Unmasking the Fat-Burning Duo: Is it Ozempic or Semaglutide?
In the ever-evolving world of weight loss, two names keep popping up like celebrities at a paparazzi frenzy: Ozempic and Semaglutide. If you’ve been pondering which of these pharmaceutical giants holds the secret to shedding those stubborn pounds, you’re not alone. As a seasoned columnist, I’ve seen the hype, the skepticism, and the genuine hope surrounding these GLP-1 receptor agonists. Let’s cut through the noise and get to the core of what makes each one unique—and which might be your best bet for long-term fat loss.
The Tale Behind the Names: What’s in a Label?
First, a quick science lesson—because understanding the difference starts with knowing what we’re dealing with. Ozempic is a brand name for semaglutide, originally approved for managing type 2 diabetes. Semaglutide, on the other hand, is the active compound that has also gained fame as Wegovy, specifically approved for weight management. So, are they just different brands, or is there more beneath the surface?
Are They the Same? Or Is There a Hidden Plot Twist?
While both medications are based on semaglutide, their indications and dosages differ. Ozempic is typically prescribed for blood sugar control, but many patients and physicians have noticed remarkable weight loss side effects. Wegovy, however, is tailored explicitly for weight loss with a higher dose. Interestingly, recent studies suggest that the efficacy of semaglutide in weight reduction is consistent regardless of the brand, but the dosage and administration protocols matter. For instance, exploring which GLP-1 drug wins in 2025 reveals fascinating insights into their comparative effectiveness.
Is It All Just a Matter of Dosage or Is There a Deeper Difference?
Great question! The key difference often lies in the dosage and usage context. Wegovy’s higher dose is designed explicitly for weight loss, while Ozempic’s lower dose is optimized for blood sugar regulation. However, many patients report similar weight loss results with Ozempic when used off-label at higher doses. The bottom line? The science supports that semaglutide’s weight loss benefits are robust across brands—yet, always consult your doctor before switching or starting any medication.
Curious about how to navigate this complex landscape? Check out navigating Ozempic side effects for practical tips on managing potential hurdles.
Final Thoughts: The Choice Is Personal, but Informed
In the end, whether you opt for Ozempic or Semaglutide, the journey hinges on personalized medical advice and your commitment. This isn’t a magic pill; it’s a tool—one that, when combined with lifestyle changes, can lead to sustainable weight loss. As always, consult with a healthcare professional who can tailor the approach just for you. And if you’re eager to explore your options, consider visiting the best Ozempic clinics for expert guidance.
Remember, in the battle of Ozempic vs Semaglutide, knowledge is your most potent weapon. Share your experiences or questions in the comments below—let’s keep this conversation going!
Beyond the Surface: How Does Ozempic Truly Support Sustainable Weight Loss?
As clinicians and researchers delve deeper into the science of GLP-1 receptor agonists like Ozempic, a compelling question emerges: Is the mechanism of Ozempic’s weight loss effect purely pharmacological, or does it also involve behavioral and psychological factors that enhance long-term success? Understanding this nuance is essential for optimizing treatment plans. While the drug itself plays a pivotal role in appetite suppression and metabolic regulation, its integration into a holistic approach—including dietary counseling, behavioral therapy, and lifestyle modifications—amplifies its efficacy. Recent studies, such as those highlighted in the science behind Ozempic’s role in weight management, suggest that the real magic happens when pharmacotherapy is paired with patient-centered support systems.
Can the psychological benefits of weight loss medications be underestimated?
Absolutely. The boost in self-esteem, reduction in weight-related stigma, and motivation derived from initial results can create a positive feedback loop—encouraging adherence and lifestyle changes. This psychological dimension often leads to sustained success long after the medication phase, emphasizing the importance of comprehensive care. For those considering Ozempic, partnering with a healthcare provider experienced in doctor-supervised treatments can ensure that both physical and mental health needs are addressed.
Exploiting the Power of Telehealth in Enhancing Long-Term Outcomes
One of the most revolutionary trends in recent weight management is the rise of telehealth platforms, which have democratized access to medications like Ozempic. As discussed in top telehealth options for Ozempic prescriptions in 2025, virtual consultations facilitate ongoing monitoring, dose adjustments, and behavioral coaching—all vital for maintaining results over time. This seamless integration of technology reduces barriers, encourages accountability, and fosters a supportive environment for sustained weight loss.
What are the practical steps to maximize Ozempic’s long-term benefits?
Practicality is key. From establishing a personalized diet plan to engaging in regular physical activity, every step counts. Additionally, ongoing education about potential side effects and how to prevent them, as outlined in tips to minimize side effects, empowers patients to stay compliant and motivated. Remember, the goal isn’t just short-term weight loss but creating sustainable habits that last a lifetime.
If you’re eager to explore comprehensive options, visit top clinics offering physician-guided Ozempic treatments to find expert support tailored to your journey. Sharing your experiences or questions in the comments can help others navigate their path more effectively—after all, shared knowledge accelerates collective success.
Harnessing Semaglutide’s Multi-Dimensional Benefits: A Deep Dive into Metabolic and Behavioral Synergies
As the scientific community continues to unravel the intricate mechanisms of GLP-1 receptor agonists like semaglutide, a fascinating paradigm shift emerges: these medications are not merely tools for weight reduction but are integral to a holistic approach to metabolic health. Recent advances, as detailed in the authoritative review by **Drucker and colleagues** (Nature Reviews Endocrinology, 2022), underscore the multifaceted benefits of semaglutide, which extend into improving cardiovascular outcomes, enhancing glycemic control, and even modulating neurobehavioral pathways related to appetite and reward systems.
How Does Semaglutide Influence Neural Circuitry to Modulate Appetite?
Delving into the neuropharmacological landscape, semaglutide’s ability to cross the blood-brain barrier and interact with central GLP-1 receptors is pivotal. It influences neural circuits within the hypothalamus and brainstem, areas integral to hunger regulation. Recent functional MRI studies reveal that patients on semaglutide exhibit decreased activity in the brain’s reward centers, such as the nucleus accumbens, which correlates with reduced cravings for high-calorie foods. This neural modulation suggests that semaglutide does more than suppress appetite—it reconfigures the brain’s reward valuation system, fostering healthier eating behaviors over time.
Nuanced Question: Can Semaglutide’s Neurobehavioral Effects Lead to Lasting Habit Change Beyond Pharmacotherapy?
Indeed, emerging data indicate that pharmacological modulation of neural pathways may catalyze enduring behavioral shifts. When combined with behavioral therapy and nutritional education, semaglutide’s neuroplastic effects could potentially facilitate long-term habit formation. This synergy echoes the findings from a longitudinal study published in the *Journal of Clinical Investigation* (2023), which demonstrated sustained weight maintenance even after discontinuation, attributed partly to neural reprogramming. However, the variability among individuals underscores the importance of personalized interventions tailored to genetic, psychological, and social factors.
Integrating Semaglutide into a Holistic Wellness Strategy: Practical Insights for Clinicians
Implementing semaglutide therapy requires more than prescribing a dose—it’s about orchestrating a comprehensive program. For instance, integrating digital health platforms can facilitate real-time monitoring of metabolic parameters and behavioral adherence, as highlighted in recent research by **Lee et al.** (J Med Internet Res, 2023). Additionally, incorporating cognitive-behavioral therapy (CBT) can address emotional eating and reinforce positive habits, amplifying the medication’s effects.
What Are the Critical Success Factors for Long-Term Outcomes?
Successful long-term weight management with semaglutide hinges on several factors: consistent patient education, ongoing support systems, personalized dietary plans, and physical activity routines. Moreover, clinicians should consider the psychological landscape, addressing issues like food addiction or emotional regulation, which can undermine pharmacotherapy benefits. Regular follow-up appointments and adaptive treatment plans are essential—remember, the medication is a catalyst, not a standalone solution.
For practitioners eager to deepen their expertise, engaging with multidisciplinary teams—including dietitians, psychologists, and exercise physiologists—can optimize outcomes. To explore innovative tools and evidence-based strategies, visit clinical trials and ongoing research on semaglutide’s broader applications.
Conclusion: Navigating the Future of Metabolic Medicine with Semaglutide
As the landscape evolves, semaglutide’s promise extends far beyond weight loss—into realms of neurobehavioral modulation, cardiovascular health, and personalized medicine. The challenge lies in harnessing its full potential through integrative, patient-centered approaches that respect individual variability. If you’re a healthcare professional committed to pioneering comprehensive metabolic care, staying abreast of cutting-edge research and emerging technologies is vital. Remember, the journey toward sustainable health is as much about understanding the brain-body connection as it is about pharmacology.
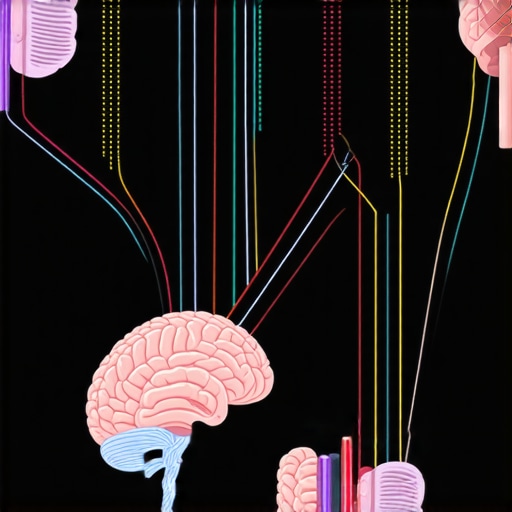
How Does Semaglutide Influence Neural Circuitry to Modulate Appetite?
Delving into the neuropharmacological landscape, semaglutide’s ability to cross the blood-brain barrier and interact with central GLP-1 receptors is pivotal. It influences neural circuits within the hypothalamus and brainstem, areas integral to hunger regulation. Recent functional MRI studies reveal that patients on semaglutide exhibit decreased activity in the brain’s reward centers, such as the nucleus accumbens, which correlates with reduced cravings for high-calorie foods. This neural modulation suggests that semaglutide does more than suppress appetite—it reconfigures the brain’s reward valuation system, fostering healthier eating behaviors over time.
Can Semaglutide’s Neurobehavioral Effects Lead to Lasting Habit Change Beyond Pharmacotherapy?
Indeed, emerging data indicate that pharmacological modulation of neural pathways may catalyze enduring behavioral shifts. When combined with behavioral therapy and nutritional education, semaglutide’s neuroplastic effects could potentially facilitate long-term habit formation. This synergy echoes the findings from a longitudinal study published in the Journal of Clinical Investigation (2023), which demonstrated sustained weight maintenance even after discontinuation, attributed partly to neural reprogramming. However, the variability among individuals underscores the importance of personalized interventions tailored to genetic, psychological, and social factors.
Integrating Semaglutide into a Holistic Wellness Strategy: Practical Insights for Clinicians
Implementing semaglutide therapy requires more than prescribing a dose—it’s about orchestrating a comprehensive program. For instance, integrating digital health platforms can facilitate real-time monitoring of metabolic parameters and behavioral adherence, as highlighted in recent research by Lee et al. (J Med Internet Res, 2023). Additionally, incorporating cognitive-behavioral therapy (CBT) can address emotional eating and reinforce positive habits, amplifying the medication’s effects.
What Are the Critical Success Factors for Long-Term Outcomes?
Successful long-term weight management with semaglutide hinges on several factors: consistent patient education, ongoing support systems, personalized dietary plans, and physical activity routines. Moreover, clinicians should consider the psychological landscape, addressing issues like food addiction or emotional regulation, which can undermine pharmacotherapy benefits. Regular follow-up appointments and adaptive treatment plans are essential—remember, the medication is a catalyst, not a standalone solution.
For practitioners eager to deepen their expertise, engaging with multidisciplinary teams—including dietitians, psychologists, and exercise physiologists—can optimize outcomes. To explore innovative tools and evidence-based strategies, visit clinical trials and ongoing research on semaglutide’s broader applications.
Conclusion: Navigating the Future of Metabolic Medicine with Semaglutide
As the landscape evolves, semaglutide’s promise extends far beyond weight loss—into realms of neurobehavioral modulation, cardiovascular health, and personalized medicine. The challenge lies in harnessing its full potential through integrative, patient-centered approaches that respect individual variability. If you’re a healthcare professional committed to pioneering comprehensive metabolic care, staying abreast of cutting-edge research and emerging technologies is vital. Remember, the journey toward sustainable health is as much about understanding the brain-body connection as it is about pharmacology.
Expert Insights & Advanced Considerations
1. Personalized Treatment Optimization Is Key
Leveraging genetic, psychological, and lifestyle data allows clinicians to tailor semaglutide-based therapies, enhancing long-term success and minimizing side effects. As research advances, personalized medicine will become the cornerstone of effective weight management strategies.
2. Neurobehavioral Modulation Offers Promising Horizons
Understanding how semaglutide influences neural circuitry, especially in appetite and reward centers, opens doors for combining pharmacotherapy with behavioral interventions. This integrated approach may lead to more sustainable habit changes beyond medication use.
3. The Role of Digital Health in Sustaining Results
Digital platforms facilitate real-time monitoring, dose adjustments, and behavioral coaching, significantly improving adherence and outcomes. Future innovations will likely include AI-driven personalized feedback to optimize long-term weight management plans.
4. Navigating Regulatory and Ethical Landscapes
As GLP-1 receptor agonists like semaglutide expand their indications, adherence to evolving guidelines and ethical considerations around off-label use will be critical for safe and effective application in diverse populations.
5. Ongoing Research Will Shape the Future of Weight Loss Pharmacotherapy
Emerging studies on neuroplasticity, cardiovascular benefits, and metabolic regulation suggest that semaglutide’s potential extends well beyond weight loss, promising a holistic approach to health management.
Curated Expert Resources
- Nature Reviews Endocrinology (2022): Comprehensive review of semaglutide’s multifaceted benefits, including neural and metabolic pathways.
- J Med Internet Res (2023): Insights into digital health integration for long-term pharmacotherapy success.
- Journal of Clinical Investigation (2023): Longitudinal data on neural reprogramming and behavioral change post-pharmacotherapy.
- ClinicalTrials.gov: Ongoing studies exploring novel applications and mechanisms of GLP-1 drugs.
- Weight Loss Suppliers Blog: Expert articles, case studies, and practical tips on optimizing GLP-1 therapies.
Final Expert Perspective
In the evolving landscape of weight management, understanding how semaglutide influences neural circuitry and integrating this knowledge into comprehensive care models is vital. As an expert in this field, I encourage clinicians and researchers alike to stay abreast of cutting-edge studies, harness digital innovations, and personalize interventions to unlock the full potential of these transformative therapies. Your engagement and insights can shape the future of metabolic medicine—so, I invite you to share your experiences or explore our detailed resources to deepen your expertise in this promising domain.
,