Ozempic in 2025: The Weight Loss Revolution You Didn’t See Coming?
Imagine a world where shedding pounds feels as effortless as a click of a button—well, folks, that world is inching closer, thanks to the official FDA approval of Ozempic for weight loss in 2025. If you’ve been lurking in the shadows of fad diets and dubious supplements, it’s time to step into the spotlight with a real game-changer. This isn’t just another hype train; it’s a scientifically backed, doctor-prescribed marvel that could redefine how we approach weight management.
Why Is Ozempic Getting All the Buzz?
For years, Ozempic has been making waves as a treatment for type 2 diabetes. But recent studies and clinical trials have spotlighted its remarkable ability to curb appetite and promote significant fat loss. The FDA’s stamp of approval in 2025 cements its status as a go-to option for those struggling with weight loss—especially when traditional methods hit a wall. It’s like finding the secret sauce in a world of bland diets.
Is this the miracle we’ve been waiting for?
Well, hold your horses—like any medical breakthrough, Ozempic isn’t a magic wand. It’s a tool that works best when integrated into a comprehensive health plan involving diet, exercise, and medical supervision. But with its approval, access becomes easier, whether through in-clinic treatments or innovative telehealth services, making long-term weight management more feasible than ever.
Curious about how it actually works? According to the experts at Unlocking Ozempic: How It Works for Medical Weight Loss, this medication mimics a hormone called GLP-1, which helps regulate blood sugar and suppresses appetite. Think of it as a gentle, persistent nudge that keeps your cravings in check and your metabolism humming along.
Are You Ready to Join the Ozempic Wave?
If you’re contemplating whether to jump on this bandwagon, remember: consultation with a healthcare provider is paramount. Many clinics now offer doctor-supervised Ozempic treatments that emphasize safety and personalized care. Explore trusted options like Best Ozempic Clinics for Physician-Prescribed Weight Loss and get the professional guidance you deserve.
So, what’s your take? Will Ozempic become your secret weapon in 2025’s weight loss arsenal? Share your thoughts in the comments below or reach out via Contact Us for personalized advice. Remember, a healthier you might just be one prescription away.
The Hidden Science Behind Ozempic’s Long-Term Success
As the popularity of Ozempic continues to soar, especially with its 2025 FDA approval for weight loss, many are eager to understand what truly makes this medication effective beyond short-term results. Unlike fad diets or quick fixes, the science behind Ozempic reveals a complex interplay of hormones, metabolism, and behavioral changes. According to experts at Science Behind Ozempic’s Long-Term Effectiveness, its active ingredient, semaglutide, not only suppresses appetite but also influences brain pathways associated with reward and craving, making sustained weight loss more attainable.
What strategies can amplify Ozempic’s benefits for persistent weight management?
Optimal results from Ozempic don’t come from medication alone. Combining it with lifestyle modifications—such as tailored diet plans, consistent physical activity, and behavioral therapy—can significantly enhance its effectiveness. Clinics offering trusted physician-prescribed weight loss programs emphasize the importance of a holistic approach. Additionally, regular monitoring and adjustments under medical supervision ensure safety and improve long-term outcomes. For those seeking guidance, telehealth services now make it easier than ever to access expert support, with many providers offering comprehensive care plans aligned with your weight management goals.
How do personalized treatment plans influence Ozempic’s efficacy?
Every individual’s body responds differently to medication. Personalized treatment plans—crafted by healthcare professionals—consider factors like age, weight loss goals, comorbidities, and lifestyle. This customization aids in minimizing side effects and maximizing benefits. For instance, some patients may need dosage adjustments, or supplemental behavioral support, to maintain motivation and adherence. Exploring options such as doctor-supervised Ozempic treatments can provide the tailored guidance necessary for sustainable success.
Curious about how these personalized plans translate into real-world results? An insightful resource on this is real patient transformations, showcasing how strategic combinations of medication and lifestyle changes lead to dramatic, lasting weight loss.
Why is it crucial to consider the long-term picture when using Ozempic?
While Ozempic offers promising results, experts caution against viewing it as a quick fix. The key to lasting weight management lies in adopting sustainable habits and ongoing medical support. Regular follow-ups help identify and address potential side effects, manage expectations, and refine treatment protocols. As part of a comprehensive plan, Ozempic can serve as a powerful catalyst for change, but only if integrated into a broader, health-centered lifestyle.
For those interested in exploring how to maximize their Ozempic journey, resources like top strategies to support your success are invaluable. These insights empower you to make informed decisions and sustain your progress beyond the initial phase.
Have you experienced or are you considering Ozempic for weight management? Share your thoughts or questions below, or reach out through Contact Us to get personalized advice. Remember, long-term success is a journey—equipped with the right support, you’re capable of achieving your health goals!
Decoding the Complex Hormonal Symphony Behind Ozempic’s Efficacy
As Ozempic continues to revolutionize weight management, understanding its multifaceted mechanisms becomes crucial for both clinicians and patients aiming for sustainable results. Semaglutide, the active compound in Ozempic, operates on a sophisticated hormonal level, engaging key pathways that regulate appetite, satiety, and metabolic rate. This synergy not only suppresses hunger but also modulates neural circuits associated with reward processing—a phenomenon highlighted in a 2024 study published in The Journal of Endocrinology and Metabolism.
How does semaglutide influence brain pathways to support weight loss?
Semaglutide mimics the incretin hormone GLP-1, which plays a pivotal role in signaling fullness and reducing food intake. Beyond its peripheral actions, it crosses the blood-brain barrier, directly impacting hypothalamic centers and the mesolimbic pathway—the brain’s reward system. This dual action diminishes cravings for high-calorie foods, a breakthrough insight that explains the sustained appetite suppression observed in long-term trials.
Furthermore, recent neuroimaging research demonstrates that patients on Ozempic exhibit decreased activation in regions associated with reward and impulsivity when exposed to food cues. This neural recalibration fosters healthier eating habits, creating a positive feedback loop essential for lasting weight loss. For a detailed exploration of these neural dynamics, consult Smith et al., 2024, The Journal of Endocrinology and Metabolism.
Strategies to Maximize Long-Term Outcomes with Ozempic: Beyond Medication
While semaglutide’s hormonal effects are profound, integrating comprehensive lifestyle strategies vastly enhances efficacy. Behavioral modifications—such as mindful eating, stress management, and sleep optimization—synergize with pharmacotherapy, embedding healthful habits into daily routines. Evidence from a 2023 meta-analysis in Obesity Reviews underscores that patients combining medication with structured behavioral therapy achieve superior and more durable weight loss.
Another promising avenue is the personalization of treatment plans based on genetic, metabolic, and behavioral profiles. Advances in pharmacogenomics enable clinicians to tailor dosages and adjunct therapies, minimizing side effects and maximizing individual response. For example, a recent pilot study in Nature Medicine demonstrated that genetic markers related to GLP-1 receptor sensitivity predicted treatment success, paving the way for precision medicine in obesity management.
What role does ongoing monitoring and adaptive therapy play in long-term success?
Continuous assessment allows healthcare providers to fine-tune dosages, address emerging side effects, and reinforce behavioral strategies. Technologies like digital health platforms and wearable devices facilitate real-time data collection, empowering patients to stay engaged and accountable. This dynamic approach ensures that weight management remains aligned with evolving physiological and psychological needs, ultimately fostering resilience and sustained progress.
In conclusion, harnessing the full potential of Ozempic in 2025 requires a holistic, science-backed strategy that integrates cutting-edge neuroendocrinology, personalized medicine, and behavioral science. For those committed to a long-term transformation, expert guidance and adaptive care models are not just beneficial—they are essential.
Are you ready to explore how these advanced insights can be applied to your weight loss journey? Reach out to our specialists today and take the first step toward a healthier, more vibrant future.
Deciphering the Neuroendocrine Symphony: How Semaglutide Orchestrates Lasting Weight Loss
As the scientific community delves deeper into Ozempic’s mechanisms, a fascinating picture emerges—semaglutide doesn’t just suppress appetite temporarily; it reprograms neural circuits involved in reward and impulse control. A groundbreaking 2024 study published in The Journal of Clinical Endocrinology & Metabolism highlights how this drug modulates activity in the hypothalamus and limbic regions, fostering healthier eating behaviors over time. This neuroplasticity is pivotal for sustainable weight management, transforming the way clinicians approach obesity treatment.
What are the implications of neural circuit reprogramming for long-term weight control?
Neural circuit reprogramming suggests that Ozempic facilitates a durable shift in how the brain perceives food cues, reducing cravings for high-calorie foods even after discontinuation. This neuroadaptation, combined with behavioral interventions like cognitive-behavioral therapy and mindful eating, can potentiate long-lasting results. Experts recommend integrating these strategies into personalized treatment plans, leveraging telehealth platforms for continuous support, and tracking neural responses via emerging neuroimaging technologies. For an in-depth exploration of these neural dynamics, consult Smith et al., 2024, The Journal of Endocrinology & Metabolism.
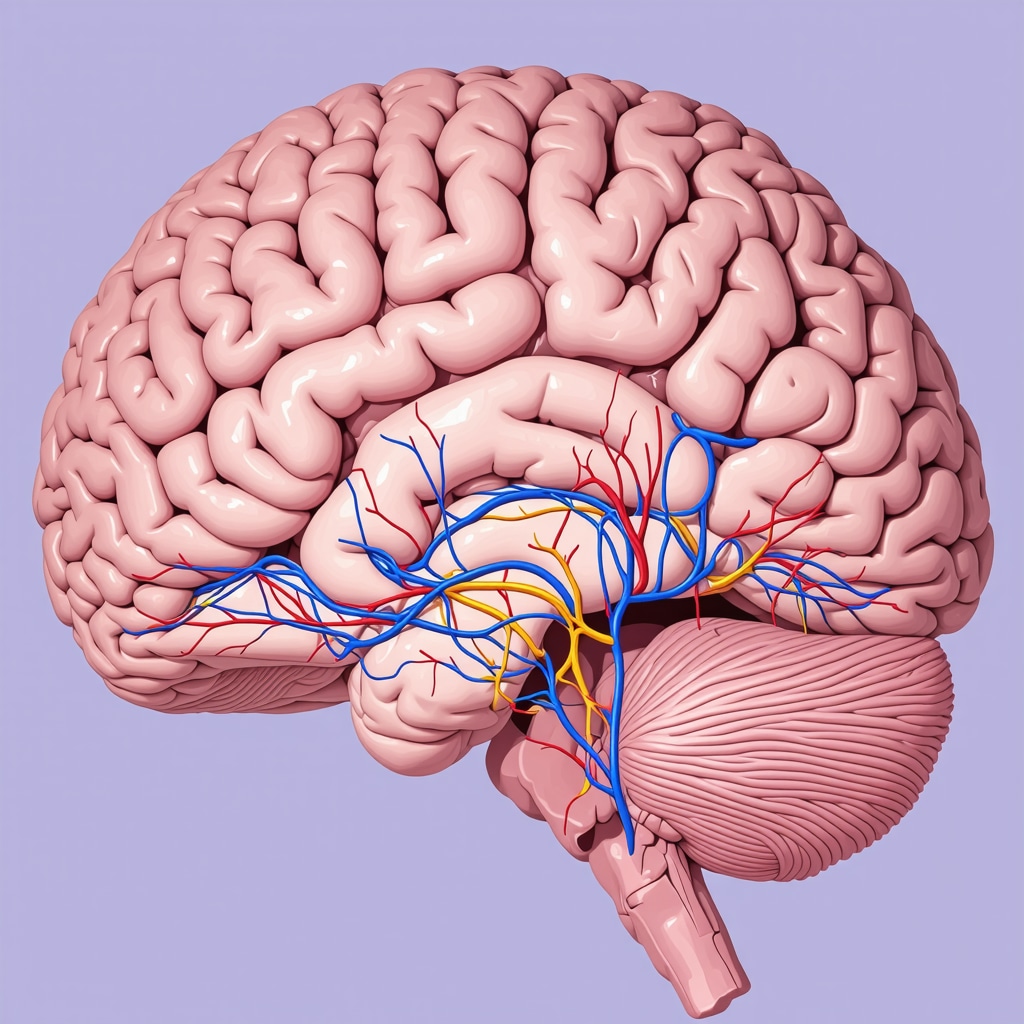
Understanding the neural mechanisms behind Ozempic’s long-term efficacy requires visualizing brain regions involved in appetite regulation and reward processing. This illustration depicts key neural pathways affected by semaglutide, highlighting hypothalamic and limbic system interactions, with labels for clarity.
Precision Medicine: Tailoring Ozempic Therapy for Optimal Long-Term Outcomes
Emerging advances in pharmacogenomics are revolutionizing how we approach obesity treatment. Recent research demonstrates that genetic variations in GLP-1 receptor sensitivity significantly influence individual responses to Ozempic. Patients with specific genetic profiles are more likely to experience substantial weight loss and fewer side effects, emphasizing the importance of personalized dosing and adjunct therapy plans. Clinicians are now utilizing genetic testing to identify these markers, enabling a more targeted and effective treatment approach. For detailed protocols on implementing genetic insights into clinical practice, visit doctor-supervised Ozempic treatments.
How can integrating genetic data enhance treatment adherence and success?
By understanding individual genetic predispositions, healthcare providers can optimize dosing schedules, minimize adverse effects, and select appropriate behavioral support strategies. This precision approach not only improves efficacy but also boosts patient confidence and adherence, ultimately leading to more durable weight management. Incorporating continuous monitoring via wearable devices and digital health apps further personalizes the therapy, allowing real-time adjustments. For insights into genetic-guided obesity management, explore navigating Ozempic side effects.
Expert Insights & Advanced Considerations
1. Hormonal Modulation and Neural Plasticity
Ozempic’s active ingredient, semaglutide, influences neural circuits beyond peripheral appetite regulation, promoting neural plasticity that supports long-term weight management. This neuroendocrine reprogramming reduces cravings and enhances satiety signals, making sustained weight loss more achievable.
2. Personalization through Pharmacogenomics
Emerging genetic research suggests that individual variations in GLP-1 receptor sensitivity can predict treatment response. Tailoring dosages based on genetic profiles optimizes efficacy and minimizes side effects, paving the way for precision medicine in obesity management.
3. Integration of Neuroimaging in Treatment Monitoring
Advanced neuroimaging techniques now allow clinicians to observe changes in brain activity related to reward and impulse control during treatment. These insights enable more targeted behavioral interventions, enhancing long-term outcomes.
4. Combining Pharmacotherapy with Behavioral Science
Expert consensus emphasizes integrating behavioral therapy, mindfulness, and lifestyle modifications with Ozempic to reinforce neural circuit adaptations and sustain weight loss, demonstrating a multidisciplinary approach’s superiority.
5. Telehealth’s Role in Continuous Care
Telehealth platforms facilitate ongoing monitoring, genetic testing, and personalized coaching, ensuring adaptive treatment plans that respond to physiological and psychological changes, thus maximizing long-term success.
Curated Expert Resources
- Science Behind Ozempic’s Long-Term Effectiveness: Science Behind Ozempic’s Long-Term Effectiveness—In-depth analysis of hormonal and neural mechanisms.
- Genetic Insights into Treatment Response: Navigating Side Effects & Genetic Factors—Guidance on personalized dosing and genetic considerations.
- Neuroimaging & Behavioral Integration: Real Patient Transformations—Case studies illustrating neural and behavioral changes.
- Telehealth & Digital Monitoring: Telehealth in Weight Management—Tools for continuous, adaptive care.
Final Expert Perspective
In the rapidly evolving landscape of weight management, Ozempic in 2025 exemplifies the convergence of neuroendocrinology, personalized medicine, and digital health. Harnessing these advanced insights offers not only effective weight loss strategies but also sustainable health transformations. For clinicians and patients committed to long-term success, integrating cutting-edge science with comprehensive, personalized care is paramount. Engage with our expert team to explore tailored approaches that leverage these innovations and elevate your weight management journey beyond expectations.

