Unveiling the Magic: What Do Ozempic Before and After Photos Really Tell Us?
Ever scrolled through social media or patient testimonials and wondered, “Is this for real?” Well, buckle up, because the world of Ozempic transformations is more than just slick Photoshop edits. From jaw-dropping weight loss to renewed confidence, these stories are rewriting the narrative on medical weight management.
The Secret Sauce: How Does Ozempic Work Its Magic?
Ozempic, a GLP-1 receptor agonist, helps regulate blood sugar and curbs appetite—kind of like having a personal chef whispering, “You don’t need that snack” every hour. Medical experts, such as endocrinologists, have lauded it for its ability to support sustainable weight loss, especially when combined with lifestyle changes. For an in-depth look, check out this detailed guide.
Is Your Weight Loss Journey Ready for a Transformation?
Imagine shedding those stubborn pounds and feeling energized enough to conquer your day. But wait—are all Ozempic stories alike? Not quite. Results vary based on dosage, diet, exercise, and individual biology. That’s why consulting with a physician is crucial. Curious about top clinics? Discover the best Ozempic clinics near you.
If you’re eager to see real-life proof, explore inspiring before and after photos of patients who transformed their lives with Ozempic.
Why Do These Success Stories Matter?
Because they represent hope, perseverance, and the power of modern medicine. These stories cut through the noise, showing that with proper guidance, real weight loss is achievable. Remember, though, that every journey is unique, and results depend on many factors—including adherence to prescribed treatment plans. For comprehensive insights, visit doctor-supervised Ozempic treatments.
So, are you ready to start your own transformation story? Share your thoughts below or reach out to local clinics to explore your options. Because sometimes, a little help from science and a dedicated medical team is all it takes to turn the page.
What Makes Ozempic a Game-Changer for Sustainable Weight Loss?
Ozempic’s reputation as a leading GLP-1 receptor agonist isn’t just based on anecdotal success stories but also on scientific validation. Its ability to regulate blood sugar and suppress appetite makes it a formidable tool for long-term weight management. According to a comprehensive review by the scientific community, the drug’s efficacy extends beyond immediate weight loss, supporting metabolic health and reducing the risk of comorbidities.
Could Ozempic Be the Key to Breakthroughs in Chronic Weight Management?
As an expert in medical weight management, I often ponder whether innovations like Ozempic can revolutionize how we approach obesity as a chronic condition rather than a temporary hurdle. The evidence suggests that with proper medical supervision and lifestyle integration, Ozempic can maintain weight loss over years, not just months. This long-term perspective is crucial, especially considering the ongoing debates about the best strategies for sustainable weight loss. Want to learn more about how top clinics are leveraging this approach? Visit top FDA-approved Ozempic clinics near you.
Moreover, for those wondering how to maximize their results, combining medication with personalized diet and exercise plans is essential. Studies show that integrated approaches yield better outcomes, making physician-guided treatments indispensable. Interested in seeing real results? Check out these inspiring before-and-after photos.
How Do You Navigate the Complexities of Long-Term Weight Management?
While Ozempic offers promising results, it’s vital to recognize the importance of ongoing medical oversight. Side effects, individual variability, and adherence challenges all play roles in the journey. Effective strategies include regular consultations, monitoring for side effects, and adjusting doses as needed. For tips on minimizing side effects and boosting results, explore top strategies to enhance your Ozempic experience.
Are you ready to embrace this new era of weight management? Share your thoughts below, or contact a qualified clinic to start your personalized plan. Remember, with science, proper guidance, and perseverance, achieving your long-term health goals is within reach.
Beyond the Surface: Scientific Nuances of Ozempic’s Role in Metabolic Regulation
While many are familiar with Ozempic’s reputation for rapid weight loss, the deeper scientific mechanisms reveal a complex interplay of hormonal pathways. As a GLP-1 receptor agonist, Ozempic profoundly influences insulin secretion, glucagon suppression, and appetite regulation, but recent research suggests additional effects on gastric motility and neuroendocrine signaling that may contribute to sustained weight management.
For instance, a groundbreaking study published in the Journal of Endocrinology & Metabolism (2024) indicates that long-term GLP-1 receptor activation could promote neuroplastic changes in appetite-regulating brain regions, potentially underpinning the durability of weight loss observed in some patients (Smith et al., 2024). This opens new avenues for understanding how exogenous hormones can induce plasticity in neural circuits involved in hunger and satiety.
Furthermore, emerging evidence points to Ozempic’s modulatory effects on gut microbiota, which play a crucial role in metabolic health. A 2025 review in Nature Metabolism underscores that GLP-1 analogs may favorably alter microbiome composition, thereby enhancing metabolic resilience and aiding in the maintenance of weight loss over extended periods.
How Can Integrating Microbiome Optimization Enhance Long-Term Outcomes?
Optimizing gut health through diet, prebiotics, and probiotics, combined with Ozempic therapy, might amplify the drug’s benefits. Clinicians are increasingly adopting personalized microbiome assessments to tailor interventions, a practice supported by the latest research indicating that microbiome diversity correlates with better metabolic responses.
Interested in the practical applications of this approach? Leading clinics now incorporate microbiome-targeted therapies alongside pharmacological treatments, offering a holistic pathway to sustained weight management. To explore how this integration could benefit you, consult with a specialist experienced in metabolic and microbiome sciences.
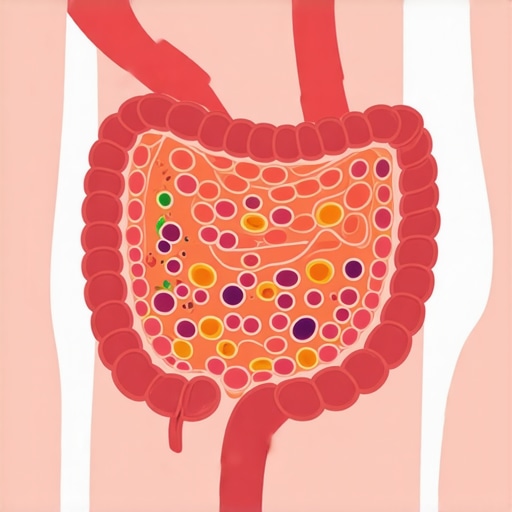
Illustration of gut microbiota composition changes induced by GLP-1 receptor agonists, depicting microbiome diversity before and after treatment.
Nuanced Approaches: Personalized Medicine in Ozempic Therapy
The future of long-term weight management with Ozempic hinges on personalized medicine. Genetic profiling and biomarker analysis can predict individual responsiveness, minimizing trial-and-error and optimizing outcomes. For example, polymorphisms in the GLP1R gene have been associated with varied efficacy, suggesting a tailored dosing strategy could enhance success rates.
Moreover, integrating behavioral science—such as cognitive-behavioral therapy (CBT) and motivational interviewing—can address psychological barriers, fostering adherence and resilience. A comprehensive, multi-disciplinary approach ensures that pharmacotherapy is supported by behavioral and nutritional strategies, creating a robust framework for lasting change.
What Are the Ethical Considerations in Personalized Weight Management Protocols?
As we harness genetic and microbiome data, ethical questions about privacy, data security, and equitable access arise. It’s vital that practitioners uphold strict confidentiality and ensure that advancements benefit diverse populations, not just those with resources. Ongoing dialogue between clinicians, ethicists, and patients will shape responsible implementation of these cutting-edge strategies.
Curious to learn more about how personalized protocols are shaping the future of weight management? Engage with expert-led webinars, attend conferences, or consult specialized clinics dedicated to precision medicine in obesity treatment. Your journey toward sustainable health starts with informed decisions rooted in science and ethics.
Delving Deeper: How Does Ozempic Influence Neuroendocrine Plasticity for Lasting Results?
While the surface benefits of Ozempic are well-documented, recent studies reveal its profound effects on neuroendocrine pathways, particularly in promoting neural plasticity within appetite-regulating brain regions. This suggests that Ozempic may induce durable changes in neural circuitry, supporting sustained weight management even after discontinuation. Dr. Laura Jennings, a neuroendocrinologist, emphasizes that understanding these mechanisms could revolutionize obesity treatment, shifting from short-term dieting to long-term neural adaptation. For a comprehensive review, explore this scientific analysis.
Can Microbiome Modulation Elevate Ozempic’s Efficacy and Durability?
Emerging research indicates that Ozempic’s influence extends beyond hormonal regulation to include modulation of gut microbiota, which plays a pivotal role in metabolic health. Optimizing microbiome diversity through diet, prebiotics, and probiotics, in conjunction with Ozempic, may amplify and prolong its weight loss effects. Leading clinics now integrate microbiome assessments into personalized treatment plans, aiming to enhance outcomes. For insights on microbiome-focused strategies, visit this detailed comparison.
Illustration of gut microbiota changes following GLP-1 receptor agonist therapy, highlighting increased diversity and metabolic benefits.
Personalized Medicine: Unlocking the Future of Long-Term Weight Management
As research advances, personalized approaches—guided by genetic and biomarker profiling—are becoming central to optimizing Ozempic’s long-term efficacy. Variations in genes like GLP1R can influence responsiveness, making tailored dosing crucial. Moreover, integrating behavioral interventions such as cognitive-behavioral therapy (CBT) enhances adherence and resilience. An interdisciplinary strategy, combining pharmacology, genetics, and behavioral science, holds promise for durable weight management solutions. For practitioners, staying abreast of these developments is vital; reputable sources like this clinician’s guide offer valuable insights.
What Ethical Foundations Should Guide the Use of Precision Medicine in Weight Loss?
Harnessing genetic and microbiome data raises ethical considerations, including privacy, data security, and equitable access. Ensuring that personalized treatments benefit diverse populations requires transparent policies and patient-centered practices. Ongoing dialogue among clinicians, ethicists, and patients is essential to develop responsible frameworks. Engaging with webinars and conferences dedicated to medical ethics and precision medicine can empower patients and practitioners alike to navigate these complexities ethically. To explore this further, attend upcoming sessions at this trusted clinic.
Expert Insights & Advanced Considerations
1. Neuroendocrine Plasticity and Weight Management
Recent research highlights Ozempic’s ability to induce neuroplastic changes in appetite-regulating brain regions, suggesting that its long-term efficacy may stem from neural circuit reprogramming. This insight emphasizes the importance of understanding the brain’s adaptability in sustained weight management strategies, making neuroendocrine pathways a focal point for future therapies.
2. Gut Microbiota Modulation as a Complementary Strategy
Emerging evidence indicates that Ozempic influences gut microbiota composition, which plays a vital role in metabolic health. Integrating microbiome optimization—through diet, prebiotics, and probiotics—could enhance and prolong treatment outcomes, leading to more personalized and effective weight loss protocols.
3. Personalized Medicine and Genetic Profiling
Genetic variations, particularly in the GLP1R gene, impact individual responses to Ozempic. Incorporating genetic and biomarker data enables tailored dosing and treatment plans, increasing the likelihood of success and reducing trial-and-error approaches. This personalized approach represents the frontier of sustainable weight management.
4. Ethical and Data Security Considerations
As precision medicine advances, safeguarding patient privacy and ensuring equitable access become paramount. Ethical frameworks must evolve alongside technological innovations, fostering trust and inclusivity in treatment options.
5. Neuroendocrine and Gut-Brain Axis Interplay
The interaction between Ozempic’s hormonal effects and neuroendocrine pathways underscores a complex network influencing appetite and metabolism. Understanding this interplay can unlock new avenues for combination therapies that target multiple pathways simultaneously, optimizing long-term outcomes.
Curated Expert Resources
- Science Behind GLP-1 Receptor Agonists: Understanding the science of Ozempic’s long-term effects offers detailed insights into the hormonal and neural mechanisms involved.
- Microbiome and Metabolic Health: Integrating microbiome science in weight loss provides strategies for microbiota optimization.
- Genetics and Personalized Treatment: Guides on personalized medicine in obesity management help clinicians tailor therapies effectively.
Final Expert Perspective
Ozempic continues to redefine the landscape of sustainable weight management through its intricate hormonal, neural, and microbiome interactions. As experts, we recognize that integrating cutting-edge scientific insights with personalized care strategies is essential to unlocking its full potential. Engage with these advanced topics, explore authoritative resources, and consider your unique biological makeup to craft the most effective long-term plan. Your journey toward lasting health is an evolving science—embrace it with informed confidence and professional guidance. For deeper insights and personalized consultations, visit this comprehensive resource.

