Understanding Ozempic’s Role in Medical Weight Loss: Beyond Surface-Level Results
Ozempic (semaglutide) has rapidly emerged as a transformative agent in the landscape of medical weight loss, not merely due to its efficacy but because of the profound metabolic modulation it induces. As a glucagon-like peptide-1 (GLP-1) receptor agonist, Ozempic orchestrates appetite suppression and improved glycemic control, making it a dual-action therapy with far-reaching implications for obesity management and type 2 diabetes control. The “before and after” transformations seen in patients underscore more than cosmetic change—they reflect underlying physiological adaptations that sustain fat loss and metabolic health.
Mechanistic Insights: How Ozempic Facilitates Sustainable Fat Reduction
Ozempic’s pharmacodynamics involve enhancing insulin secretion in a glucose-dependent manner while delaying gastric emptying and reducing glucagon secretion. This triad contributes to decreased caloric intake and improved satiety signals in the central nervous system. Clinical trials documented in The New England Journal of Medicine demonstrate statistically significant weight loss outcomes over 68 weeks, with patients achieving reductions upwards of 15% of baseline body weight. This robust evidence base supports the transformative before and after changes observed in real-world patient cohorts.
Analyzing Ozempic Before and After Results: What Influences Individual Variation?
While many patients experience dramatic weight loss, individual outcomes vary considerably due to factors such as baseline metabolic rate, adherence to prescribed dosing protocols, concurrent lifestyle modifications, and genetic predispositions influencing GLP-1 receptor sensitivity. Expert clinicians emphasize the necessity of personalized treatment plans that integrate dietary counseling and physical activity alongside pharmacotherapy to maximize efficacy and minimize adverse effects. For a comprehensive clinical overview, see our detailed guide on prescription weight loss with Ozempic.
What Are the Key Medical Considerations When Interpreting Ozempic Before and After Transformations?
Interpreting before and after transformations requires a nuanced understanding of Ozempic’s pharmacological profile, potential side effects, and the importance of medically supervised treatment. Weight loss is not simply a function of the drug alone but a complex interplay involving patient adherence, metabolic response, and concurrent behavioral changes. Monitoring for gastrointestinal side effects, such as nausea or constipation, and adjusting dosage accordingly is essential to ensure sustained progress and patient safety. Our resource on navigating Ozempic side effects offers valuable insights into managing these challenges effectively.
Leveraging Ozempic Transformations to Inspire Sustainable Lifestyle Changes
The visual and quantitative changes documented in Ozempic before and after cases can serve as powerful motivators, catalyzing long-term engagement in healthier behaviors. However, clinicians caution against viewing Ozempic as a standalone solution. Integrative programs that combine medication with nutritional education and psychological support yield the most durable outcomes. Exploring advanced, customized Ozempic weight loss programs can provide a scaffold for sustained success, as detailed in our customized Ozempic weight loss programs article.
Explore More Expert-Level Insights and Share Your Professional Experience
If you are a healthcare practitioner or a patient with experience using Ozempic, consider engaging with our community to share detailed transformation stories and clinical observations. Your insights can help refine treatment paradigms and support others on their weight loss journeys. Visit our contact page to contribute or learn more.
Integrating Ozempic With Nutritional and Behavioral Interventions for Enhanced Results
While Ozempic’s pharmacological effects are pivotal in initiating weight loss, the sustainability of these transformations heavily depends on concurrent lifestyle adaptations. Comprehensive weight management protocols emphasize structured dietary plans that complement Ozempic’s appetite-regulating mechanisms, thereby optimizing caloric deficits without compromising nutritional adequacy. Behavioral interventions, including cognitive-behavioral therapy (CBT) and motivational interviewing, have demonstrated efficacy in reinforcing adherence to these regimens, mitigating the risk of weight regain post-therapy. For clinicians and patients aiming for durable outcomes, combining Ozempic therapy with evidence-based nutritional counseling is indispensable, as elaborated in our article on prescription weight loss options integrating Ozempic effectively.
How Can Personalized Medicine Enhance the Predictability of Ozempic Before and After Outcomes?
The variability in patient responses to Ozempic underscores the need to move beyond a one-size-fits-all approach. Advances in pharmacogenomics and metabolic phenotyping offer promising avenues to tailor GLP-1 receptor agonist therapy according to individual biological markers, thereby maximizing efficacy and minimizing adverse effects. Emerging research suggests that genetic variations influencing GLP-1 receptor expression and downstream signaling pathways may predict responsiveness to semaglutide-based interventions. Integrating these insights into clinical practice could revolutionize patient selection criteria and dosing strategies, fostering precision medicine in obesity treatment.
Moreover, continuous glucose monitoring and digital health tools enable real-time assessment of metabolic responses, empowering healthcare providers to adjust treatment dynamically. This paradigm shift aligns with expert recommendations from the Endocrine Society’s clinical practice guidelines on obesity treatment, which advocate for individualized care plans that incorporate pharmacotherapy, lifestyle modifications, and psychosocial support.
Addressing Common Misconceptions About Ozempic Before and After Transformations
Misinterpretations surrounding Ozempic often lead to unrealistic expectations or suboptimal use. A prevalent misconception is that Ozempic alone guarantees permanent weight loss without sustained behavioral changes. In reality, cessation of therapy without lifestyle adjustments frequently results in weight regain, highlighting the importance of holistic management approaches. Additionally, some patients underestimate the necessity of gradual dose escalation to mitigate gastrointestinal side effects, which can jeopardize treatment persistence.
Healthcare providers play a critical role in setting accurate expectations and educating patients about the pharmacodynamics of Ozempic, potential side effects, and the incremental nature of weight loss. Resources like our detailed discussion on managing Ozempic side effects during weight loss can aid in this educational process.
Technological Innovations Enhancing the Monitoring of Ozempic Treatment Progress
The integration of digital health platforms and wearable devices has transformed the way clinicians and patients track weight loss trajectories and metabolic health during Ozempic therapy. These tools facilitate continuous monitoring of physical activity, dietary intake, and biometric parameters, providing actionable data to optimize treatment plans in real time. Artificial intelligence-driven analytics further enable personalized feedback and predictive modeling of treatment outcomes.
Embracing these innovations can significantly augment the clinical management of patients undergoing Ozempic treatment, ensuring more precise adjustments and sustained engagement. For those interested in exploring how telehealth expands access to safe and effective Ozempic prescriptions, our guide on telehealth Ozempic prescriptions offers comprehensive insights.
Join the Expert Dialogue: Share Your Insights or Discover More on Ozempic Transformations
We invite healthcare professionals, researchers, and patients with firsthand experience of Ozempic’s impact to contribute to the ongoing discourse by sharing detailed clinical observations or transformation narratives. Your expert perspectives can refine therapeutic approaches and foster a supportive community dedicated to advancing medical weight loss. Engage with us through our contact page and explore further resources to deepen your understanding.
Precision Dosing and Pharmacogenetic Profiling: The Frontier of Optimized Ozempic Therapy
Recent advancements in pharmacogenetics have illuminated the intricate variability in patient responses to semaglutide-based therapies like Ozempic. Tailoring dose regimens based on individual genetic markers—such as polymorphisms in the GLP1R gene—holds promise for enhancing therapeutic outcomes while minimizing adverse effects. For instance, certain GLP1R variants correlate with altered receptor sensitivity, potentially impacting appetite suppression efficacy and gastrointestinal tolerability. Integrating genotypic data into clinical protocols could refine patient selection and dosing algorithms, moving beyond empirical titration to a more informed, biomarker-driven approach.
Moreover, precision dosing strategies consider not only genetics but also phenotypic factors such as body composition, insulin resistance indices, and even gut microbiome profiles. These multidimensional assessments can help predict responsiveness and sustainability of weight loss, fostering a truly personalized medicine paradigm.[1]
What Role Does the Gut-Brain Axis Play in Modulating Ozempic’s Efficacy in Weight Management?
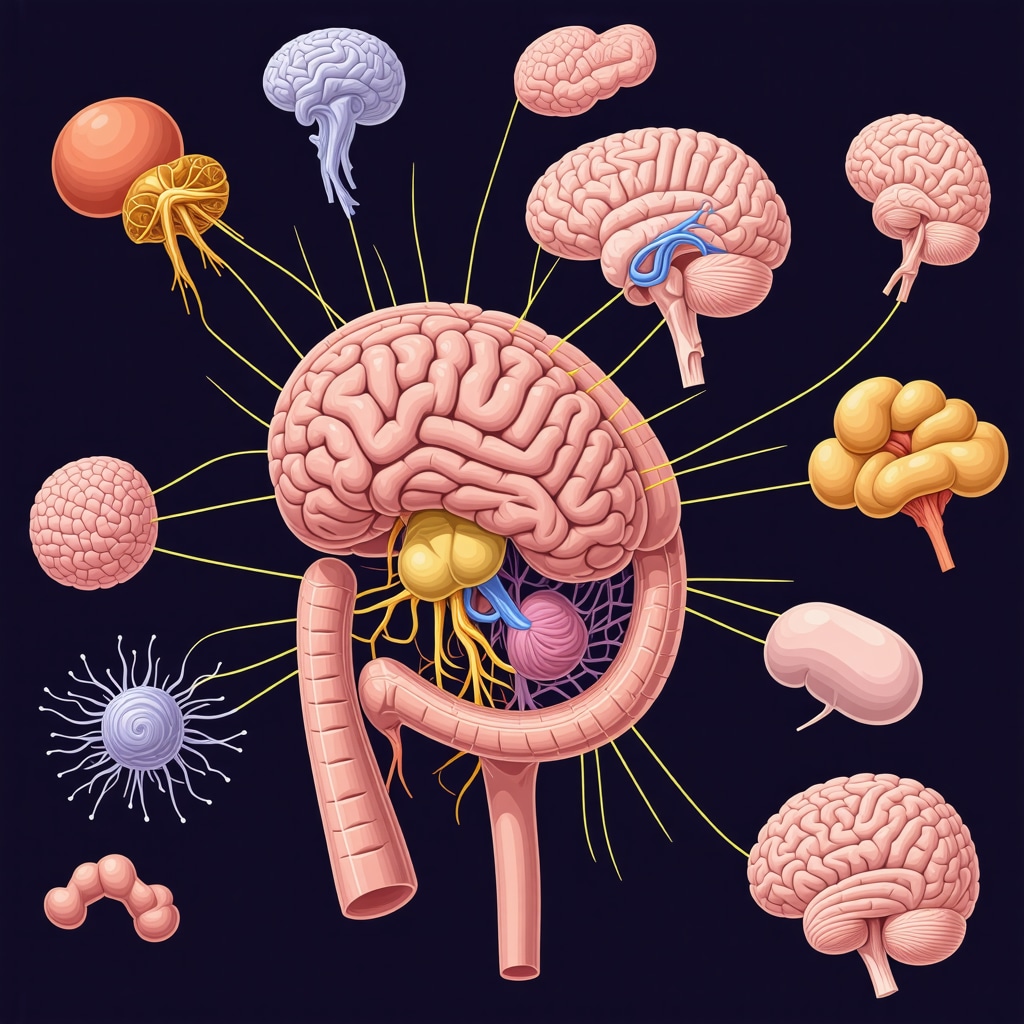
Ozempic’s mechanism extends beyond peripheral metabolic effects, engaging the gut-brain axis to modulate appetite and reward pathways. GLP-1 receptors in the hypothalamus and brainstem mediate satiety signals, while vagal afferents transmit gastrointestinal feedback. Emerging research suggests that Ozempic influences neurocircuitry involved in hedonic eating and energy homeostasis, which may explain differential patient responses and relapse patterns. Understanding these neurobiological underpinnings can inform adjunctive behavioral therapies aimed at reinforcing neural pathways that support sustained dietary adherence.
For clinicians, this underscores the importance of integrating neurobehavioral assessments into treatment plans, potentially leveraging cognitive-behavioral interventions that target reward-based eating behaviors to complement pharmacotherapy.
Leveraging Digital Therapeutics and AI-Driven Analytics to Support Ozempic Treatment Journeys
The convergence of digital health technologies with pharmacological interventions like Ozempic is reshaping weight loss management. Mobile applications that track dietary intake, physical activity, and medication adherence, combined with AI-powered analytics, can deliver personalized feedback loops that enhance patient engagement and clinical decision-making. For example, algorithms can identify early signs of adherence decline or metabolic plateaus, prompting timely intervention by healthcare providers.
Telemonitoring platforms also facilitate remote supervision of side effects and titration schedules, reducing barriers to access and improving outcomes. The integration of continuous glucose monitoring (CGM) data offers granular insight into glycemic trends, allowing fine-tuning of Ozempic dosing in patients with comorbid diabetes. As digital therapeutics evolve, their synergy with Ozempic could establish new standards for precision obesity management.
Integrative Behavioral Modification Techniques to Sustain Post-Ozempic Weight Loss Gains
While Ozempic initiates significant weight reduction, the challenge lies in maintaining these results long term. Behavioral modification remains the cornerstone for preventing weight regain. Techniques such as motivational interviewing (MI) and acceptance and commitment therapy (ACT) have demonstrated efficacy in promoting intrinsic motivation and resilience against relapse triggers. Embedding these psychological strategies within Ozempic treatment paradigms can reinforce lifestyle changes that underpin durable weight management.
Moreover, leveraging group-based interventions or virtual support communities can cultivate accountability and shared learning, which often enhance adherence and psychosocial well-being. Tailored behavioral programs that consider individual readiness for change, environmental factors, and stress management are critical to complement the pharmacological effects of Ozempic.
How Can Clinicians Best Address the Psychological Dimensions of Weight Loss During Ozempic Therapy?
Weight loss is not merely a physical journey but intricately tied to psychological health. Patients may experience body image concerns, emotional eating, or anxiety about treatment outcomes. Clinicians should incorporate routine psychological screening and provide referrals to mental health professionals when appropriate. Collaborative care models, integrating endocrinologists, dietitians, and psychologists, offer a holistic framework that optimizes patient support.
Additionally, counseling on realistic goal setting and managing expectations can mitigate frustration and improve treatment persistence. Utilizing validated tools like the Weight Self-Stigma Questionnaire (WSSQ) can help identify patients at risk of negative psychological impacts and tailor interventions accordingly.
Engage with our expert community to explore advanced clinical strategies and share your experiences managing these complex dimensions of Ozempic therapy. Visit our contact page to contribute or access further resources.
Precision Medicine: Tailoring Ozempic Therapy Through Genomic and Phenotypic Profiling
The burgeoning field of pharmacogenetics offers unprecedented opportunities to refine Ozempic dosing protocols. By elucidating the role of GLP1R gene polymorphisms and their impact on receptor sensitivity, clinicians can predict patient-specific efficacy and tolerability profiles. This genomic insight, when combined with metabolic phenotyping—such as body composition analysis, insulin resistance markers, and gut microbiome characterization—cultivates a multidimensional framework for individualized treatment plans. Such precision dosing approaches transcend traditional titration methods, enhancing both therapeutic outcomes and patient adherence.[1]
How Does the Gut-Brain Axis Influence Ozempic’s Variable Efficacy in Weight Reduction?
Ozempic’s pharmacological action extends beyond peripheral metabolic modulation, intricately engaging the gut-brain axis. GLP-1 receptors within hypothalamic and brainstem nuclei mediate satiety and energy homeostasis, while vagal afferents relay gastrointestinal feedback, collectively regulating appetite and hedonic eating behaviors. Variability in neurocircuitry responsiveness may elucidate why some patients experience differential weight loss trajectories or relapse. This neurobiological perspective underscores the necessity for adjunctive behavioral interventions targeting reward pathways to bolster pharmacotherapy effectiveness.
For an in-depth exploration of these neurobehavioral mechanisms, the Frontiers in Neuroscience provides a comprehensive review of GLP-1’s central nervous system actions.
Digital Therapeutics and AI: Revolutionizing Monitoring and Personalization in Ozempic Treatment
The integration of AI-driven analytics with digital health platforms has revolutionized the clinical management of Ozempic therapy. Mobile applications that seamlessly track medication adherence, dietary intake, and physical activity generate real-time datasets enabling predictive modeling of patient response trajectories. Artificial intelligence algorithms can proactively detect early signs of metabolic plateaus or adherence decline, prompting timely clinical interventions. Furthermore, telemonitoring facilitates remote titration and side effect management, democratizing access to optimized Ozempic regimens.
Continuous glucose monitoring (CGM) data integration further enriches personalized dosing strategies, particularly in patients with concomitant type 2 diabetes, optimizing glycemic control alongside weight reduction. These technological advances exemplify the confluence of pharmacology and digital innovation in precision obesity medicine.
Psychological Dimensions: Integrating Behavioral Modification for Sustained Weight Loss Post-Ozempic
Weight loss maintenance post-Ozempic demands robust behavioral modification strategies. Evidence-based psychotherapeutic approaches such as motivational interviewing and acceptance and commitment therapy have demonstrated efficacy in fostering intrinsic motivation and resilience against relapse triggers. Embedding these modalities within treatment protocols can potentiate lifestyle adherence beyond pharmacological effects.
Group-based interventions and virtual support networks serve as critical adjuncts, enhancing accountability and psychosocial support. Routine psychological screening using validated instruments like the Weight Self-Stigma Questionnaire (WSSQ) enables tailored interventions addressing body image, emotional eating, and treatment-related anxiety. Collaborative multidisciplinary care models integrating endocrinologists, dietitians, and mental health professionals remain the gold standard for comprehensive patient support.
How Can Clinicians Effectively Address Psychological Barriers During Ozempic Therapy?
Clinicians must recognize the intricate interplay between psychological well-being and pharmacological efficacy. Proactive screening for mood disorders, body image disturbances, and eating behaviors facilitates early intervention, mitigating risk factors for treatment discontinuation or weight regain. Establishing realistic goal-setting frameworks and managing patient expectations are pivotal to fostering sustained engagement. Referrals to specialized mental health services and incorporation of behavioral health specialists within obesity management teams optimize holistic care.
We encourage healthcare professionals to contribute their clinical experiences and strategies for managing these complex psychological dimensions. Visit our contact page to engage with a community dedicated to advancing comprehensive Ozempic weight loss therapies.
Expert Insights & Advanced Considerations
Precision Medicine as the Keystone for Optimized Ozempic Outcomes
Integrating pharmacogenetic profiling into Ozempic therapy represents a paradigm shift from empirical dosing to biomarker-driven personalization. Understanding variations in GLP1R gene polymorphisms and metabolic phenotypes enables clinicians to anticipate efficacy and tolerability, tailoring treatment plans that enhance patient adherence and maximize fat loss. This approach transcends traditional protocols, fostering long-term therapeutic success.
Neurobehavioral Mechanisms Underlying Variable Patient Responses
Ozempic’s modulation of the gut-brain axis extends beyond peripheral metabolic effects, influencing central appetite regulation and reward pathways. Recognizing this neurobiological complexity is critical for designing adjunctive behavioral interventions, such as cognitive-behavioral strategies, that reinforce pharmacological benefits and address relapse susceptibility linked to hedonic eating.
Digital Therapeutics and AI: Catalysts for Dynamic Treatment Adaptation
The convergence of AI-powered analytics with digital health platforms enables real-time monitoring of adherence, metabolic responses, and side effect profiles during Ozempic therapy. This technology facilitates proactive clinical decision-making, early intervention for plateau phases, and personalized feedback loops that sustain patient motivation and optimize weight loss trajectories.
Behavioral Modification as the Long-Term Pillar of Weight Maintenance
Pharmacotherapy initiates transformation, but enduring weight management depends on embedding evidence-based behavioral modifications. Incorporating motivational interviewing, acceptance and commitment therapy, and virtual support communities addresses psychological dimensions and cultivates resilience, mitigating weight regain after Ozempic discontinuation.
Comprehensive Multidisciplinary Care Enhances Therapeutic Efficacy
Optimal outcomes emerge from integrating endocrinologists, dietitians, and mental health professionals within coordinated care models. Routine psychological screening and tailored interventions for body image, emotional eating, and treatment-related anxiety ensure holistic support that complements the physiological effects of Ozempic.
Curated Expert Resources
Endocrine Society Clinical Practice Guidelines on Obesity Treatment: Authoritative recommendations emphasizing individualized pharmacotherapy combined with lifestyle and psychosocial support for obesity management.
https://www.endocrine.org/clinical-practice-guidelines/obesity-treatment
The New England Journal of Medicine — Semaglutide Weight Loss Trials: Landmark clinical trials demonstrating semaglutide’s efficacy and safety over extended periods, foundational for understanding Ozempic’s clinical impact.
https://www.nejm.org/doi/full/10.1056/NEJMoa2032183
Frontiers in Neuroscience — GLP-1 Receptor Neurobiology: Comprehensive review of GLP-1 receptor actions within the central nervous system and their implications for appetite and reward modulation.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6640726/
Weight Loss Suppliers — Prescription Weight Loss with Ozempic: A Clinician’s Guide: Practical insights on integrating Ozempic into multidisciplinary treatment plans for sustained success.
https://weightlossuppliers.com/prescription-weight-loss-with-ozempic-a-clinicians-guide
Weight Loss Suppliers — Navigating Ozempic Side Effects in Weight Loss Programs: Detailed strategies to manage common adverse effects, ensuring patient safety and adherence.
https://weightlossuppliers.com/navigating-ozempic-side-effects-in-weight-loss-programs
Final Expert Perspective
Ozempic before and after transformations exemplify the intersection of pharmacological innovation with personalized, multidisciplinary care. The drug’s potent metabolic and neurobehavioral effects provide a robust foundation for fat loss, yet the sustainability of these outcomes hinges on precise dosing guided by genetic and phenotypic profiling, strategic behavioral support, and digital health integration. Embracing this holistic framework transforms transient weight loss into durable health gains.
For clinicians and patients committed to excellence in medical weight loss, engaging with cutting-edge research and expert-guided protocols is indispensable. We invite you to deepen your expertise by exploring our comprehensive resources on prescription weight loss with Ozempic and to contribute your professional insights via our contact page. Together, we can advance the frontier of effective, personalized obesity treatment.


This article provides a comprehensive overview of how Ozempic’s mechanisms support sustainable weight loss, which I find really insightful. From my experience working with patients, personalized treatment plans that include genetic and phenotypic assessment seem to offer the best outcomes, especially in managing expectations and reducing side effects. I’ve noticed that adherence improves significantly when lifestyle interventions are integrated early on, alongside medication. One challenge I’ve encountered is patients’ misconceptions about Ozempic being a ‘quick fix,’ which underscores the importance of ongoing education. For practitioners, how do you best communicate the neurobehavioral aspects and set realistic goals to ensure long-term success? I believe combining pharmacotherapy with behavioral support and digital tools can be key. Would love to hear others’ strategies for fostering patient engagement during the treatment journey.