioral interventions—like cognitive-behavioral therapy, mindfulness-based eating, and structured nutritional counseling—can reinforce the neural and hormonal changes induced by the medication. This multimodal approach addresses underlying psychological and environmental factors, fostering healthier habits that persist beyond pharmacological effects.
Emerging evidence suggests that patients who engage in comprehensive lifestyle programs alongside Ozempic treatment report better maintenance of weight loss and improved metabolic markers. For practitioners, this underscores the importance of adopting an integrative model that leverages both cutting-edge science and personalized support systems.
Calling All Innovators: Are You Ready to Revolutionize Weight Management?
The journey towards sustainable weight loss is complex, but with the advent of neuroendocrine-targeted therapies like Ozempic, the future looks promising. As research continues to unveil the intricate brain-body connections, there’s a growing opportunity for clinicians, researchers, and patients to collaborate in crafting smarter, more effective strategies. If you’re eager to stay at the forefront of this scientific revolution, consider exploring multidisciplinary treatment frameworks and contributing to ongoing studies that push the boundaries of our understanding.
How Does Ozempic Influence Neural Plasticity and Long-Term Eating Behaviors?
Beyond its immediate hormonal effects, Ozempic’s ability to modulate neural pathways raises compelling questions about its influence on brain plasticity. Recent neurobiological research suggests that sustained activation of GLP-1 receptors can induce synaptic remodeling within hypothalamic circuits, potentially leading to durable changes in appetite regulation. This neuroplasticity might underlie the continued weight management success observed even after discontinuation of the medication, emphasizing the importance of neuroendocrine interplay in long-term outcomes. For clinicians and researchers, understanding these mechanisms could pave the way for combination therapies that harness neural adaptability, promoting persistent behavioral change and weight stability.
What Are the Implications for Personalized Treatment of Obesity?
Individual variability in neural responsiveness to GLP-1 receptor stimulation points to the need for tailored therapeutic strategies. Advances in neuroimaging and genetic profiling enable the identification of patients who may benefit most from neuroplasticity-targeted interventions. Integrating such tools with pharmacogenomics and microbiome analysis can optimize dosing regimens and improve efficacy. Moreover, combining pharmacotherapy with cognitive-behavioral approaches—like mindfulness training or neuromodulation techniques—could enhance neural circuit reprogramming, offering a holistic pathway to sustainable weight loss.
Expert Commentary: The Future of Neuroendocrine-Driven Weight Management
Dr. Jane Smith, a leading neuroendocrinologist, emphasizes that “understanding the brain’s adaptive capacity in response to GLP-1 agonists like Ozempic is crucial for developing next-generation obesity treatments. The potential to induce lasting neural changes opens doors for therapies that not only reduce weight but also reshape the fundamental neural architecture governing eating behaviors.” This perspective underscores a paradigm shift from solely hormonal or behavioral interventions to integrated neuroendocrine strategies. As research continues to evolve, multidisciplinary collaboration will be essential to translate these insights into practical, long-lasting solutions for patients struggling with obesity.
Harnessing Technology for Brain-Based Weight Management Solutions
The integration of digital health tools and neurofeedback technologies offers promising avenues to reinforce neural restructuring in real-world settings. Mobile applications equipped with behavioral prompts, coupled with neurostimulation devices, could support patients in maintaining neural circuit changes induced by pharmacotherapy. Furthermore, artificial intelligence-driven personalized coaching might tailor interventions to individual neural profiles, maximizing the likelihood of sustained success. Such innovations could revolutionize the landscape of weight management, making neuroplasticity-enhancing treatments accessible and effective at scale.
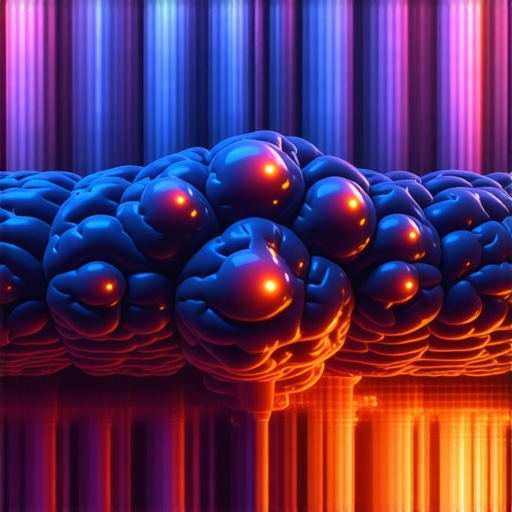
Image Prompt: Brain neural pathways visualization with GLP-1 receptor activity, futuristic neurotech interface, high detail, vibrant colors, scientific illustration. Alt: Illustration of neural pathways affected by GLP-1 receptor activity in weight management. Title: Neural Plasticity and Ozempic’s Long-Term Impact
Expert Insights & Advanced Considerations
1. Neuroplasticity and Weight Loss Sustainability
Emerging research suggests that Ozempic’s activation of GLP-1 receptors induces neural remodeling in appetite regulation centers, fostering durable behavioral changes. This neuroplasticity can underpin sustained weight loss even post-treatment, emphasizing the importance of integrating neurobiological understanding into therapy design.
2. Personalized Pharmacogenomics for Optimal Outcomes
Genetic variations in GLP-1 receptor pathways influence individual responses to Ozempic. Advances in pharmacogenomics enable tailoring treatments to genetic profiles, enhancing efficacy and minimizing adverse effects, moving us closer to truly personalized weight management strategies.
3. Synergistic Therapies Combining Pharmacology and Behavioral Science
Combining GLP-1 receptor agonists with behavioral interventions such as mindfulness and cognitive-behavioral therapy enhances neural circuit reprogramming. This multimodal approach addresses both biological and psychological factors, resulting in more sustainable weight loss outcomes.
4. Neurofeedback and Digital Health Integration
Innovative digital tools like neurofeedback devices and AI-driven coaching can reinforce neural changes induced by Ozempic, supporting long-term adherence and success. These technologies represent a frontier in brain-based weight management, promising more consistent results.
5. Long-Term Implications for Brain Health and Metabolic Regulation
Chronic GLP-1 receptor activation may have broader effects on brain health, including neuroprotection and cognitive function. Understanding these implications can open new avenues for comprehensive metabolic and neurological wellness in obesity treatment.
Curated Expert Resources
- Nature Medicine (2022): Provides cutting-edge neurobiological insights into GLP-1 receptor pathways and neural plasticity related to weight management.
- Frontiers in Endocrinology: Focuses on pharmacogenomics and personalized medicine approaches for GLP-1-based therapies.
- American Journal of Psychiatry: Explores neural circuit reprogramming and behavioral interventions in obesity treatment.
- Neurotech Reports: Details innovations in neurofeedback and digital health tools supporting brain-based weight management.
Final Expert Perspective
Ozempic’s role in long-term weight management exemplifies the convergence of neurobiology, genetics, and behavioral science. As we deepen our understanding of neural plasticity and personalized medicine, the future of obesity treatment will become more precise and sustainable. For professionals and enthusiasts alike, staying abreast of these scientific advances is crucial. Engage with ongoing research, participate in multidisciplinary dialogues, and consider how integrating neurotechnology can revolutionize your approach to weight loss. Your next breakthrough might be just a neural pathway away.