Transformative Power of Ozempic: Real Stories Behind the Before and After
In 2024, the weight loss landscape has been notably shaped by Ozempic, a GLP-1 receptor agonist originally designed for diabetes management but now celebrated for its remarkable impact on body weight reduction. Beyond the clinical data and scientific jargon, the most compelling evidence lies in the vivid before and after weight loss journeys shared by real patients. These stories reveal more than just pounds lost; they illuminate renewed confidence, improved health markers, and lifestyle transformations that inspire many to consider this innovative therapy.
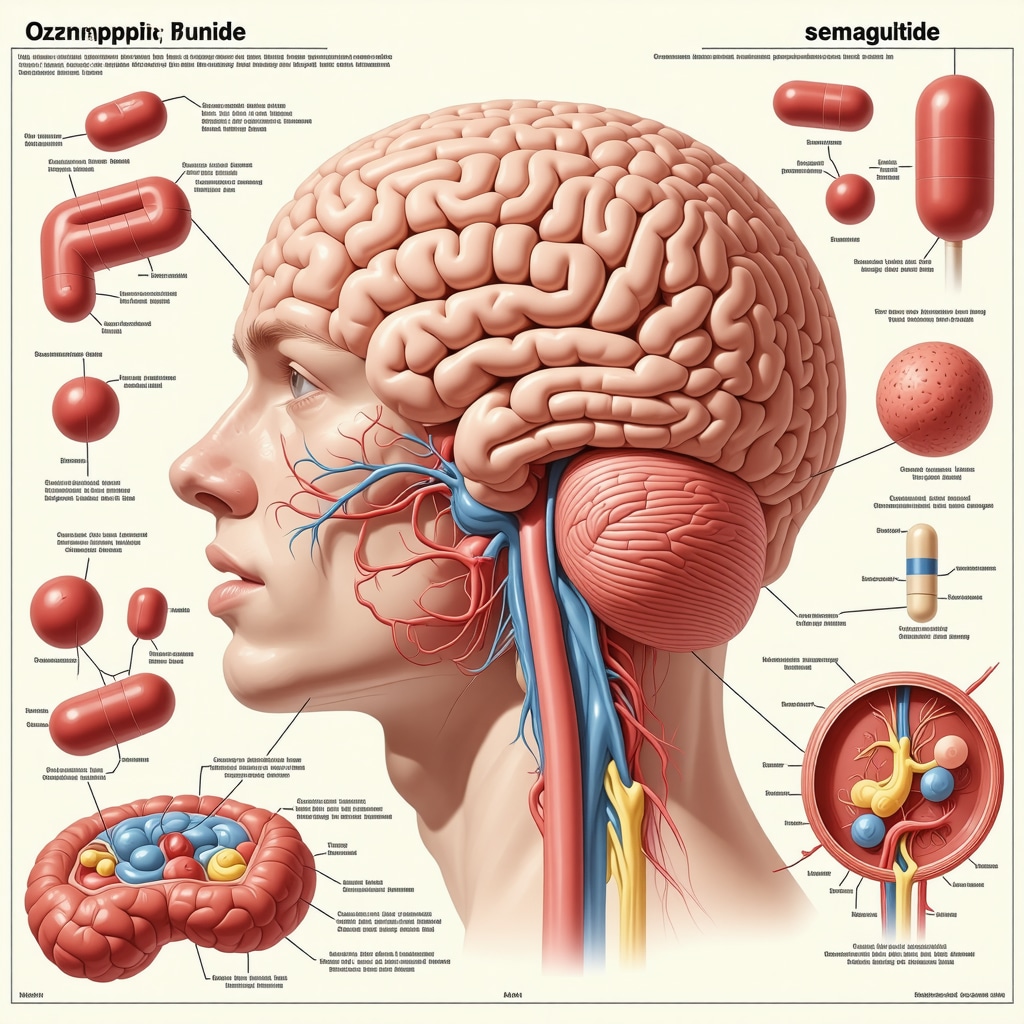
Unpacking the Science Behind Ozempic’s Weight Loss Magic
Ozempic, containing semaglutide, mimics the glucagon-like peptide-1 hormone, which regulates appetite and insulin secretion. This mechanism not only controls blood sugar levels but also significantly reduces hunger and promotes satiety, leading to decreased caloric intake. Studies published in top-tier journals like The New England Journal of Medicine demonstrate that patients using Ozempic can achieve substantial weight loss, often surpassing traditional methods. This scientific foundation explains why many who embark on this path witness stunning transformations within months.
Stunning Ozempic Before and After Results: What Do They Reveal?
The before and after photos and testimonials of 2024 reveal consistent themes: significant fat reduction, improved metabolic health, and enhanced physical mobility. One patient shared how a 16-week regimen not only dropped 25 pounds but also alleviated joint pain and boosted energy levels. Importantly, these transformations are amplified when Ozempic use is paired with clinician-guided lifestyle adjustments, emphasizing nutrition and exercise. Such tailored programs, like those featured in effective Ozempic weight loss programs, maximize outcomes safely and sustainably.
How Can Patients Maximize Their Ozempic Weight Loss Journey?
Maximizing Ozempic’s benefits involves more than just medication adherence. Expert guidance recommends integrating a balanced diet, regular physical activity, and ongoing medical supervision to optimize results and minimize side effects. Understanding the nuances of dosage adjustments and recognizing early signs of adverse reactions are critical. For those curious about safe approaches, detailed insights can be found in physician-prescribed guidelines such as optimal dosing strategies. This holistic approach ensures that the stunning before and after transformations are not only achievable but also maintainable over time.
Embracing a New Chapter: The Emotional and Physical Rewards of Ozempic
Beyond numbers on a scale, the Ozempic before and after journeys of 2024 underscore profound emotional benefits. Patients often report heightened self-esteem, improved mental clarity, and a renewed zest for life. These intangible outcomes highlight the therapy’s role as a catalyst for holistic well-being, encouraging healthier habits and long-term lifestyle changes. Engaging with communities sharing these success stories can provide motivation and support during the weight loss process.
Curious to see more inspiring transformations and learn how expert-supervised Ozempic treatments can help you? Explore real patient transformations and discover how tailored programs can unlock your potential.
Lessons Learned: What My Ozempic Journey Taught Me About Patience and Persistence
Reflecting on my own experience with Ozempic, I realized early on that patience truly is a virtue when it comes to weight loss. Initially, I was eager to see dramatic changes overnight, but the reality was more nuanced. The gradual progress, week by week, was a gentle reminder that sustainable results come from consistency rather than quick fixes. This mindset shift helped me stay motivated even when the scale didn’t move as rapidly as I hoped.
For anyone embarking on this path, remember that Ozempic isn’t a magic wand but a powerful ally when combined with lifestyle changes. The support of a knowledgeable healthcare provider can make all the difference. I found that regular check-ins helped me adjust my dosage safely and tailor my diet and exercise regime to suit my evolving needs.
Integrating Ozempic with Lifestyle Habits: More Than Just Medication
One of the most valuable insights from my journey has been the importance of pairing Ozempic with mindful eating and physical activity. I started tracking my meals and noticed how the appetite-suppressing effects of the medication naturally nudged me towards healthier choices. This wasn’t about deprivation but about savoring nutritious foods that fueled my body.
Incorporating moderate exercise, even just daily walks, amplified my results and improved my mood. It’s a reminder that successful weight loss is holistic, involving both body and mind. For those curious about combining Ozempic with fitness plans, resources like prescription weight loss options combining Ozempic with exercise offer great guidance on making this integration seamless and effective.
What Are the Common Challenges People Face with Ozempic, and How Can They Be Overcome?
Many people, including myself, experience side effects such as nausea or mild digestive discomfort during the initial weeks. It can be discouraging, but understanding that these symptoms often subside with time made a huge difference. Staying hydrated, eating smaller meals, and communicating openly with my healthcare provider helped me manage these hurdles effectively.
Moreover, the emotional rollercoaster of weight loss—moments of self-doubt, plateaus, or comparing progress with others—can be tough. Joining support groups or online communities where people share their real patient transformations helped me feel less isolated and more empowered.
The Role of Medical Supervision: Why It’s Essential for Safe and Effective Use
From my experience and research, including insights from trusted sources like the Mayo Clinic, medical supervision is critical when using Ozempic for weight loss. Doctors can monitor your health markers and adjust your treatment plan to maximize benefits while minimizing risks. This personalized care ensures that your weight loss journey is not only successful but safe.
For anyone considering Ozempic, exploring doctor-supervised Ozempic treatments can provide clarity on what to expect and how to prepare. It’s reassuring to know that expert guidance is readily available, empowering you to make informed decisions about your health.
I’d love to hear your stories and questions about Ozempic and weight loss. Have you tried it, or are you considering it? Share your experiences or concerns in the comments below, and let’s support each other on this transformative journey!
Decoding the Complex Pharmacodynamics of Ozempic for Sustained Weight Loss
Ozempic’s efficacy extends beyond its initial appetite suppression; its intricate pharmacodynamics play a pivotal role in long-term metabolic modulation. Semaglutide exerts sustained effects on the central nervous system’s hypothalamic pathways, orchestrating hunger cues and energy expenditure regulation. Furthermore, emerging research suggests that Ozempic influences gastrointestinal motility and gastric emptying rates, contributing to prolonged satiety signals. This multifaceted action underscores why patients often experience not only significant weight reduction but also improvements in insulin sensitivity and lipid profiles over extended periods.
How Does Ozempic’s Mechanism Interact with Individual Metabolic Variability to Affect Weight Loss Outcomes?
Individual metabolic variability poses one of the thorniest challenges in predicting Ozempic’s weight loss trajectory. Genetic polymorphisms affecting GLP-1 receptor expression, differences in gut microbiota, and baseline insulin resistance levels all modulate therapeutic response. For instance, patients with higher baseline insulin resistance may observe more pronounced glycemic improvements, indirectly facilitating weight loss. Conversely, those with altered receptor sensitivity might require tailored dosing regimens. Recognizing these nuances is essential for clinicians aiming to customize treatment plans, a concept supported by detailed pharmacogenomic analyses in recent peer-reviewed studies.
Strategic Management of Ozempic-Induced Side Effects: Beyond the Basics
While nausea and gastrointestinal discomfort are the most commonly reported adverse effects during Ozempic initiation, advanced management strategies can significantly enhance patient adherence. Gradual dose escalation protocols, as advised by endocrinology experts, mitigate symptom severity. Additionally, adjunct therapies such as prokinetic agents or targeted dietary adjustments—focusing on low-fat, low-fiber meals—have shown promise in clinical settings. Psychological support addressing anticipatory nausea and incorporating behavioral therapy techniques can further optimize tolerability, emphasizing the importance of a multidisciplinary approach.
Integrating Ozempic in Complex Clinical Scenarios: Addressing Comorbidities and Polypharmacy
Patients with obesity frequently present with multifaceted comorbid conditions, including cardiovascular disease, hypertension, and depression, necessitating careful Ozempic integration. The drug’s cardiovascular benefits, evidenced by reductions in major adverse cardiac events in diabetes cohorts, make it particularly advantageous for high-risk patients. However, clinicians must vigilantly monitor for potential pharmacodynamic interactions, especially when concomitant medications such as beta-blockers or antidepressants are prescribed. Tailored monitoring protocols and interprofessional collaboration are paramount to ensure safety and efficacy.
For readers interested in a deeper dive into these complex interactions and tailored management strategies, the American Heart Association’s comprehensive review on GLP-1 receptor agonists offers invaluable expert perspectives.
Can Ozempic’s Weight Loss Effects Be Sustained Long-Term Without Continuous Medication?
A pivotal question in the obesity treatment landscape is whether Ozempic-induced weight loss can be maintained post-therapy cessation. Current evidence suggests that discontinuation often leads to partial weight regain, underscoring the drug’s role as a long-term adjunct rather than a standalone cure. Sustainable success hinges on ingraining lifestyle modifications during treatment—nutritional education, physical activity optimization, and psychological resilience training. Ongoing clinical trials are investigating maintenance strategies, including dose tapering and combination therapies, to extend benefits while minimizing dependency.
Personalizing Ozempic Treatment: The Frontier of Precision Medicine in Weight Management
As the role of Ozempic in weight loss continues to expand, the future lies in tailoring therapy to individual metabolic profiles. Precision medicine approaches leverage genetic, epigenetic, and metabolic biomarkers to predict responsiveness and optimize dosing schedules. This paradigm shift moves beyond one-size-fits-all, enabling clinicians to harness pharmacogenomic data and patient-specific factors to maximize efficacy while minimizing adverse effects. Such customization is increasingly supported by emerging clinical tools and real-world evidence, promising a new era of personalized obesity management.
Innovations in Combination Therapies: Synergizing Ozempic with Emerging Weight Loss Agents
Recent pharmacological advances have opened avenues for combining Ozempic with novel agents targeting complementary pathways involved in energy balance and appetite regulation. For example, dual agonists acting on GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptors show potential for enhanced weight reduction beyond monotherapy. These combinations, under rigorous clinical investigation, aim to amplify metabolic benefits while addressing limitations of single-agent use, such as tolerance development or plateauing effects. Integrating Ozempic into such multifaceted regimens may redefine therapeutic outcomes in complex obesity cases.
What Are the Emerging Strategies for Maintaining Ozempic-Induced Weight Loss After Discontinuation?
Addressing the challenge of weight regain post-Ozempic cessation, experts are exploring multifactorial maintenance strategies. These include gradual dose tapering to mitigate rebound appetite, incorporation of cognitive-behavioral therapy to reinforce behavioral change, and sustained nutritional counseling emphasizing macronutrient quality and meal timing. Additionally, adjunctive use of other pharmacotherapies with distinct mechanisms is being evaluated to support weight stabilization. Longitudinal studies underscore that embedding these strategies within comprehensive lifestyle modification programs is critical for durable success.
Leveraging Digital Health Platforms for Enhanced Ozempic Treatment Adherence
Digital therapeutics and telemedicine are revolutionizing how patients engage with Ozempic-based regimens. Interactive apps offering real-time tracking of medication adherence, side effect monitoring, and personalized coaching foster higher compliance and early identification of complications. Integration of artificial intelligence algorithms further enables predictive analytics to tailor interventions dynamically. This convergence of technology and pharmacotherapy not only enhances patient empowerment but also facilitates data-driven decision-making by healthcare providers, ultimately improving clinical outcomes.
For clinicians and patients eager to delve deeper into the nuances of Ozempic’s long-term management and personalized protocols, resources from the National Center for Biotechnology Information provide comprehensive, peer-reviewed insights.
Embrace these advanced perspectives and share your experiences or questions about optimizing Ozempic therapy in the comments below. Let’s deepen the dialogue on achieving sustainable, personalized weight loss outcomes together.
Frequently Asked Questions (FAQ)
What is Ozempic, and how does it aid weight loss beyond diabetes management?
Ozempic is a medication containing semaglutide, a GLP-1 receptor agonist initially approved for type 2 diabetes treatment. It assists weight loss by mimicking the GLP-1 hormone, which reduces appetite, slows gastric emptying, and enhances satiety, leading to decreased calorie intake. Its metabolic effects also improve insulin sensitivity, which supports sustainable fat reduction.
How quickly can I expect to see noticeable weight loss results with Ozempic?
Weight loss trajectories vary, but many patients begin to see measurable changes within 12 to 16 weeks of treatment initiation. Steady, gradual weight reduction is typical, with peak effects often observed several months into therapy, especially when combined with lifestyle modifications.
Are Ozempic’s weight loss effects permanent after stopping the medication?
Evidence indicates that discontinuing Ozempic frequently leads to some degree of weight regain. Therefore, long-term success depends on integrating sustainable lifestyle habits alongside medication, and in some cases, ongoing pharmacotherapy or maintenance strategies may be advised to preserve the benefits.
What are common side effects of Ozempic, and how can they be managed effectively?
Common side effects include nausea, vomiting, and gastrointestinal discomfort, primarily during the initial weeks. Management strategies involve gradual dose escalation, eating smaller low-fat meals, staying hydrated, and consulting healthcare providers for personalized interventions such as prokinetic agents or behavioral therapies.
Can Ozempic be safely used alongside other medications for comorbid conditions?
Yes, but careful medical supervision is essential. Ozempic’s cardiovascular benefits make it suitable for many patients with obesity-related comorbidities, yet clinicians must monitor for drug interactions, especially with beta-blockers or antidepressants, adjusting treatment protocols as needed.
How does individual metabolic variability affect Ozempic’s weight loss outcomes?
Genetic factors, gut microbiota composition, and baseline insulin resistance influence individual responses to Ozempic. Personalized dosing and precision medicine approaches aim to tailor treatment for optimal efficacy, acknowledging that not all patients will experience identical results.
What role do lifestyle changes play alongside Ozempic treatment?
Lifestyle modifications such as balanced nutrition, regular physical activity, and behavioral support are critical complements to Ozempic. These changes enhance medication efficacy, aid in managing side effects, and contribute to long-term maintenance of weight loss.
Are there emerging therapies that can be combined with Ozempic for improved results?
Yes, combination therapies involving dual agonists targeting GLP-1 and GIP receptors are under investigation and show promise for superior weight loss outcomes by addressing multiple metabolic pathways synergistically.
How can digital health platforms improve adherence and outcomes with Ozempic?
Digital tools facilitate real-time medication tracking, side effect monitoring, personalized coaching, and predictive analytics, empowering patients and enabling clinicians to optimize treatment dynamically, thereby improving adherence and clinical success.
Is medical supervision necessary during Ozempic treatment?
Absolutely. Continuous medical oversight ensures appropriate dosing, monitoring of side effects, management of comorbidities, and adjustment of treatment plans to maximize safety and therapeutic benefits.
Trusted External Sources
- The New England Journal of Medicine (NEJM) – Provides rigorous clinical trial data on semaglutide’s efficacy and safety profiles, foundational for understanding Ozempic’s weight loss impact.
- American Heart Association (AHA) – Offers comprehensive reviews on GLP-1 receptor agonists, including cardiovascular benefits and integration in complex clinical scenarios.
- National Center for Biotechnology Information (NCBI) – Hosts peer-reviewed articles detailing pharmacodynamics, pharmacogenomics, and emerging combination therapies related to Ozempic.
- Mayo Clinic – Supplies authoritative clinical guidelines and patient-focused overviews on safe medication use and side effect management.
- PubMed – A repository of biomedical literature instrumental for accessing the latest research on individual metabolic variability and precision medicine approaches in obesity treatment.
Conclusion
Ozempic has emerged as a transformative agent in the 2024 weight loss arena, offering significant benefits rooted in its sophisticated pharmacological action on appetite regulation and metabolism. The compelling before and after patient stories underscore not just physical transformation but also emotional and lifestyle renewal when combined with tailored medical supervision and sustainable habits. Recognizing the complexities of individual metabolic responses and integrating emerging combination therapies and digital health innovations paves the way for personalized, effective obesity management. As research advances, embracing a holistic, multidisciplinary approach remains paramount to maximizing and maintaining Ozempic’s weight loss success. If you found this detailed expert insight valuable, share your experiences, ask questions, or explore related content to deepen your journey toward healthier living.


After reading about the transformative power of Ozempic and its real patient stories, I’m truly impressed by how this medication not only promotes significant weight loss but also positively impacts emotional well-being. The post’s emphasis on integrating Ozempic with lifestyle changes resonates with my experience. I’ve seen people struggle with quick-fix mentalities, but the gradual, steady progress approach detailed here struck a chord. It’s encouraging to hear about the emotional rewards such as improved self-esteem and mental clarity that go hand-in-hand with physical transformation. What stood out most to me was the acknowledgment of individual metabolic variability—something I believe is often overlooked. It makes me wonder how much personalized medicine will reshape how we approach obesity treatment moving forward. Has anyone tried combining Ozempic with fitness regimens or nutrition programs and noticed a particular synergy? I’d be interested in hearing how others manage side effects while maintaining motivation. Also, digital health platforms sound like a promising tool for adherence but I’m curious about their real-world effectiveness. Would love to learn from others’ experiences!