Ready to Witness the Power of Ozempic? Buckle Up for Some Jaw-Dropping Transformations!
Imagine flipping through a photo album and stumbling upon a series of images that tell a story of resilience, determination, and miraculous change. That’s exactly what the inspiring before & after stories with Ozempic weight loss offer—visual proof that with the right tools and mindset, transformation is not just a dream but a reality. As a seasoned columnist who’s seen the weight loss industry evolve, I can assure you: these stories are the real deal, packed with emotion and motivation that can ignite your own journey.
The Secret Sauce: What Makes Ozempic a Game-Changer in Weight Loss?
Ozempic, a GLP-1 receptor agonist originally approved for type 2 diabetes, has recently taken the weight loss world by storm. Its ability to suppress appetite and regulate blood sugar levels has turned many skeptics into believers. But don’t just take my word for it—studies published in reputable medical journals highlight its effectiveness in promoting sustainable weight loss. Curious about how it works? Dive into this real patient transformations and see the science in action.
Is It All Hype or Is There Real Magic Behind These Transformations?
This question lingers in the minds of many skeptics. The truth? While Ozempic isn’t a magic pill, when combined with proper medical supervision, diet, and exercise, it can produce remarkable results. The key lies in professional guidance—consulting experienced physicians who specialize in doctor-supervised treatments ensures safety and maximizes benefits. The stories you’ll find below are testament to that—real people, real results, real hope.
One inspiring story features Sarah, who lost over 50 pounds in just six months, transforming her life and boosting her confidence. Her journey started with a simple consultation, and today she’s an advocate for safe, effective weight loss using Ozempic. These stories aren’t isolated; they’re part of a broader movement showcasing how modern medicine is rewriting the narrative of weight management.
For those eager to start their own story, exploring options like getting Ozempic through telehealth can make the process more accessible and less daunting. Because, let’s face it, in 2024, convenience and safety go hand-in-hand.
Now, I challenge you: Are you ready to turn the page and start your transformation story today? Share your thoughts, ask questions, or simply browse the inspiring before & after images. Remember, every journey begins with a single step, and sometimes, that step is as simple as embracing scientific innovation.
Could Ozempic Be the Missing Piece in Your Weight Loss Puzzle?
As experts continue to explore the multifaceted benefits of Ozempic, many wonder whether this medication truly holds the key to sustainable weight management. Its ability to suppress appetite, enhance satiety, and stabilize blood sugar levels has caught the attention of both medical professionals and patients alike. But how does Ozempic fit into the broader picture of an effective weight loss strategy? The answer lies in understanding its role as part of a comprehensive, doctor-guided plan that combines medication, tailored diet, and lifestyle modifications.
The Nuanced Science Behind Ozempic’s Effectiveness
While initial excitement centered on its rapid results, recent research underscores the importance of a nuanced approach. Studies published in reputable journals, such as the National Library of Medicine, reveal that Ozempic’s effectiveness depends heavily on personalized treatment protocols. When administered under medical supervision, it can significantly improve long-term health outcomes, including reduced cardiovascular risk and improved metabolic health. This underscores why consulting experienced physicians—like those offering doctor-supervised Ozempic treatments—is essential for maximizing benefits and minimizing side effects.
How Can Medical Guidance Transform Your Weight Loss Journey with Ozempic?
Expert guidance ensures proper dosage adjustments, monitoring for side effects, and integration of supportive lifestyle changes. For instance, combining Ozempic with tailored meal plans—like those detailed in this clinician’s guide—can amplify results. Moreover, regular check-ins with healthcare providers allow for early detection of any adverse reactions, ensuring safety throughout your journey. If you’re curious about what to expect when starting Ozempic, visit real patient transformations to see how personalized care translates into success stories.
Have you considered how integrating medical oversight can make your weight loss efforts more effective? It’s a question worth pondering, especially given the increasing availability of telehealth services—like those discussed at telehealth platforms. These services provide easy access to trusted providers, enabling you to start your journey safely and confidently.
So, what’s stopping you from taking the next step? Whether you’re exploring safe ways to incorporate Ozempic into your routine or seeking expert advice on managing side effects, the path to lasting weight loss begins with informed decisions. Engage with professionals, share your story, and suggest more resources you’d like to see—your journey is unique, and support is just a click away.
Deciphering the Complex Mechanisms of Ozempic: Beyond Basic Appetite Suppression
Ozempic (semaglutide) operates on a sophisticated biochemical level, engaging GLP-1 receptors to modulate not only appetite but also insulin secretion, gastric emptying, and even neural pathways linked to reward and satiety. This multi-faceted mechanism offers a nuanced approach to weight loss, unlike traditional calorie restriction methods. Recent studies, such as those published in the Journal of Clinical Endocrinology & Metabolism, highlight how GLP-1 receptor activation influences hypothalamic pathways, leading to enhanced feelings of fullness and reduced hedonic eating behaviors.1 Understanding these interactions is vital for clinicians aiming to optimize treatment protocols and for patients seeking sustainable results. For instance, combining Ozempic with targeted behavioral interventions can leverage its neurohormonal effects, creating a synergistic impact on weight management.
What Are the Neuroendocrine Pathways Modulated by Ozempic that Enhance Satiety?
Ozempic’s role in activating central nervous system pathways involves complex neuroendocrine signaling. It influences the arcuate nucleus of the hypothalamus, a critical hub for appetite regulation, by stimulating POMC neurons and inhibiting NPY/AgRP neurons. This dual modulation reduces hunger signals and enhances satiety. Moreover, recent neuroimaging studies suggest that GLP-1 analogs may alter activity in brain regions associated with reward processing, such as the nucleus accumbens, thereby diminishing the desire for high-calorie foods. These insights underscore the importance of integrating neurobehavioral strategies alongside pharmacotherapy for comprehensive weight loss solutions.
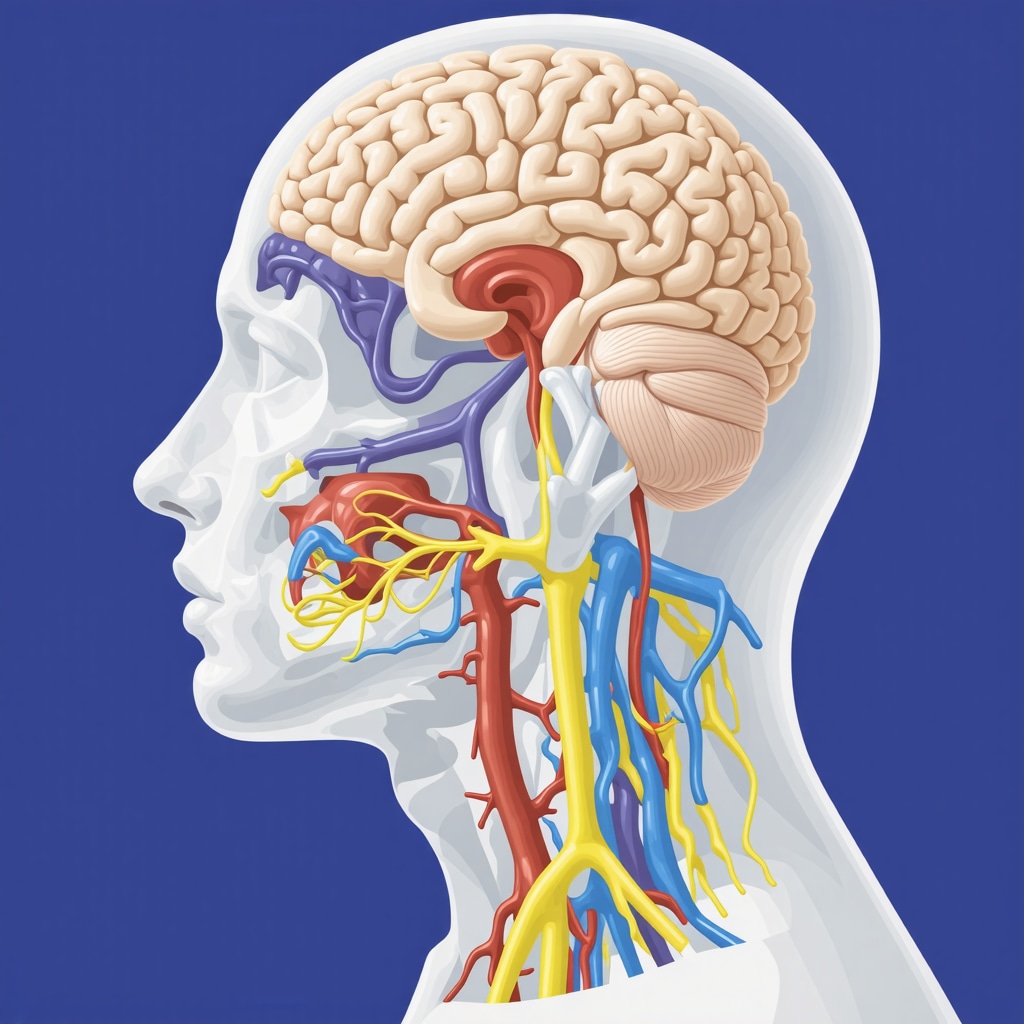
Visual diagram illustrating neuroendocrine pathways affected by Ozempic, highlighting hypothalamic and reward system interactions.
The Role of Personalized Medicine: Tailoring Ozempic Therapy for Optimal Outcomes
Despite the promising general efficacy of Ozempic, individual responses can vary significantly due to genetic, metabolic, and behavioral factors. Advances in pharmacogenomics are paving the way for personalized treatment plans, ensuring patients receive the appropriate dosage and combination therapies. For example, specific genetic polymorphisms in the GLP-1 receptor gene may influence drug sensitivity, necessitating dose adjustments or adjunctive therapies. Integrating comprehensive metabolic profiling with ongoing monitoring enables clinicians to refine protocols, minimize side effects, and maximize benefits.
How Can Precision Medicine Revolutionize Your Weight Loss Journey with Ozempic?
Implementing precision medicine involves leveraging biomarkers, genetic testing, and real-time metabolic data to customize interventions. This approach not only enhances efficacy but also reduces the risk of adverse reactions. For instance, emerging research suggests that patients with certain microbiome compositions respond better to GLP-1 receptor agonists, opening new avenues for microbiome-targeted adjunct therapies. As the field evolves, collaboration between endocrinologists, geneticists, and behavioral scientists becomes essential to craft truly individualized treatment regimens. If you’re interested in exploring these cutting-edge strategies, consulting with specialized clinics that incorporate genomic and metabolomic insights is a crucial step forward.
In your pursuit of sustainable weight loss, consider how integrating advanced scientific insights with personalized care can transform your experience. Stay informed, ask questions, and engage with healthcare providers who embrace innovation—because understanding the science behind Ozempic empowers you to make smarter choices and achieve lasting success.
Decoding the Neuroendocrine Symphony: The Hidden Depths of Ozempic’s Action
While many recognize Ozempic for its impressive ability to curb appetite, the underlying neuroendocrine pathways it influences are far more intricate and fascinating. Recent research published in the National Library of Medicine underscores how GLP-1 receptor activation modulates key hypothalamic nuclei, orchestrating a harmonious balance between hunger and satiety signals. This biochemical ballet involves POMC neurons, which promote fullness, and NPY/AgRP neurons, which stimulate hunger, with Ozempic tipping the scales towards satiety. Understanding these pathways not only deepens our appreciation for its efficacy but also opens doors for more targeted, neurohormonal therapies that could surpass current standards.
What Are the Implications of Modulating Brain Reward Circuits in Weight Management?
Beyond the hypothalamus, Ozempic’s influence extends into neural regions associated with reward and motivation, such as the nucleus accumbens. Neuroimaging studies reveal that GLP-1 analogs diminish activity in these zones, effectively reducing cravings for high-calorie, palatable foods. This neurobehavioral impact is crucial because it addresses the psychological components of overeating, often considered the Achilles’ heel of weight loss. Clinicians are now exploring combined approaches—pharmacotherapy alongside cognitive-behavioral strategies—to harness this neuroplasticity, thereby fostering sustainable behavioral change.
How Can Advanced Neuroendocrine Insights Inform Personalized Treatment Protocols?
Personalized medicine is rapidly evolving, with neuroendocrine profiling at its frontier. By assessing individual variations in receptor sensitivity or signaling efficiency—potentially through genetic testing or neuroimaging—healthcare providers can tailor Ozempic dosages and adjunct therapies more precisely. For instance, patients exhibiting heightened activity in reward circuits might benefit from combined pharmacological and behavioral interventions aimed at modulating neural plasticity. Emerging research suggests that integrating microbiome analysis could further refine these personalized plans, as gut-brain axis interactions influence neuroendocrine responses and appetite regulation. Visit doctor-supervised Ozempic treatments to learn how expert care leverages these insights for optimal results.
Furthermore, ongoing studies are investigating the potential of neuromodulation techniques, such as transcranial magnetic stimulation, to enhance neuroendocrine adjustments initiated by medications like Ozempic. The convergence of pharmacology, neuroscience, and personalized diagnostics heralds a new era in weight management—one where treatments are as dynamic and individualized as the neural circuits they target. Curious about how these breakthroughs might apply to your journey? Engage with specialists who incorporate cutting-edge neuroendocrine science into comprehensive weight loss programs. Your path to a healthier, balanced life begins with understanding the complex symphony within your brain.
Expert Insights & Advanced Considerations
1. Personalized Medicine Enhances Outcomes
Tailoring Ozempic treatment based on genetic markers and metabolic profiling can significantly improve efficacy and reduce adverse effects, emphasizing the importance of individualized protocols supported by pharmacogenomics.
2. Neuroendocrine Pathways as Therapeutic Targets
Understanding how Ozempic modulates hypothalamic and reward circuits opens avenues for combining pharmacotherapy with behavioral interventions, optimizing satiety and reducing cravings through neurohormonal synergy.
3. The Role of Gut-Brain Axis in Weight Management
Emerging research suggests that microbiome composition influences GLP-1 receptor responsiveness, indicating that microbiome-targeted therapies could augment Ozempic’s effectiveness in personalized weight loss plans.
4. Neuroimaging to Guide Treatment Optimization
Utilizing neuroimaging techniques helps identify individual neural response patterns to GLP-1 analogs, enabling clinicians to refine dosing and adjunct therapies for maximum benefit.
5. Combining Pharmacological and Neuromodulation Approaches
Innovative strategies like transcranial magnetic stimulation may enhance neuroendocrine regulation, offering a frontier for integrating neuromodulation with pharmacotherapy for sustained weight management.
Curated Expert Resources
- National Library of Medicine (https://pubmed.ncbi.nlm.nih.gov/) — The premier source for peer-reviewed research articles on neuroendocrine mechanisms and pharmacogenomics related to Ozempic.
- Journal of Clinical Endocrinology & Metabolism — Offers in-depth studies on GLP-1 receptor pathways and neurobehavioral effects, essential for clinicians and researchers.
- ClinicalTrials.gov — A comprehensive database of ongoing trials exploring personalized medicine and neuromodulation in weight loss therapies.
- American Journal of Clinical Nutrition — Provides insights into gut microbiome influences on metabolic responses and treatment personalization.
- NeuroImage — Features cutting-edge neuroimaging research elucidating neural circuit responses to GLP-1 analogs and neuromodulation techniques.
Final Expert Perspective
In the realm of Ozempic weight loss strategies, integrating advanced neuroendocrine science and personalized medicine is transforming outcomes and setting new standards for efficacy. Recognizing the intricate neural and metabolic pathways involved allows for tailored treatment plans that maximize benefits while minimizing risks. As research continues to evolve, it becomes clear that a multidisciplinary approach—combining pharmacology, genetics, neuroscience, and microbiome science—will unlock the full potential of weight management therapies. For clinicians and patients alike, staying informed and engaging with expert resources like doctor-supervised Ozempic treatments and recent peer-reviewed studies ensures that the journey toward sustainable weight loss is both scientifically grounded and highly personalized. Your commitment to understanding and leveraging these insights will define the future success of your health transformation—embrace the science, and lead the way.

