Is Ozempic the Secret Weapon in Your Weight Loss Arsenal?
Imagine this: you’re at your wit’s end, trying every diet and gym routine under the sun, only to find yourself stuck in a frustrating plateau. Then, a friend whispers about Ozempic — a medication that’s been making waves in the weight loss community. But here’s the kicker: it’s not just about popping pills; it’s about a medically-supervised journey that could finally help you achieve those elusive weight goals.
Why the Buzz About Medically-Supervised Ozempic Treatments?
Ozempic, known scientifically as semaglutide, is a GLP-1 receptor agonist originally developed for managing type 2 diabetes. However, its remarkable ability to curb appetite and promote satiety has caught the attention of weight loss experts. When administered under medical supervision, Ozempic offers a safe, effective pathway to shedding pounds — especially for those who’ve struggled with traditional methods.
The Inside Scoop: How Does It Work?
Think of Ozempic as your new best friend in a fight against hunger. It mimics the hormone GLP-1, which signals your brain to feel full and satisfied. This means fewer cravings, less overeating, and ultimately, weight loss. But, like all medications, it’s not a magic bullet. Proper medical guidance ensures you’re using it safely and maximizing benefits. Want to learn more? Check out how Ozempic works for medical weight loss.
Is It Just About the Pills or Something More?
Medically-supervised treatments aren’t just about handing out prescriptions—they’re about crafting a comprehensive plan tailored to your unique needs. With the oversight of a healthcare provider, you can navigate potential side effects, adjust dosages, and integrate lifestyle changes that reinforce your weight loss journey. It’s a partnership built on trust, expertise, and real results.
Questions That Might Be Running Through Your Mind
How do you even get started? Are there clinics near you offering safe Ozempic treatments? And what about costs and insurance? These are valid questions that deserve honest answers. For instance, exploring reputable clinics that prioritize patient safety can make all the difference. You can find top-rated options in your area by visiting best Ozempic clinics near you.
Additionally, telehealth services are revolutionizing access, making it easier and more discreet to get your treatment. Curious about how to access Ozempic via telehealth? Check out telehealth Ozempic prescriptions.
Let’s Talk About Results — The Proof Is in the Photos
Real stories, real transformations. Many patients share inspiring before-and-after photos that showcase the effectiveness of supervised Ozempic treatments. Want to see the stunning results? Visit real patient transformations and get inspired.
Remember, success isn’t just about the medication; it’s about a holistic approach involving diet, exercise, and ongoing medical support. So, if you’re ready to take control of your weight loss journey, consulting a healthcare provider about Medically-Supervised Ozempic Treatments might just be your game-changer.
Have you tried Ozempic or are you considering it? Share your thoughts and experiences in the comments below. Your story could motivate someone else to start their own transformation!
And for a deeper dive into the science behind Ozempic’s effectiveness, visit FDA’s official site for credible insights.
Is Your Weight Loss Strategy Missing a Critical Piece?
While medications like Ozempic have revolutionized weight management, the secret to long-term success often lies in how these treatments are integrated into your broader lifestyle. A question worth pondering is: are you leveraging all the tools available to maximize your results? Beyond the medication itself, factors such as personalized nutrition plans, behavioral therapy, and ongoing medical support play crucial roles. Recent studies, including those highlighted by the FDA, emphasize that a multifaceted approach enhances sustainability and mitigates potential setbacks.
How Can You Tailor Your Ozempic Journey for Lasting Results?
Expert insights suggest that pairing Ozempic with lifestyle modifications—like a balanced diet rich in whole foods, regular physical activity, and stress management—significantly boosts its effectiveness. Consulting with healthcare providers for a personalized plan ensures you address unique health considerations, optimize dosage, and navigate side effects safely. Curious about the latest strategies? Check out doctor-supervised Ozempic treatments for a comprehensive understanding.
Furthermore, embracing a holistic approach includes mental health support to tackle emotional eating and motivation challenges. This integrated method not only accelerates weight loss but also fosters habits that sustain it beyond medication use.
What Are the Hidden Benefits of Combining Medical Support with Lifestyle Changes?
Combining Ozempic with structured support systems can dramatically improve adherence and outcomes. For example, engaging with a certified weight loss clinic offers accountability and expert guidance, which are vital during the initial phases of treatment. Many patients report that their success stories are rooted in consistent medical oversight, as detailed in top-rated clinics.
Additionally, ongoing education about potential side effects and how to manage them empowers patients, reducing anxiety and improving compliance. Telehealth services, for instance, have expanded access, making it easier and more discreet to receive expert advice. Want to explore more about this? Discover telehealth Ozempic options.
Could Your Weight Loss Journey Be More Than Just a Number on the Scale?
Absolutely. The true measure of success extends beyond the mirror — it encompasses improvements in energy levels, metabolic health, and overall well-being. Patients who combine medication with behavioral modifications often report better mental health and confidence, fueling motivation for continued progress. For compelling real-life stories, visit patient transformations.
If you’re contemplating how to optimize your weight loss journey with Ozempic, remember: the key is a balanced, supportive framework that encourages sustainable habits. Engage with reputable clinics, stay informed about emerging research, and connect with a healthcare team dedicated to your success.
Have you experienced or considered combining Ozempic with lifestyle changes? Share your insights or questions in the comments below — your story might inspire someone else to start their journey!
For trusted guidance and latest updates on Ozempic, visit trusted Ozempic suppliers.
Beyond the Surface: The Neuroendocrine Impact of Ozempic on Appetite Regulation
While most discussions focus on Ozempic’s role in suppressing appetite through GLP-1 receptor activation, emerging research reveals its profound influence on the neuroendocrine system. Semaglutide, the active compound in Ozempic, modulates not only peripheral metabolic pathways but also central nervous system circuits involving the hypothalamus, which orchestrates hunger signals. According to a 2022 study published in Nature Metabolism, semaglutide crosses the blood-brain barrier, altering neuronal activity in appetite-regulating regions, thus providing a dual mechanism that enhances satiety and reduces caloric intake over extended periods. This neuroplasticity might explain the sustained weight loss observed in long-term users and opens avenues for targeted therapies that optimize neural pathways involved in energy homeostasis.
What Are the Long-Term Neurological Adaptations to Continued Ozempic Use?
Understanding the brain’s adaptive responses is crucial for anticipating potential tolerance or neurochemical shifts. Chronic activation of GLP-1 pathways could induce receptor desensitization or influence neurogenesis in appetite centers, potentially impacting efficacy over time. Current animal models suggest a need for periodic assessment of neural plasticity markers during prolonged therapy. Clinicians should consider integrating neurocognitive evaluations into treatment plans, especially for patients with comorbid neurological conditions, to tailor interventions that sustain the neuroprotective benefits while mitigating adaptation risks.
Synergizing Pharmacology with Personalized Lifestyle Interventions for Sustainable Results
The integration of advanced pharmacotherapy like Ozempic with individualized lifestyle modifications is not merely additive but synergistic. Personalized nutrition plans, rooted in genetic and microbiome analyses, can potentiate the drug’s effects by aligning dietary patterns with metabolic predispositions. Moreover, behavioral therapies that address emotional eating and stress management are critical; they reinforce neural pathways associated with healthy habits, making the medication’s impact more durable. A comprehensive approach, supported by data from the NIH, ensures that weight loss is maintained well beyond the cessation of pharmacological intervention.
How Can Advanced Data Analytics Enhance Personalization of Ozempic-Based Treatments?
Integrating wearable technology and AI-driven analytics offers a frontier for customizing Ozempic regimens. Continuous monitoring of physiological parameters such as glucose levels, heart rate variability, and sleep patterns can inform dynamic dosage adjustments and behavioral recommendations. Predictive modeling, leveraging machine learning algorithms trained on large datasets, can identify early signs of metabolic plateau or side effects, enabling preemptive modifications. This real-time, precision medicine approach not only maximizes efficacy but also minimizes adverse events, paving the way for a new era of bespoke obesity management.
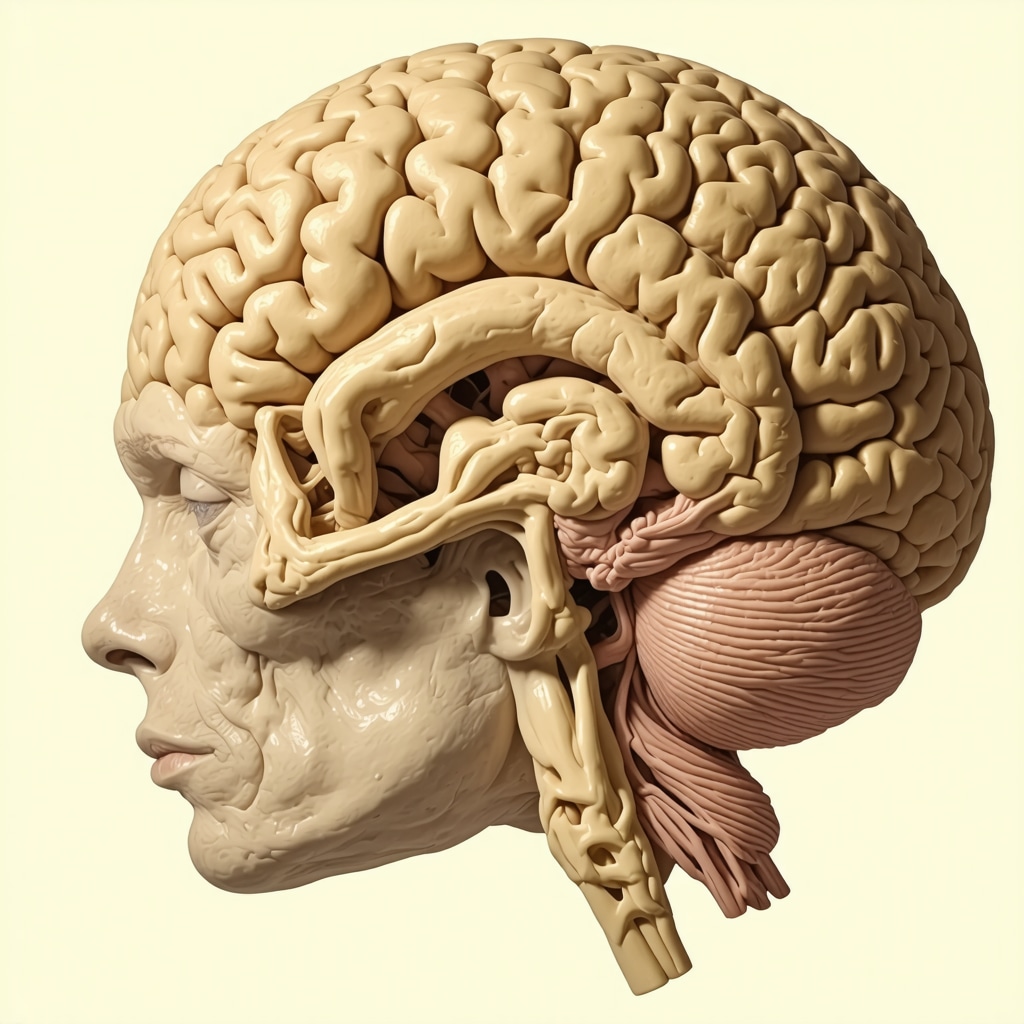
Visualize the neuroendocrine pathways affected by Ozempic, highlighting the hypothalamus and neural circuits involved in appetite regulation, to enhance understanding of its central effects on weight loss.
The Future of Weight Management: Integrating Neurobiology, Pharmacology, and Technology
As our comprehension deepens, the convergence of neurobiology, advanced pharmacology, and digital health tools promises a paradigm shift in obesity treatment. Researchers are exploring combination therapies that target multiple neural pathways, potentially reducing the dosage requirements and side effects of medications like Ozempic. Simultaneously, digital platforms facilitate patient engagement, adherence, and real-time feedback, transforming the treatment landscape into a personalized, tech-enabled ecosystem. This holistic integration aims to deliver not only weight loss but also improved metabolic resilience and mental health.
What Are the Ethical and Practical Considerations in Deploying AI-Enhanced Weight Management Solutions?
The deployment of AI and big data in personalized medicine raises important questions about data privacy, equitable access, and clinical validation. Ensuring that these innovations are ethically implemented involves rigorous regulation, transparency, and inclusivity to prevent disparities. Moreover, clinicians must be trained to interpret complex analytics and incorporate them into holistic care. As these technologies evolve, ongoing research and policy development are essential to balance innovation with patient safety and societal benefit.
If you’re eager to stay ahead in the evolving landscape of weight management, consider consulting with specialists who integrate neurobiological insights, cutting-edge pharmacology, and digital health tools into tailored treatment plans. Your journey toward sustainable weight loss can benefit immensely from this multidisciplinary approach, ensuring both safety and effectiveness.
Could Ozempic’s Neuroendocrine Effects Hold the Key to Long-Term Weight Management?
While the primary discussion around Ozempic centers on its peripheral metabolic actions, recent neurobiological research uncovers a fascinating dimension: its profound influence on the brain’s appetite regulation circuitry. Semaglutide, the active component of Ozempic, traverses the blood-brain barrier, directly modulating neurons within the hypothalamus—often regarded as the brain’s hunger command center. This neuroendocrine interaction not only amplifies satiety signals but might also induce neuroplastic changes that sustain weight loss beyond the pharmacological effects, according to a 2022 study published in Nature Metabolism. Understanding these neural pathways provides a new frontier for personalized, neural-targeted obesity treatments.
How Do Neural Adaptations Influence Ozempic’s Efficacy Over Time?
Chronic activation of GLP-1 receptors in the brain may lead to receptor desensitization or neuroplastic shifts, which could potentially diminish the drug’s appetite-suppressing effects over extended periods. Insights from animal models suggest that periodic neurocognitive assessments and adaptive dosing strategies might mitigate tolerance development. Integrating neuroimaging and neurochemical monitoring could enable clinicians to fine-tune treatments, ensuring sustained neural engagement and long-term efficacy. For a comprehensive understanding, explore the detailed mechanisms in NIH’s latest neuroendocrine research.
Synergizing Pharmacology and Neural Plasticity for Enduring Results
The convergence of pharmacological innovation with neuroplasticity principles heralds a new era in weight management. Personalized interventions could involve combining Ozempic with cognitive behavioral therapies that target neural pathways associated with emotional eating and reward processing. Such integrative approaches may reinforce neural circuits favoring healthy habits, making weight loss more durable. Recent advancements in neurofeedback and brain stimulation techniques also hold promise for augmenting pharmacotherapy, as discussed in recent neuroscience reviews. This multifaceted strategy could reduce reliance on medication in the long run, fostering sustainable weight control.
What Role Can Digital Neurotechnology Play in Enhancing Personalized Weight Loss?
Emerging digital health tools, including wearable neurofeedback devices and AI-powered behavioral analytics, are poised to revolutionize personalized weight management. These technologies can monitor neural and behavioral markers in real-time, providing insights that inform dynamic treatment adjustments. For example, tracking stress-related neural responses might help tailor interventions to reduce emotional eating episodes. The integration of such neurotechnology with pharmacotherapy could optimize neural engagement, ensuring that each patient’s unique neurobiological profile guides their weight loss journey. For more on this innovative frontier, see latest neurotech developments in weight management.
Beyond the Brain: The Future of Neuroendocrine-Driven Weight Solutions
As research continues to unravel the neuroendocrine intricacies of appetite regulation, future therapies may involve targeted neuromodulation or gene editing techniques aimed at specific neural circuits. Combining these cutting-edge modalities with existing pharmacotherapies like Ozempic could significantly enhance efficacy, reduce side effects, and promote long-term metabolic resilience. Ethical considerations and rigorous clinical trials will be paramount in translating these innovations from laboratory to clinic. The integration of neurobiology, pharmacology, and digital health promises a comprehensive, personalized approach that addresses the root causes of obesity, rather than just symptoms.
Are you intrigued by the neurobiological dimensions of weight loss? Share your thoughts or questions below, and join the conversation on how neuroscience is shaping the future of obesity treatment!
Expert Insights & Advanced Considerations
Neuroendocrine Modulation and Long-Term Efficacy
Recent research underscores Ozempic’s profound impact on neural circuits involved in appetite regulation, highlighting its potential to induce neuroplastic changes that support sustained weight loss. Understanding these mechanisms can guide clinicians in optimizing treatment durations and dosing strategies to prevent receptor desensitization and maximize neuroprotective benefits.
Integrating Pharmacology with Personalized Medicine
The synergy between GLP-1 receptor agonists like Ozempic and personalized interventions—such as genomics-informed nutrition and behavioral therapy—represents the frontier of effective weight management. Tailoring treatments based on individual metabolic and neurobiological profiles enhances durability and reduces side effects.
Neurotechnology and Digital Biomarkers
Emerging neurofeedback devices and AI-driven behavioral analytics offer promising avenues to monitor neural responses in real-time, enabling dynamic adjustments to therapy. These tools facilitate a precision medicine approach, ensuring neural pathways associated with satiety and reward are optimally engaged throughout treatment.
Curated Expert Resources
- Nature Metabolism: A leading journal publishing cutting-edge neuroendocrine research on GLP-1 analogs, providing insights into neural circuitry modulation by Ozempic.
- NIH Neuroplasticity Studies: Comprehensive data on neural adaptations to chronic GLP-1 receptor activation, essential for understanding long-term treatment effects.
- FDA Guidelines on GLP-1 Agonists: Authoritative regulatory framework for safe and effective use of medications like Ozempic, including emerging evidence-based practices.
- Recent Neuroscience Reviews: Syntheses of neurofeedback and neuromodulation techniques applicable to obesity management, highlighting innovative adjunct therapies.
Final Expert Perspective
As we advance into 2025, the integration of neurobiological insights with pharmacotherapy like Ozempic offers a promising path toward sustainable weight management. Understanding the neuroendocrine mechanisms and leveraging personalized neurotechnology can enhance treatment efficacy and long-term outcomes. For professionals and patients alike, staying informed through authoritative sources and engaging in multidisciplinary approaches remains paramount. If you’re committed to pushing the boundaries of weight loss strategies, explore collaborations with neuroendocrinologists, genetic counselors, and digital health innovators to craft truly tailored interventions. Your expertise and curiosity are vital in shaping the future of effective, science-driven obesity treatment.

