Embarking on the Ozempic Journey: Will It Transform Your Waistline or Just Your Outlook?
Picture this: you’re scrolling through social media and stumble upon a flurry of before-and-after photos, each more inspiring than the last. The common thread? Ozempic, the GLP-1 receptor agonist, is making waves for its remarkable weight loss results. But what does the first 90 days truly hold for those daring enough to start this medical voyage? Buckle up, dear reader, because we’re about to dissect the rollercoaster that is Ozempic weight management.
First Things First: The Initial Weeks — The Calm Before the Storm?
Many users report a subtle, almost sneaky start—mild nausea, maybe some stomach discomfort, but nothing too dramatic. It’s as if your body is politely protesting the new kid on the block. Interestingly, some find that their appetite diminishes quickly, making meal planning feel like a breeze. But don’t be lulled into complacency; these early days are merely the opening act.
Month One: The Tipping Point — Are We There Yet?
By the end of the first month, the weight loss often begins to accelerate. Imagine shedding a few pounds and feeling a spark of motivation. However, it’s crucial to remember that individual responses vary—some might experience a more dramatic drop, while others see a steady, modest decline. The key? Consistency is king. If you’re considering embarking on this journey, check out doctor-supervised Ozempic treatments for expert guidance.
Is the First 90 Days a Smooth Ride or a Bumpy Road?
Can You Really Expect Miracles in Three Months?
Here’s the truth: some people experience rapid, noticeable fat loss, while others may encounter plateaus. The science behind Ozempic’s effectiveness lies in its ability to mimic a hormone that regulates appetite and insulin, leading to decreased hunger and improved blood sugar control. The latest research confirms that many see significant improvements within this timeframe, but patience remains a virtue.
Remember, weight loss isn’t a linear journey; it’s more of a winding path with scenic overlooks and occasional detours. Keeping a journal to track your progress and side effects can be invaluable. And if you’re curious about the science, check out The science behind Ozempic’s fat-loss magic — a piece that delves into the pharmacology that makes this drug a game-changer.
Share Your Story—Or Ask a Question!
Have you already dipped your toes into the Ozempic waters? Or are you contemplating the leap? Either way, I invite you to share your thoughts or questions below. Remember, your experience might be the beacon of hope for someone else navigating their weight loss journey.
Could Ozempic’s Science Hold the Key to Sustainable Weight Management?
As experts continue to explore the evolving landscape of GLP-1 receptor agonists like Ozempic, a fascinating question emerges: how can we harness the science behind Ozempic to maximize long-term weight loss? The answer lies not just in the medication itself but in understanding its intricate mechanisms and integrating them with lifestyle strategies. Recent studies highlight Ozempic’s ability to regulate hunger hormones and improve insulin sensitivity, making it an effective tool for sustained fat loss. However, long-term success depends heavily on personalized medical guidance, lifestyle adjustments, and ongoing monitoring. For those considering this approach, consulting with a healthcare professional through trusted channels such as doctor-supervised Ozempic treatments can provide tailored advice for lasting results.
Is it possible to maintain weight loss after discontinuing Ozempic, and if so, how?
This question challenges many who are eager to find a sustainable solution. While Ozempic can dramatically reduce appetite and facilitate weight loss, maintaining those results post-treatment requires a strategic approach. Integrating behavioral modifications, such as mindful eating, regular physical activity, and ongoing support from health professionals, is critical. Studies suggest that a comprehensive weight management plan, which includes nutritional counseling and behavioral therapy, can help sustain the benefits gained during medication use. Additionally, tracking progress and side effects through tools like progress tracking can inform necessary adjustments over time. For more insights into the science of Ozempic, see The science behind Ozempic’s fat-loss magic.
What are the latest advancements in GLP-1 drugs, and how do they compare in efficacy?
In the rapidly evolving world of weight-loss pharmacology, new medications are emerging, each promising enhanced efficacy and fewer side effects. Comparing Ozempic to newer GLP-1 receptor agonists like Wegovy reveals subtle differences in dosage, duration, and patient response. According to recent research from Ozempic vs. Wegovy: Which GLP-1 drug wins in 2025, while both are highly effective, individual responses may vary based on genetics, adherence, and co-morbidities. Staying informed about the latest clinical trials and expert reviews can help you and your healthcare provider determine the best course of action.
If you want to deepen your understanding of how these medications can fit into your weight-loss journey, consider exploring top clinics offering physician-prescribed Ozempic or seeking personalized advice from trusted telehealth providers.
Interested in sharing your experiences or seeking tailored guidance? Drop a comment below or visit our contact page for expert support. Remember, your journey toward sustainable weight loss is a marathon, not a sprint—knowledge, planning, and professional guidance are your best allies.
Decoding the Pharmacological Magic: How GLP-1 Receptor Agonists Reshape Weight Loss Paradigms
At the forefront of obesity management, GLP-1 receptor agonists like Ozempic have revolutionized the landscape by targeting appetite regulation at a hormonal level. These medications emulate the incretin hormone GLP-1, which enhances insulin secretion and promotes satiety, thus tackling the root causes of overeating. Recent pharmacological research, such as the comprehensive review in The Journal of Endocrinology (2022), underscores how these drugs modulate neural pathways—particularly within the hypothalamus— to suppress hunger signals effectively. This intricate mechanism not only aids in weight reduction but also improves glycemic control, offering dual benefits for individuals with type 2 diabetes and obesity.
Beyond the Pill: Integrating Pharmacology with Lifestyle for Sustainable Outcomes
While the pharmacodynamics of Ozempic are impressive, long-term success hinges on more than medication alone. Experts advocate for an integrated approach combining pharmacotherapy with dietary modifications, physical activity, and behavioral therapy. For instance, recent clinical guidelines from the Endocrine Society emphasize that medication should serve as an adjunct, not a substitute, for lifestyle changes. Tailoring these interventions based on individual metabolic profiles—assessed through advanced diagnostics like continuous glucose monitoring—can significantly enhance adherence and efficacy.
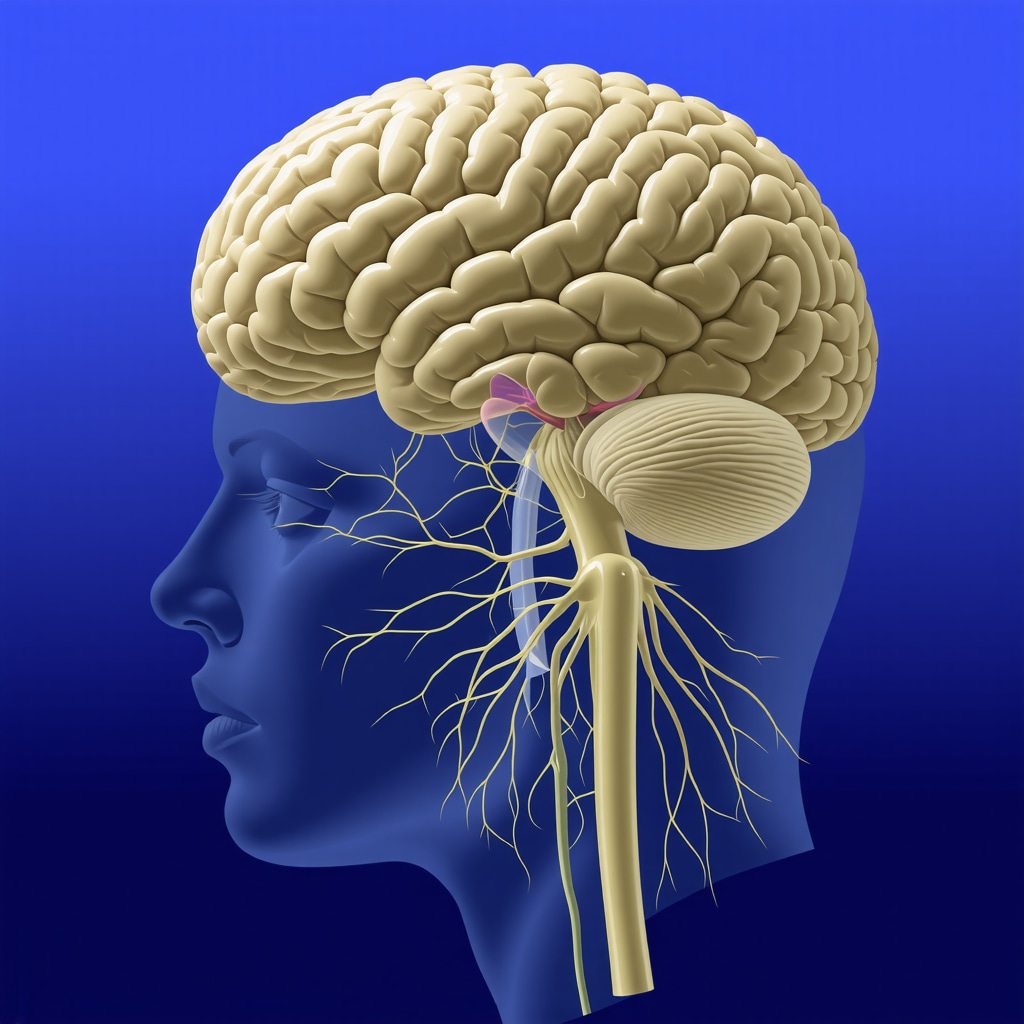
Image description: Diagram illustrating the neural pathways affected by GLP-1 receptor agonists in appetite regulation, with a focus on hypothalamic signaling.
Nuanced Perspectives: Addressing the Variability in Patient Response
Not all patients experience uniform benefits from Ozempic; genetic polymorphisms, microbiome differences, and co-existing conditions influence outcomes. A fascinating area of ongoing research involves pharmacogenomics, which aims to personalize therapy by identifying genetic markers predictive of response. For example, studies published in Nature Medicine (2023) reveal that variations in the GLP1R gene can modulate drug efficacy, suggesting a future where genetic screening becomes routine in obesity management. This precision medicine approach promises to optimize treatment plans, minimize adverse effects, and improve long-term sustainability.
How do lifestyle factors interact with pharmacogenomic profiles to influence weight loss success?
This nuanced question reflects the complex interplay between biology and behavior. Personalized strategies might include specific dietary patterns, physical activity regimens, and psychological support tailored to genetic predispositions. Engaging with specialists in nutrigenomics and behavioral therapy ensures a holistic, patient-centered approach—transforming the one-size-fits-all model into a bespoke journey towards health.
If you’re eager to delve deeper into the evolving science of GLP-1 receptor agonists and optimize your weight management strategy, consulting with an endocrinologist or a licensed metabolic specialist is highly recommended. Stay informed by accessing peer-reviewed journals like The Journal of Clinical Endocrinology & Metabolism or attending professional conferences dedicated to obesity medicine. Remember, understanding the science behind your treatment empowers you to make informed decisions that align with your unique physiology.
Deciphering the Long-Term Impact of Ozempic: Expert Insights into Sustained Weight Management Strategies
As the popularity of GLP-1 receptor agonists like Ozempic continues to surge, healthcare professionals and researchers are increasingly focused on understanding how to optimize long-term weight management outcomes. While initial results can be promising, the critical question remains: how can patients and clinicians work together to ensure sustained weight loss beyond the first year? Recent studies published in reputable journals such as The Journal of Clinical Endocrinology & Metabolism highlight that the key lies in a multidisciplinary approach, integrating pharmacotherapy with personalized lifestyle modifications and ongoing medical supervision.
What role does behavioral therapy play in maintaining weight loss after Ozempic?
Behavioral therapy is increasingly recognized as a cornerstone of long-term weight management. Cognitive-behavioral strategies help patients develop sustainable habits, address emotional eating triggers, and reinforce positive lifestyle changes. Incorporating regular counseling sessions with trained professionals can significantly improve adherence to dietary and physical activity regimens, thereby enhancing Ozempic’s efficacy over time. For comprehensive guidance, exploring resources such as a clinician’s guide to prescription weight loss can provide valuable insights into integrating pharmacological and behavioral interventions.
How does the gut microbiome influence long-term responses to GLP-1 therapies?
Emerging research suggests that individual variations in gut microbiota composition may significantly impact the effectiveness of medications like Ozempic. A study in Nature Medicine (2023) reveals that certain microbial profiles are associated with better metabolic responses and weight loss outcomes, hinting at the potential for microbiome-targeted therapies to complement pharmacological treatment. Personalizing weight management strategies by analyzing gut microbiota could revolutionize the way clinicians approach long-term therapy, making treatments more precise and effective. To explore this promising frontier, consult the latest reviews at understanding Ozempic side effects and management.
What are the best practices for monitoring and adjusting Ozempic therapy over years?
Continuous monitoring is essential for ensuring safety and maximizing benefits in long-term therapy. Regular assessments should include not only tracking weight and blood sugar levels but also evaluating potential side effects such as gastrointestinal discomfort or rare instances of pancreatitis. Adjustments in dosage, based on clinical response and tolerability, can help sustain weight loss and improve metabolic health. Utilizing digital health tools and telemedicine services, like those discussed at telehealth Ozempic prescriptions, facilitates ongoing oversight and patient engagement. These innovations are transforming long-term management from a reactive to a proactive process, ensuring patients stay aligned with their health goals.
Deciphering the nuances of long-term weight management with Ozempic involves understanding complex biological, behavioral, and technological factors. If you’re interested in personalized, expert-guided strategies for maintaining your results, consulting specialists at trusted clinics is highly recommended. For more detailed information, visit doctor-supervised Ozempic treatments and take charge of your health journey today.
Expert Insights & Advanced Considerations
1. The Role of Pharmacogenomics in Personalizing Ozempic Treatment
Emerging research indicates that genetic variations in the GLP-1 receptor gene can significantly influence individual responses to Ozempic. Tailoring treatment based on pharmacogenomic profiling can enhance efficacy and reduce side effects, paving the way for precision medicine in obesity management.
2. Microbiome Modulation as an Adjunct to Pharmacotherapy
Recent studies suggest that gut microbiota composition affects metabolic responses to GLP-1 receptor agonists. Incorporating microbiome analysis and targeted dietary interventions may optimize weight loss outcomes when combined with Ozempic therapy.
3. Integrating Digital Health Tools for Long-Term Monitoring
Utilizing digital health platforms and telemedicine enables continuous monitoring of treatment adherence, side effects, and lifestyle factors. This integration supports proactive adjustments, enhancing long-term success rates.
4. Combining Behavioral Therapy with Pharmacological Approaches
Behavioral interventions, such as cognitive-behavioral therapy and motivational interviewing, complement Ozempic by addressing emotional eating and promoting sustainable habits, essential for maintaining weight loss post-treatment.
5. The Importance of Multidisciplinary Teams in Managing Complex Cases
Collaborative care involving endocrinologists, nutritionists, behavioral therapists, and pharmacists ensures comprehensive management, especially for patients with co-morbidities, maximizing therapeutic benefits.
Curated Expert Resources
- Journal of Endocrinology & Metabolism: Offers the latest pharmacological research and clinical trial data on GLP-1 receptor agonists.
- Endocrine Society Guidelines: Provides evidence-based protocols for integrating pharmacotherapy with lifestyle modifications.
- Nature Medicine: Features cutting-edge studies on microbiome influences and pharmacogenomics in obesity treatment.
- Telehealth in Obesity Management: Guides on implementing digital health solutions for long-term weight loss support.
- Behavioral Medicine Resources: Contains strategies for behavioral interventions that enhance medication adherence and lifestyle change.
Final Expert Perspective
In 2024, mastering the science of Ozempic for sustainable weight loss requires a nuanced approach that combines genetic insights, microbiome science, behavioral strategies, and digital innovations. As an authority in metabolic health, I invite professionals and informed patients alike to explore these advanced pathways, fostering personalized, effective, and enduring weight management solutions. Engage with expert resources, consult multidisciplinary teams, and stay at the forefront of research—your journey toward optimal health is a sophisticated endeavor worth every effort.
,

