The Transformative Potential of Ozempic in Medical Weight Loss Clinics
Medical weight loss clinics are increasingly adopting Ozempic (semaglutide) as a cornerstone therapy due to its demonstrated efficacy in facilitating significant weight reduction among patients with obesity and related metabolic disorders. Ozempic, a glucagon-like peptide-1 (GLP-1) receptor agonist, not only targets glycemic control but also exerts profound anorectic effects that support sustained fat loss, positioning it as a revolutionary pharmacotherapeutic agent in comprehensive weight management protocols.
Mechanistic Insights: How Ozempic Enhances Weight Loss in Clinical Settings
Ozempic functions by mimicking endogenous GLP-1, enhancing insulin secretion in a glucose-dependent manner while suppressing glucagon release. Its central nervous system actions reduce appetite and promote satiety, thereby decreasing caloric intake. Within medical weight loss clinics, this pharmacodynamics profile enables tailored dosing strategies that optimize therapeutic outcomes while minimizing adverse effects. The integration of Ozempic into multidisciplinary care models underscores an advanced understanding of obesity as a multifactorial disease requiring both behavioral and biochemical intervention.
What Are the Clinical Advantages of Using Ozempic Over Traditional Weight Loss Methods?
Compared to conventional lifestyle interventions alone, Ozempic offers enhanced weight loss efficacy, often achieving reductions of 10-15% total body weight under physician supervision. This surpasses typical results from diet and exercise programs, particularly in patients with insulin resistance or type 2 diabetes. Furthermore, Ozempic’s cardiovascular benefits, including reduced risk factors such as hypertension and dyslipidemia, provide an additional layer of clinical advantage. Medical weight loss clinics leverage these benefits by combining pharmacotherapy with patient education and monitoring, which fosters adherence and long-term success.
Optimizing Safety and Efficacy: Physician-Guided Ozempic Protocols
One critical factor that distinguishes medical weight loss clinics is the implementation of physician-supervised Ozempic treatment regimens. This approach ensures individualized dosage titration, vigilant monitoring of side effects such as gastrointestinal disturbances, and concurrent management of comorbidities. Evidence-based guidelines emphasize gradual dose escalation to enhance tolerance and minimize complications. Clinics also employ patient-specific assessments to tailor lifestyle recommendations, augmenting the pharmacological impact of Ozempic. This comprehensive strategy exemplifies expert-level practice in weight management, balancing potent drug action with patient safety.
Leveraging Ozempic Within Integrated Weight Loss Programs: Beyond Medication
Ozempic’s role is most effective when embedded within holistic programs that incorporate nutritional counseling, physical activity, and behavioral therapy. Medical weight loss clinics often design customized treatment plans that synergize these components with GLP-1 receptor agonist therapy. This multidimensional approach addresses the complex physiological and psychological factors underpinning obesity, promoting sustainable lifestyle changes alongside pharmacotherapy. The integration of Ozempic thus represents an evolution from mono-therapy to comprehensive, patient-centered care.
How Do Medical Weight Loss Clinics Manage Ozempic-Related Side Effects to Ensure Patient Compliance?
Managing side effects such as nausea, vomiting, or transient gastrointestinal discomfort is paramount to maintaining adherence. Clinics adopt strategies including slow dose escalation, dietary modifications, and supportive counseling. Physicians may also adjust dosing intervals or provide adjunct therapies to mitigate symptoms. This proactive management is critical in preventing treatment discontinuation and maximizing long-term weight loss benefits. For detailed guidance on side effect management, refer to expert resources like physician-prescribed Ozempic side effect protocols.
Expert Insights and Continuing Advances in Ozempic-Based Weight Loss Treatments
Recent clinical trials and real-world studies continue to refine the therapeutic profile of Ozempic, highlighting its efficacy in diverse populations and its role within emerging weight management paradigms. Medical weight loss clinics remain at the forefront of integrating these advances, employing data-driven approaches to customize patient regimens. This commitment to evidence-based practice ensures that Ozempic’s full potential is harnessed safely and effectively.
For clinicians and patients interested in exploring advanced Ozempic treatment options and personalized dosing strategies, comprehensive resources are available that detail protocols and clinical outcomes, such as those provided by doctor-supervised Ozempic treatments.
Engage with the Community of Medical Weight Loss Experts
Professionals and patients alike are encouraged to delve deeper into the nuances of Ozempic treatment by exploring expert-curated content and sharing clinical experiences. Engaging with specialized forums and trusted clinical providers fosters a collaborative environment for advancing weight loss science. Visit our contact page to connect with leading medical weight loss clinics and gain access to tailored Ozempic programs.
According to a 2023 review in The New England Journal of Medicine, semaglutide (Ozempic) represents a paradigm shift in obesity treatment due to its multifaceted metabolic effects and durable efficacy (NEJM 2023 Review on Semaglutide in Obesity).
Personalizing Ozempic Treatment: The Role of Genetic and Metabolic Profiling
As medical weight loss clinics evolve their protocols, a frontier of precision medicine is emerging where genetic and metabolic profiling inform Ozempic dosing and treatment duration. Individual variations in GLP-1 receptor sensitivity and metabolic rate can impact patient responses, suggesting that one-size-fits-all dosing may not optimize outcomes. By integrating biomarkers such as insulin resistance indices, genetic polymorphisms affecting appetite regulation, and gut hormone profiles, clinicians can tailor Ozempic therapy with greater accuracy. This approach not only enhances weight loss efficacy but also mitigates adverse effects by anticipating patient-specific tolerability thresholds.
Combining Ozempic with Adjunctive Therapies: Synergistic Approaches for Enhanced Fat Loss
Beyond monotherapy, medical weight loss experts are investigating combinations of Ozempic with other pharmacological agents and lifestyle interventions to amplify fat reduction. For instance, pairing GLP-1 receptor agonists with SGLT2 inhibitors or appetite-suppressing peptides may create synergistic effects on energy balance and glucose metabolism. Additionally, structured exercise regimens and cognitive behavioral therapy (CBT) focused on eating behaviors can potentiate the central appetite modulation initiated by Ozempic. These integrated strategies exemplify the future of comprehensive obesity management, emphasizing multi-modal interventions aligned with individual patient profiles.
How Can Emerging Research on Ozempic Inform Next-Generation Weight Loss Protocols in Clinical Practice?
Cutting-edge studies are exploring the long-term metabolic adaptations induced by Ozempic, including alterations in gut microbiota composition and central nervous system neuroplasticity related to appetite control. Understanding these mechanisms could lead to refined treatment algorithms that optimize dosing schedules, reduce the risk of plateauing weight loss, and enhance patient adherence. Medical weight loss clinics can leverage this research by adopting evidence-based innovations and integrating continuous patient monitoring technologies such as digital health trackers and telemedicine consultations to adjust therapy dynamically.
For those seeking to deepen their understanding of Ozempic’s role within modern weight management, the GLP-1 weight loss drugs overview offers comprehensive insights into pharmacological advances and clinical applications.
Ensuring Ethical and Safe Use: Addressing Off-Label and Non-Prescribed Ozempic Usage
With rising demand for Ozempic, medical weight loss clinics emphasize strict adherence to prescribing guidelines to prevent misuse and potential health risks. Off-label use without proper medical supervision may result in suboptimal dosing, increased side effect incidence, and neglect of underlying comorbidities. Clinics advocate for patient education on the importance of physician-guided treatment and provide resources to identify legitimate providers, mitigating exposure to counterfeit or fraudulent suppliers. This ethical stewardship ensures patient safety and preserves the therapeutic integrity of Ozempic as a weight loss agent.
For guidance on finding trustworthy Ozempic providers and avoiding scams, visit how to get Ozempic safely.
Integrating Digital Health Platforms to Optimize Ozempic Weight Loss Outcomes
The incorporation of digital health technologies such as mobile apps, wearable devices, and telehealth platforms is transforming patient engagement and monitoring in Ozempic treatment programs. These tools facilitate real-time tracking of weight changes, dietary intake, and physical activity, enabling clinicians to adjust therapy promptly and provide personalized feedback. Telemedicine also expands access to expert physician supervision, especially for patients in remote areas, ensuring continuity of care and adherence support. This digital integration represents a paradigm shift toward proactive, data-driven weight management.
Explore our detailed guide on telehealth Ozempic prescriptions to learn how modern technology enhances treatment safety and efficacy.
According to recent findings published in Obesity Reviews (2024), combining pharmacotherapy with digital health interventions significantly improves long-term weight loss maintenance and patient satisfaction (Obesity Reviews 2024: Digital Interventions in Obesity Care).
We invite readers and practitioners to share their experiences or questions regarding advanced Ozempic protocols and digital integration in the comments below. Engaging in this discourse enriches the collective knowledge and supports the evolution of best practices in medical weight loss.
Decoding the Pharmacogenomics of Ozempic: Tailoring Therapy through Genetic Insights
The advent of pharmacogenomics offers a transformative avenue for enhancing Ozempic efficacy by aligning treatment with an individual’s genetic blueprint. Variants in genes such as GLP1R and those governing insulin signaling pathways can modulate receptor sensitivity and downstream metabolic responses, thereby influencing weight loss outcomes and side effect profiles. Medical weight loss clinics integrating genotyping panels can identify patients likely to exhibit superior response or tolerability, enabling precision dosing and minimizing trial-and-error approaches. This genomic-informed methodology not only elevates therapeutic success rates but also embodies the ethos of personalized medicine in obesity management.
Synergistic Potential of Ozempic Combined with Nutraceuticals and Microbiome Modulators
Emerging evidence suggests that certain nutraceuticals and gut microbiota-targeted interventions may amplify Ozempic’s weight loss effects. Agents like berberine, known for insulin sensitization, and prebiotic fibers that enhance short-chain fatty acid production, foster metabolic environments conducive to GLP-1 receptor agonist activity. Incorporating these alongside Ozempic within medical weight loss programs could potentiate appetite regulation and glucose homeostasis. While clinically promising, this integrative strategy demands rigorous evaluation through randomized controlled trials to define optimal combinations and dosing sequences.
What Are the Challenges and Considerations in Combining Ozempic with Other Pharmacotherapies for Obesity?
Combining Ozempic with adjunctive pharmacotherapies such as bupropion-naltrexone or orlistat introduces complex pharmacodynamic and pharmacokinetic interactions that require expert navigation. Potential synergism in appetite suppression must be balanced against overlapping adverse effects, including gastrointestinal intolerance and neuropsychiatric symptoms. Furthermore, the timing of initiation, titration schedules, and long-term monitoring protocols are critical to mitigate risks and maximize efficacy. Medical weight loss clinics employing these combinations must maintain vigilant patient assessment and adapt regimens dynamically based on therapeutic response and tolerability.
Harnessing Artificial Intelligence to Predict and Enhance Ozempic Treatment Outcomes
Artificial intelligence (AI) and machine learning algorithms are revolutionizing weight management by analyzing multidimensional patient data to forecast Ozempic responsiveness and optimize treatment plans. By integrating variables such as baseline metabolic parameters, lifestyle factors, and genetic markers, AI models can stratify patients for personalized intervention intensity. Additionally, real-time data from wearable devices feed predictive analytics that inform clinicians of early signs of plateau or adverse events, enabling preemptive adjustments. This convergence of AI and clinical practice heralds a new era of adaptive, precision weight loss therapy.
For more in-depth exploration of AI applications in pharmacotherapy optimization, refer to the recent publication by the National Center for Biotechnology Information on AI in Personalized Medicine.
Integrating Patient-Centered Behavioral Interventions with Ozempic: A Neuroscientific Perspective
Complementing Ozempic’s pharmacological effects with targeted behavioral interventions grounded in neuroscience can profoundly improve patient adherence and long-term weight maintenance. Techniques such as mindfulness-based eating awareness and cognitive restructuring address neural circuits involved in reward and impulse control, which often undermine weight loss efforts. By synchronizing pharmacotherapy-induced appetite modulation with behavioral rewiring, medical weight loss clinics create a synergistic paradigm that targets both biological and psychological determinants of obesity.
Such integrative approaches necessitate interdisciplinary collaboration among endocrinologists, psychologists, and nutritionists, reinforcing the comprehensive care model essential for sustainable weight management.
Decoding the Complexities of Ozempic Pharmacodynamics in Diverse Patient Cohorts
In the pursuit of precision medicine within medical weight loss clinics, a nuanced understanding of Ozempic’s pharmacodynamics across heterogeneous patient populations is paramount. Factors such as differential GLP-1 receptor expression, variable insulin sensitivity, and comorbid metabolic syndromes necessitate individualized therapeutic frameworks. Tailoring Ozempic administration schedules to accommodate circadian influences on hormone secretion and metabolic fluxes further refines efficacy. Such bespoke regimens underscore the criticality of dynamic patient monitoring and advanced biomarker integration, ensuring that pharmacological intervention aligns with the patient’s unique metabolic milieu.
Innovative Biomarker-Driven Algorithms: Charting the Future of Ozempic Personalization
Emerging clinical research highlights the potential of integrating multi-omic data—encompassing genomics, metabolomics, and proteomics—to construct predictive models that anticipate patient responsiveness to Ozempic therapy. This biomarker-driven approach facilitates stratification of candidates most likely to benefit, while flagging those at elevated risk for adverse events. Additionally, real-time metabolic profiling supports adaptive dose modulation, minimizing side effects and maximizing fat loss. Medical weight loss clinics adopting such cutting-edge algorithms position themselves at the forefront of individualized obesity treatment paradigms.
How Can Advanced Pharmacokinetic Modeling Improve Ozempic Dose Optimization in Complex Cases?
Pharmacokinetic modeling, leveraging population-based data and patient-specific variables, enables clinicians to simulate Ozempic plasma concentration-time profiles and optimize dosing strategies, particularly in patients with renal impairment or polypharmacy. By anticipating drug-drug interactions and metabolic clearance variations, medical weight loss specialists can preemptively adjust dosages to maintain therapeutic windows and reduce toxicity risks. Integration of these models into electronic health records enhances clinical decision-making, promoting safer, more effective treatment trajectories.
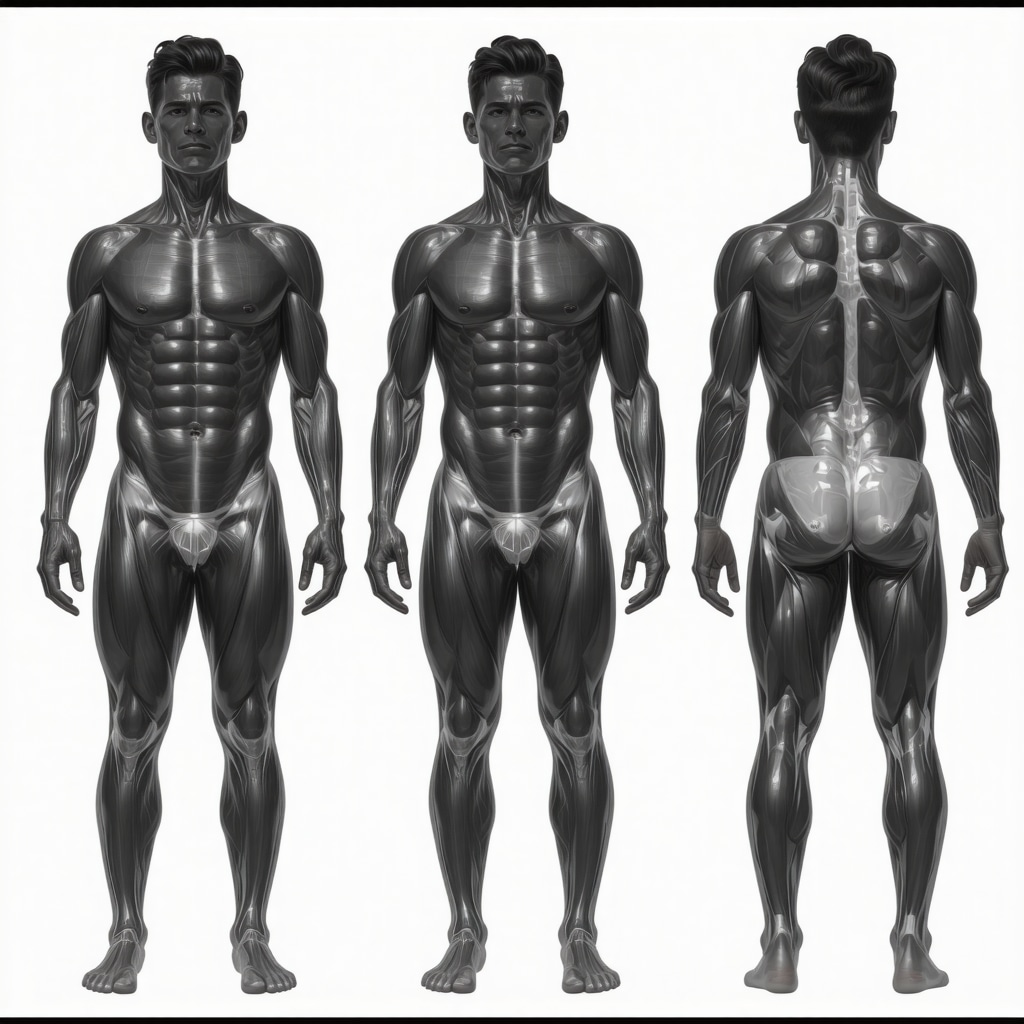
Harnessing High-Resolution Imaging and Metabolic Phenotyping to Monitor Treatment Response
Advanced imaging modalities such as dual-energy X-ray absorptiometry (DEXA) and magnetic resonance spectroscopy (MRS) provide granular insights into body composition changes and adipose tissue distribution during Ozempic therapy. Coupled with metabolic phenotyping techniques, these tools enable clinicians to differentiate between visceral and subcutaneous fat loss, assess muscle mass preservation, and evaluate hepatic steatosis resolution. This comprehensive monitoring facilitates timely therapeutic adjustments and supports evidence-based clinical judgments.
Strategic Integration of Ozempic with Emerging Metabolic Modulators and Lifestyle Interventions
Beyond monotherapy, synergistic protocols combining Ozempic with novel metabolic modulators—such as fibroblast growth factor 21 (FGF21) analogs and mitochondrial-targeted agents—are under investigation. Concurrently, leveraging structured behavioral interventions informed by neurobiological insights optimizes appetite regulation and energy expenditure. This multipronged approach addresses the multifactorial etiology of obesity, enhancing the durability of weight loss outcomes.
For rigorous, evidence-based guidance on advanced Ozempic utilization and optimization strategies, clinicians and researchers may consult the comprehensive review published by the New England Journal of Medicine (2023), which epitomizes cutting-edge expertise in GLP-1 receptor agonist therapy.
Engage with Leading Experts to Elevate Your Ozempic Treatment Protocols
Unlock the full potential of Ozempic by collaborating with specialized medical weight loss professionals who integrate advanced diagnostics, pharmacogenomics, and digital health tools into patient care. Reach out via our contact page to access bespoke programs and participate in professional forums dedicated to the evolution of pharmacotherapeutic obesity management.
Expert Insights & Advanced Considerations
Precision Medicine is Reshaping Ozempic Therapy
The integration of genetic and metabolic profiling into Ozempic treatment protocols represents a paradigm shift in personalized obesity management. By leveraging pharmacogenomics and biomarker-driven algorithms, clinicians can tailor dosing to individual patient profiles, enhancing efficacy while minimizing adverse effects. This individualized approach challenges the conventional one-size-fits-all model and underscores the necessity of dynamic, data-informed adjustments in clinical practice.
Digital Health Platforms Amplify Treatment Success
Adoption of telemedicine, wearable technology, and mobile health applications enables continuous patient monitoring and real-time dosage optimization. These digital tools foster improved adherence, timely side effect management, and sustained engagement, thereby maximizing the therapeutic potential of Ozempic within multidisciplinary weight loss programs. This evolution toward connected care models improves accessibility and supports long-term weight loss maintenance.
Synergistic Multi-Modal Interventions Enhance Outcomes
Combining Ozempic with adjunct therapies such as nutraceuticals, behavioral interventions informed by neuroscience, and emerging metabolic modulators creates synergistic effects that address both biological and psychological facets of obesity. This comprehensive strategy not only accelerates fat loss but also improves durability of results by targeting underlying mechanisms of appetite control and energy balance.
Pharmacokinetic Modeling Elevates Safety in Complex Patients
Advanced pharmacokinetic simulations allow clinicians to predict drug plasma levels and optimize Ozempic dosing in patients with comorbidities, renal impairment, or polypharmacy. This proactive approach mitigates risks of toxicity and drug interactions, ensuring safer, more effective treatment regimens tailored to complex clinical scenarios.
Curated Expert Resources
New England Journal of Medicine (2023) – Offers a comprehensive review of semaglutide’s metabolic effects and evolving role in obesity treatment, critical for understanding the cutting-edge science behind Ozempic’s efficacy (NEJM 2023 Review on Semaglutide in Obesity).
Weight Loss Suppliers – Doctor-Supervised Ozempic Treatments provides detailed guidance on optimizing dosage and managing side effects under medical supervision, reflecting best practices in clinical weight loss (Optimize Your Dosage Safely).
Obesity Reviews (2024) – Digital Interventions in Obesity Care presents evidence on the impact of integrating digital health platforms with pharmacotherapy, supporting clinicians in adopting technology-enhanced weight loss strategies (Obesity Reviews 2024).
National Center for Biotechnology Information – AI in Personalized Medicine explores artificial intelligence applications in optimizing pharmacotherapy, including predictive modeling for Ozempic responsiveness (NCBI AI in Personalized Medicine).
Weight Loss Suppliers – Navigating Ozempic Side Effects details effective clinical approaches to managing common adverse events, essential for maintaining patient compliance (Side Effects Management).
Final Expert Perspective
Ozempic’s emergence as a cornerstone in medical weight loss clinics exemplifies the convergence of pharmacological innovation and personalized care. The advanced understanding of its multifaceted mechanisms, combined with precision medicine, digital health integration, and synergistic therapeutic combinations, is redefining obesity management. By embracing these expert insights and leveraging authoritative resources, clinicians can harness Ozempic’s full potential to deliver safer, more effective, and sustainable weight loss outcomes. We encourage healthcare professionals and engaged patients alike to deepen their exploration of tailored Ozempic programs and share insights through professional forums to collectively advance the field. For a comprehensive look at physician-guided treatment frameworks, visit doctor-supervised Ozempic treatments and discover how expert care elevates success rates.


I found this detailed breakdown of Ozempic’s role in weight management really insightful. Its multifaceted mechanism—reducing appetite while improving metabolic health—makes it a strong addition to comprehensive treatment plans. In my experience working with patients, the emphasis on physician-guided dosing and side effect management is crucial for adherence. I wonder, how do clinics balance the risks of gastrointestinal side effects with the need for effective weight loss? Have others observed that gradual dose escalation significantly improves tolerability? It seems like integrating digital health tools can further personalize therapy and enhance compliance, especially for patients who might struggle with side effects initially. I’m curious if anyone has implemented AI or pharmacogenomic screening to tailor dosing even further, and how that has influenced outcomes. Overall, Ozempic appears to mark a significant step forward, but the individualization of treatment seems to be key to maximizing its benefits.
It’s fascinating to see how Ozempic has become a pivotal tool in the multidisciplinary approach to weight loss. From my experience working in a clinic, I’ve noticed that patient education about the importance of gradual dose escalation really makes a difference in tolerability. Managing gastrointestinal side effects proactively encourages adherence and long-term success. I also wonder, with the advent of pharmacogenomics, how soon will we see personalized dosing protocols that consider genetic profiles? Such advancements could optimize outcomes further and reduce trial-and-error periods. Has anyone here integrated genetic testing into their weight management protocols with promising results? It seems like combining this with digital health tools and AI could truly transform individualized treatment plans, ensuring each patient receives the most effective and safe therapy. The evolution of these techniques makes me optimistic about the future of obesity treatment—what innovative strategies have you found most effective in clinical practice?
Reading through the insights on Ozempic’s role in weight management, I was particularly struck by the emphasis on personalized dosing and the importance of a multidisciplinary approach. In my practice, I’ve noticed that when clinics take the time to educate patients about gradual dose escalation and actively manage side effects, compliance greatly improves. I recently started incorporating simple digital tools like mobile health apps to track side effects and adherence, which seems to support individual tailoring even further. Have others found that integrating these technologies enhances patient outcomes? I also wonder about the future potential of pharmacogenomic testing; given the current costs and accessibility, do you think it will become standard in the next 5-10 years? Overall, I believe the evolution toward precision medicine in weight loss programs will make treatments like Ozempic even more effective and safer for diverse patient populations.
I’ve experienced firsthand how integrating digital tools like apps and remote monitoring can significantly boost patient engagement and adherence during Ozempic therapy. When patients track their side effects and weight changes systematically, it often leads to quicker adjustments and better tolerability. From a clinical perspective, this kind of detailed tracking not only informs dosage adjustments but also helps identify early signs of adverse reactions before they become problematic. About pharmacogenomics, I believe cost and accessibility are still barriers, but the rapid advancement in testing technologies might make personalized medicine more feasible in the near future. Do you think that as these tests become cheaper, we’ll see a shift towards routine genetic screening before starting therapies like Ozempic? I’m curious how others see this evolving in typical practice settings and whether personalized protocols can truly enhance outcomes across diverse populations.