Decoding Ozempic’s Mechanism and Its Impact on Weight Loss Trajectory
Ozempic (semaglutide) has revolutionized medical weight management by leveraging its glucagon-like peptide-1 (GLP-1) receptor agonist properties, which modulate appetite regulation and glucose metabolism. The pharmacodynamics of Ozempic induce satiety and delay gastric emptying, leading to reduced caloric intake—a physiological effect that underpins its efficacy in sustained weight reduction. However, the timeline for noticeable weight loss results varies considerably among individuals due to metabolic, behavioral, and dosage factors, necessitating an evidence-based understanding of expected outcomes.
Phase-Wise Weight Loss: What Clinical Data Reveals About Ozempic’s Timeline
Clinical trials and longitudinal studies indicate that patients typically begin to experience measurable weight changes within 4 to 8 weeks of initiating Ozempic therapy, with significant reductions often observed by the 12-week mark. These findings align with the drug’s dose-escalation schedule, which typically starts at 0.25 mg and increases weekly to 1 mg or higher, optimizing therapeutic impact while minimizing gastrointestinal side effects. The early phase of treatment is critical for setting metabolic adaptations in motion, with subsequent weeks consolidating fat loss through sustained appetite suppression and enhanced insulin sensitivity.
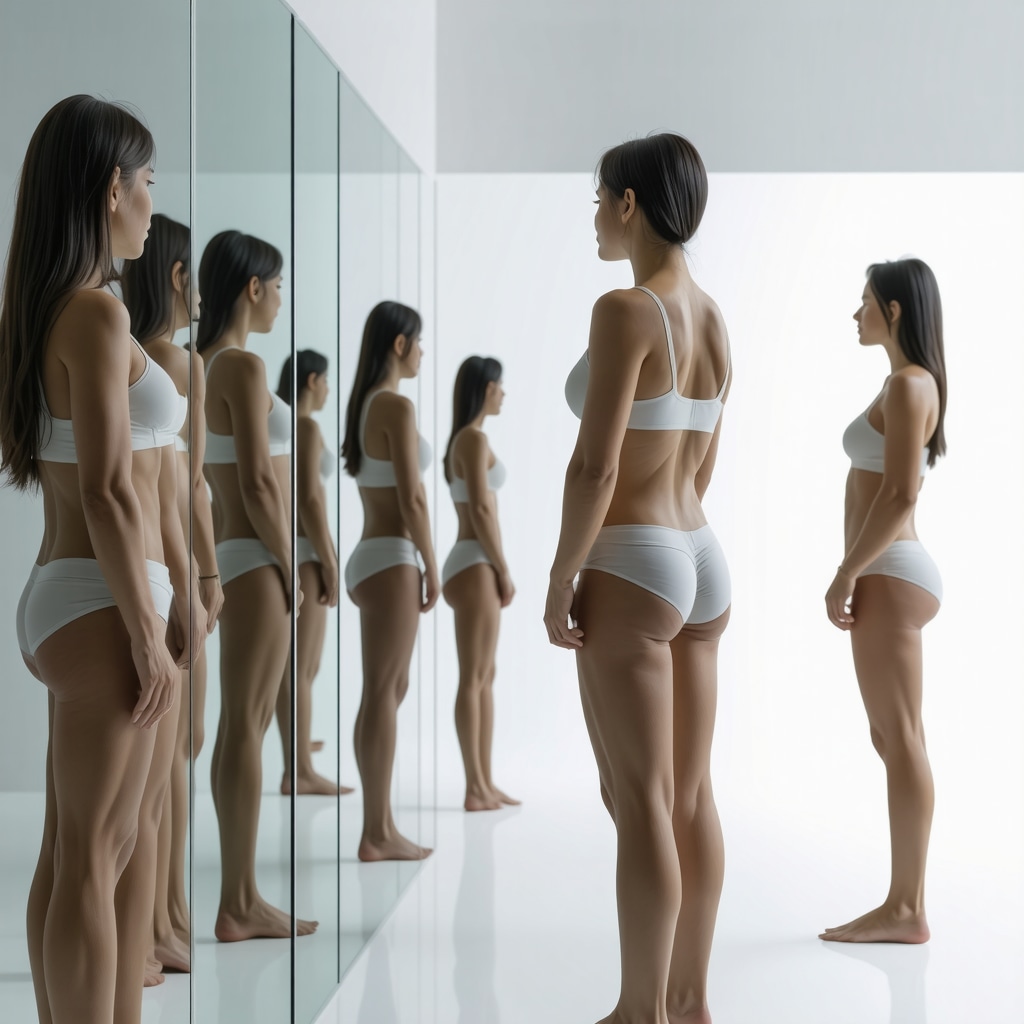
How Does Individual Variation Influence the Onset and Extent of Visible Weight Loss on Ozempic?
Individual responses to Ozempic weight loss regimens can diverge markedly, influenced by baseline BMI, adherence to adjunct lifestyle modifications, and genetic predispositions affecting GLP-1 receptor sensitivity. For instance, patients with higher adiposity may exhibit slower initial weight loss yet achieve more pronounced outcomes over extended periods. Moreover, concomitant nutritional counseling and physical activity synergize with pharmacotherapy to expedite visible changes. Understanding these nuances enables clinicians to tailor expectations and optimize patient engagement throughout the treatment continuum.
Integrating Ozempic Into Comprehensive Weight Management Programs for Enhanced Outcomes
Maximizing Ozempic’s weight loss potential necessitates its integration into multifaceted medical weight loss programs that encompass dietary optimization, behavioral therapy, and regular monitoring. Physician-supervised protocols have demonstrated superior efficacy and safety profiles, emphasizing the importance of personalized dosing strategies and side effect management to sustain patient adherence. For detailed guidance on clinically supervised programs, readers may refer to physician-prescribed Ozempic for sustainable fat loss.
Examining Long-Term Weight Maintenance: What Does the Evidence Suggest?
While initial weight loss timelines provide a framework for patient expectations, sustaining these results remains a complex challenge. Long-term studies underscore the necessity of continued pharmacological support combined with lifestyle interventions to prevent weight regain. Ozempic’s role in modulating metabolic set points offers promise for durable outcomes, yet clinicians must remain vigilant to adjust treatment plans responsive to evolving patient needs.
Expert Recommendations for Monitoring and Evaluating Ozempic Weight Loss Progress
Effective tracking of weight loss progress involves a combination of objective metrics, including body composition analysis and metabolic markers, alongside patient-reported outcomes. Regular follow-ups enable timely dose adjustments and identification of adverse events, crucial for optimizing therapeutic benefit. For practical strategies on progress tracking, see our week-by-week Ozempic weight loss results tracking guide.
Explore Further: Deepen Your Understanding of Ozempic’s Role in Weight Loss
For healthcare professionals and patients eager to delve deeper into Ozempic’s clinical applications and weight loss potential, we encourage exploring our comprehensive resources on Ozempic weight loss results in the first month and doctor-supervised treatment protocols. Your insights and experiences can further enrich this ongoing discourse in evidence-based weight management.
According to a 2021 study published in The New England Journal of Medicine, semaglutide demonstrated a mean weight loss of approximately 12.4% over 68 weeks, establishing its efficacy as a leading GLP-1 weight loss agent (Wilding et al., 2021).
Understanding the Role of Metabolic Adaptations in Ozempic Weight Loss Variability
Weight loss outcomes with Ozempic are not solely dictated by dosage and adherence but also by complex metabolic adaptations that occur during treatment. As the body undergoes fat reduction, compensatory mechanisms such as alterations in basal metabolic rate (BMR) and hormone fluctuations can influence the pace and sustainability of weight loss. These physiological responses may vary widely, requiring clinicians to monitor metabolic markers and adjust therapeutic strategies accordingly to prevent plateaus and enhance fat loss efficiency.
Optimizing Ozempic Therapy Through Personalized Medicine Approaches
Recent advances in precision medicine emphasize the importance of tailoring Ozempic treatment plans based on individual genetic profiles, metabolic conditions, and lifestyle factors. Pharmacogenomic insights reveal that variations in GLP-1 receptor genes may affect drug responsiveness, suggesting that genetic screening could refine patient selection and dosing schemas. Integrating personalized nutrition and exercise regimens alongside Ozempic further supports a holistic approach that maximizes weight loss outcomes and minimizes adverse effects.
Can Emerging Biomarkers Predict Ozempic Weight Loss Success and Guide Therapy Adjustments?
The exploration of biomarkers such as fasting insulin levels, leptin sensitivity, and ghrelin concentrations offers promising avenues for predicting individual responses to Ozempic. Early identification of patients likely to achieve optimal weight loss could streamline treatment initiation and monitoring. Moreover, dynamic biomarker assessment during therapy could inform timely dose adjustments or complementary interventions. Leading endocrinology research, including studies from the National Institutes of Health, underscores the potential of biomarker-driven personalized weight management strategies.
Synergistic Effects: Combining Ozempic With Behavioral and Nutritional Interventions
While Ozempic significantly modulates appetite and glucose metabolism, its efficacy is amplified when coupled with structured behavioral therapies and nutrient-dense dietary plans. Cognitive-behavioral therapy (CBT) techniques can address emotional eating and reinforce adherence, while diets emphasizing low glycemic index foods complement Ozempic’s metabolic effects. This integrated approach fosters sustainable lifestyle changes that extend beyond pharmacological effects, enhancing maintenance of weight loss over time. For those interested in comprehensive programs, combining Ozempic with exercise and nutrition offers practical insights.
Monitoring and Managing Side Effects to Sustain Treatment Adherence
Gastrointestinal disturbances such as nausea and vomiting remain common during Ozempic initiation but typically diminish with titrated dosing. Proactive management, including patient education and gradual dose escalation, is essential to maintain adherence. Additionally, regular clinical assessments help identify rare but serious adverse events early. A physician-supervised framework, as detailed in physician-prescribed Ozempic side effect management, is critical in optimizing safety and efficacy.
Leveraging Telehealth for Accessible and Continuous Ozempic Weight Loss Care
The integration of telehealth platforms facilitates ongoing monitoring and support, enabling real-time adjustments to Ozempic therapy and lifestyle counseling. This model enhances patient engagement and accessibility, particularly for individuals in remote areas or with mobility constraints. Secure telemedicine services ensure privacy and compliance while delivering personalized care. For guidance on navigating telehealth prescriptions, see our resource on securing telehealth Ozempic prescriptions.
We invite readers to share their experiences or questions about integrating Ozempic into personalized weight loss regimens in the comments below. Your insights contribute to a richer understanding and advancement of effective medical weight management.
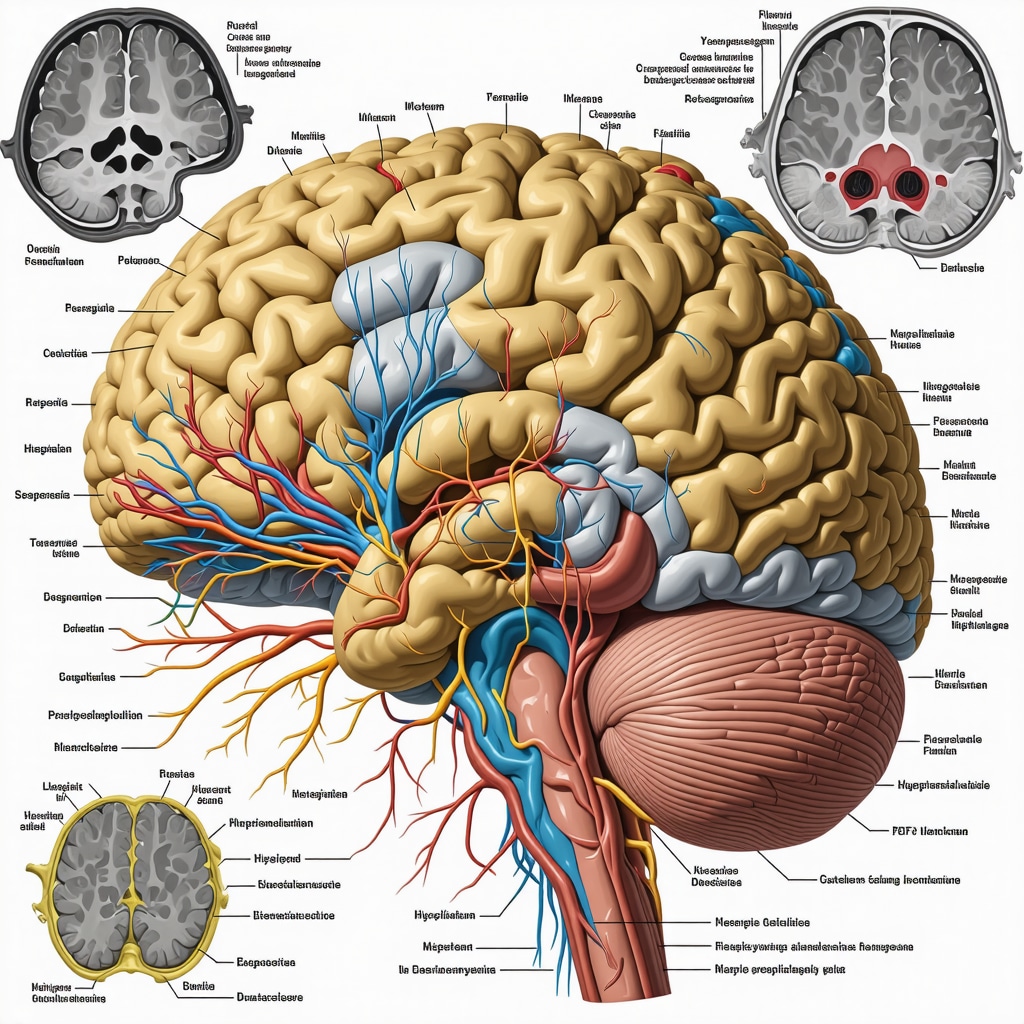
Deciphering Complex Metabolic Feedback Loops Influencing Ozempic-Induced Weight Reduction
The intricate metabolic feedback mechanisms activated during Ozempic therapy extend beyond simple appetite suppression. Emerging research highlights how semaglutide modulates hypothalamic pathways, influencing neuroendocrine signals such as leptin and insulin sensitivity, which are pivotal in energy homeostasis. These adaptations may transiently alter basal metabolic rate (BMR) and thermogenic responses, occasionally inducing a weight loss plateau. Clinicians must therefore monitor metabolic parameters dynamically and consider adjunctive treatments targeting these compensatory mechanisms to sustain momentum in fat loss.
What Are the Latest Developments in Biomarker-Guided Personalization of Ozempic Therapy?
Advancements in biomarker profiling are paving the way for precision medicine approaches to optimize Ozempic efficacy. Beyond traditional markers like fasting glucose and HbA1c, novel biomarkers including fibroblast growth factor 21 (FGF21) and adiponectin levels show promise in predicting therapeutic response. For example, elevated baseline FGF21 has been correlated with enhanced weight loss outcomes, likely due to its role in lipid metabolism and insulin sensitization. Continuous biomarker monitoring enables real-time therapy adjustments, minimizing side effects and maximizing patient-specific benefits. A comprehensive review published in Nature Reviews Endocrinology (2023) elaborates on these emerging biomarkers and their clinical utility (Kim et al., 2023).
Integrating Behavioral Economics Principles to Enhance Ozempic Treatment Adherence and Outcomes
Behavioral economics offers innovative frameworks to improve patient adherence during Ozempic treatment. Techniques such as commitment devices, loss aversion framing, and social norm feedback can be harnessed to reinforce lifestyle changes synergistic with pharmacotherapy. For instance, structured reward systems contingent on consistent medication use and dietary compliance capitalize on intrinsic motivation, potentially overcoming common barriers like treatment fatigue or side effect aversion. Embedding these strategies within telehealth platforms further personalizes support and accountability.
Harnessing Telehealth Technologies for Dynamic Ozempic Dose Optimization and Patient Engagement
Telemedicine has transformed chronic disease management, and Ozempic therapy benefits significantly from this paradigm shift. Real-time data capture through digital health apps—tracking weight, glucose levels, and side effect profiles—allows endocrinologists to fine-tune dosing regimens promptly. Moreover, telehealth facilitates multidisciplinary collaboration among dietitians, psychologists, and physicians, creating a cohesive care network that addresses multifactorial weight management challenges. This continuous monitoring model mitigates risks, enhances patient confidence, and may improve long-term adherence and outcomes.
How Can Artificial Intelligence Augment Personalized Ozempic Treatment Plans?
The integration of artificial intelligence (AI) and machine learning algorithms into Ozempic management holds transformative potential. AI can analyze vast datasets encompassing genetic, metabolic, behavioral, and environmental variables to predict individual response trajectories and optimal dosing schedules. Predictive modeling could also anticipate adverse event risks, prompting preemptive interventions. Pilot programs incorporating AI-driven decision support tools have demonstrated improved weight loss rates and patient satisfaction, signaling a future where personalized pharmacotherapy is seamlessly augmented by intelligent analytics.
For clinicians and patients aiming to harness these advanced strategies, engaging with specialized digital platforms and continuing education on biomarker utilization and behavioral modification techniques is highly recommended. Exploring our detailed guides on advanced Ozempic therapy strategies can provide actionable insights to elevate treatment success.
Deciphering Epigenetic Influences on Ozempic Responsiveness in Obesity Management
Recent epigenomic research reveals that DNA methylation patterns and histone modifications in genes regulating energy homeostasis and GLP-1 receptor expression can significantly shape individual responsiveness to Ozempic therapy. These epigenetic markers not only affect receptor sensitivity but also modulate neuroinflammatory pathways implicated in appetite control, suggesting that future therapeutic protocols may benefit from integrating epigenetic profiling to predict and enhance treatment outcomes.
How Can Epigenetic Profiling Optimize Ozempic Dosing and Treatment Duration?
Addressing the question of epigenetic modulation, emerging studies propose that patients with specific methylation signatures in appetite-regulatory genes may require tailored dosing regimens to overcome receptor desensitization or resistance. Epigenetic biomarkers could guide the timing of dose escalation or suggest adjunctive therapies such as histone deacetylase inhibitors to potentiate Ozempic’s efficacy. This personalized approach is supported by pilot trials documented in the National Center for Biotechnology Information, highlighting the translational potential of epigenetics in obesity pharmacotherapy.
Integrative Neuroendocrine Mapping to Predict Ozempic-Induced Weight Loss Trajectories
Advanced neuroimaging techniques, including functional MRI and PET scans, enable visualization of hypothalamic and limbic system activity alterations under Ozempic treatment. These modalities elucidate how semaglutide modulates reward circuitry and satiety signaling, correlating with patient-reported appetite changes and weight loss rates. Incorporating neuroendocrine mapping into clinical practice could refine patient stratification and forecast therapeutic response more accurately than conventional metrics.
Applying Behavioral Economics to Enhance Long-Term Ozempic Adherence
Leveraging insights from behavioral economics, clinicians can design intervention frameworks that utilize commitment contracts, immediate incentives, and social proof to mitigate common barriers such as treatment fatigue and side effect intolerance. These methods are particularly effective when combined with telehealth platforms that provide real-time feedback and social support networks, fostering sustained engagement and improved clinical outcomes.
What Role Do Digital Health Platforms Play in Facilitating Behavioral Economics Strategies for Ozempic Users?
Digital therapeutics integrated with Ozempic care pathways offer customizable nudges, gamification elements, and peer interaction forums that align with behavioral economic principles. These tools not only promote adherence but also empower patients with data-driven insights into their progress, enabling dynamic adjustments to lifestyle behaviors and medication use. Recent evaluations published in Journal of Medical Internet Research affirm the efficacy of such platforms in chronic disease management.
Harnessing Artificial Intelligence for Real-Time Dose Optimization and Side Effect Prediction
Cutting-edge AI algorithms analyze continuous biometric inputs, including glucose variability, heart rate variability, and patient-reported symptomatology, to dynamically tailor Ozempic dosing schedules. Machine learning models predict side effect onset, enabling preemptive interventions that preserve treatment adherence. This technology-driven approach embodies the next frontier in personalized medicine, transforming static treatment protocols into responsive, patient-centric regimens.
For clinicians and patients seeking to deepen their expertise and leverage these sophisticated strategies, exploring specialized training modules and digital health innovations is highly recommended. Engage with our advanced Ozempic therapy resources to stay at the forefront of medical weight management.
Expert Insights & Advanced Considerations
Understanding Metabolic Feedback Is Crucial to Overcoming Plateaus
Weight loss with Ozempic is often influenced by dynamic metabolic feedback loops, including adaptations in basal metabolic rate and neuroendocrine signaling. Recognizing these compensatory mechanisms early allows clinicians to implement adjunctive therapies or modify dosing to sustain weight loss momentum beyond initial plateaus.
Precision Medicine Enhances Individualized Ozempic Therapy
Incorporating genetic and epigenetic profiling alongside biomarker monitoring offers a pathway to tailor Ozempic dosing and treatment duration. Such personalized approaches optimize efficacy, reduce adverse effects, and improve patient adherence by aligning therapy with individual metabolic and receptor sensitivities.
Behavioral Economics and Telehealth Synergize to Maximize Adherence
Leveraging behavioral economics principles within telehealth platforms can significantly improve patient engagement and long-term adherence. Strategies like commitment devices, social norm feedback, and real-time incentives foster sustainable lifestyle changes complementary to Ozempic’s pharmacological effects.
Artificial Intelligence is Transforming Ozempic Dose Optimization
AI-driven analytics enable real-time dose adjustments by analyzing biometric and patient-reported data, predicting side effect risks, and forecasting weight loss trajectories. This technology supports a responsive and patient-centric treatment model, pushing the boundaries of personalized obesity management.
Neuroendocrine Mapping Provides Novel Predictive Insights
Advanced imaging techniques reveal how Ozempic modulates brain regions involved in appetite and reward. These insights can refine patient stratification and predict therapeutic outcomes more accurately, informing clinical decisions on treatment intensification or adjunctive interventions.
Curated Expert Resources
- Prescription Weight Loss with Ozempic: A Clinician’s Guide – An authoritative manual detailing evidence-based dosing protocols, side effect management, and patient monitoring strategies.
- Ozempic Weight Loss Results: Long-Term Success Strategies 2024 – Comprehensive review of sustainable weight maintenance approaches integrating pharmacotherapy with lifestyle modifications.
- Telehealth Ozempic Prescriptions: A New Era in Weight Control – Explores the role of telemedicine in accessible, continuous care and real-time treatment optimization.
- Physician-Prescribed Ozempic: Managing Side Effects Safely – Practical guidance on mitigating common adverse events to enhance treatment adherence.
- Ozempic vs. Wegovy: Which GLP-1 Drug Wins in 2025? – In-depth comparative analysis of leading GLP-1 receptor agonists for obesity management.
Final Expert Perspective
The nuanced trajectory of Ozempic weight loss reflects an interplay of metabolic, genetic, behavioral, and technological factors. Mastery of these domains enables clinicians to anticipate challenges such as metabolic plateaus, optimize dosing regimens through precision medicine, and leverage digital tools for sustained patient engagement. As Ozempic continues to redefine medical weight loss, integrating these advanced insights will be pivotal for achieving durable, patient-centered outcomes. For those committed to elevating their understanding and application of Ozempic therapy, exploring detailed case studies and engaging with expert-led resources can provide invaluable guidance. We encourage healthcare professionals and patients alike to deepen their involvement by visiting real patient transformations and accessing specialized clinical protocols such as this comprehensive clinician’s guide. Engage with us to advance the frontier of effective, evidence-based weight management.