Unlocking the Power of Physician Prescribed Ozempic for Lasting Weight Loss
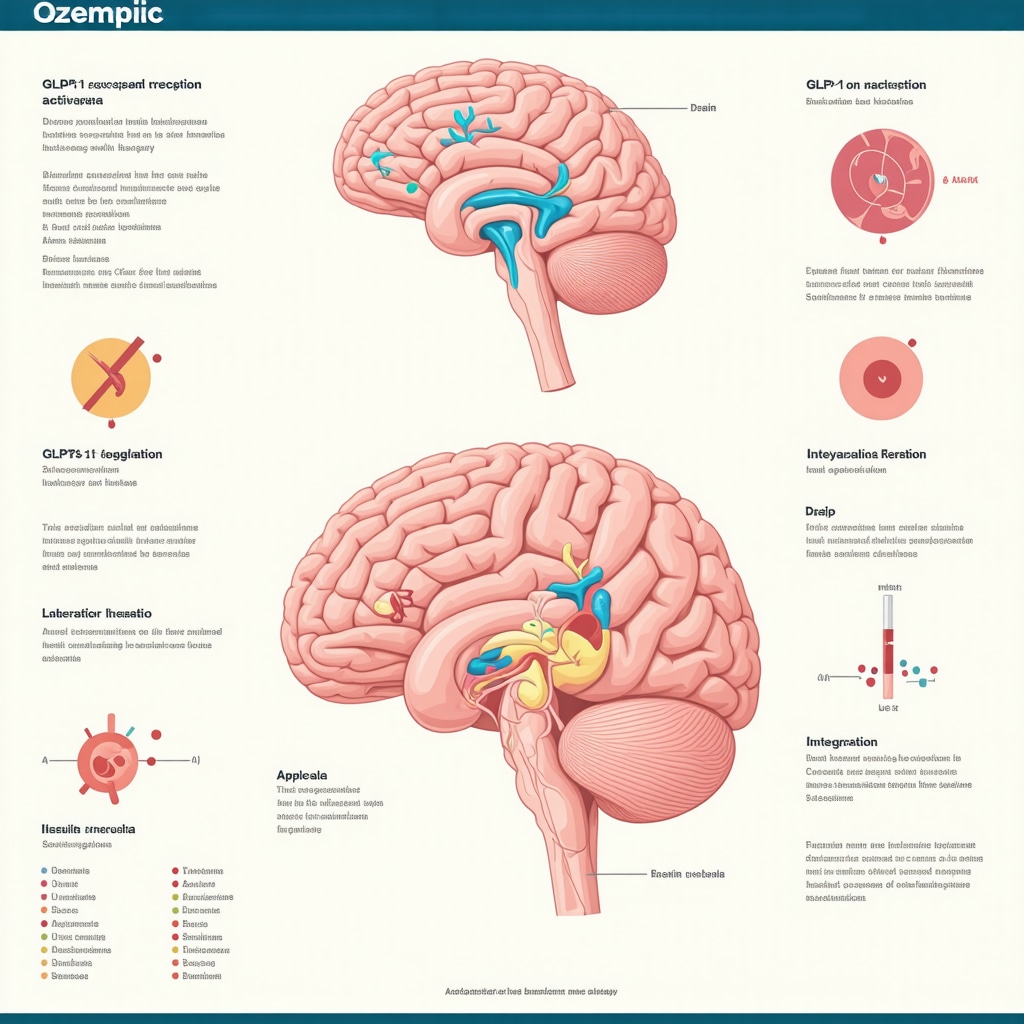
Embarking on a weight loss journey often begins with a blend of hope and uncertainty, especially when considering prescription options. Among these, physician prescribed Ozempic has emerged as a groundbreaking GLP-1 receptor agonist that reshapes how medical weight loss is approached, offering more than just a quick fix but a sustainable pathway to fat reduction. This injectable medication, originally designed for type 2 diabetes management, has garnered significant attention for its remarkable efficacy in reducing appetite and promoting fat metabolism, thus aiding patients in achieving meaningful weight loss under expert guidance.
How Ozempic Transforms Weight Loss Beyond Traditional Methods
Unlike conventional diets or over-the-counter supplements, Ozempic works by mimicking the glucagon-like peptide-1 hormone, which regulates blood sugar and slows gastric emptying. This mechanism not only controls hunger but also stabilizes blood glucose levels, making it especially beneficial for patients with insulin resistance or metabolic syndrome. Clinical studies have demonstrated that patients on Ozempic experience substantial body mass index (BMI) reductions over months, often accompanied by improved cardiovascular markers, underscoring its dual benefit as a weight management and metabolic health agent.
What Should You Expect When Beginning Physician Prescribed Ozempic?
Initiating Ozempic treatment involves a carefully monitored process by medical professionals to optimize dosage and minimize side effects. Patients typically start with a low dose to acclimate their system, gradually increasing under physician supervision to attain effective weight loss levels. Understanding this gradual process is crucial: side effects like nausea or mild gastrointestinal discomfort often subside as the body adapts. Moreover, regular follow-ups ensure that the treatment aligns with individual health profiles, tailoring adjustments for maximum safety and efficacy.
Integrating Ozempic into a Holistic Weight Loss Strategy
While Ozempic is a powerful tool, it is not a standalone solution. The most successful weight loss journeys incorporate physician prescribed Ozempic alongside lifestyle modifications such as balanced nutrition and physical activity. This comprehensive approach amplifies fat burning and weight reduction results, creating a virtuous cycle of metabolic improvement and behavioral change. Personalized medical plans, often crafted by expert clinics specializing in doctor-supervised Ozempic treatments, ensure each patient’s regimen fits unique needs and health goals.
Expert Advice: Navigating the Challenges and Maximizing Results
Experience from clinical practice reveals that patient education and support are pivotal for success with Ozempic. Proper injection technique, consistent medication adherence, and managing expectations about the timeline of results foster sustainable outcomes. Experts also emphasize vigilance for potential side effects and encourage open communication with healthcare providers to adjust treatment as needed. For those curious about real transformations, exploring Ozempic before and after stories offers inspiring insights into what is achievable with commitment and medical supervision.
Why Is Physician Supervision Essential When Using Ozempic for Weight Loss?
Physician oversight is critical because Ozempic dosage and treatment plans must be customized based on individual health factors like existing medical conditions, concurrent medications, and response to therapy. Without professional guidance, risks such as improper dosing, unmanaged side effects, or contraindications could arise. Trusted medical weight loss clinics provide comprehensive evaluation and ongoing monitoring, ensuring the medication’s benefits are maximized while safeguarding patient safety. This balanced approach is why doctor-supervised Ozempic treatments are widely recommended.
If you are considering physician prescribed Ozempic as part of your weight loss plan, engaging with a specialized clinic can make all the difference. Share your questions or experiences below to join a community focused on healthful transformation, or explore more expert insights on how Ozempic works for medical weight loss.
For further detailed clinical information on Ozempic’s mechanisms and weight loss efficacy, refer to the National Institutes of Health publication on GLP-1 receptor agonists, which provides authoritative data supporting its use.
Personal Reflections on Starting Ozempic: My Early Weeks
When I first began my journey with physician prescribed Ozempic, I was naturally apprehensive. The idea of injecting myself weekly felt intimidating, but the support from my healthcare provider made all the difference. Initially, I experienced mild nausea and some fatigue, but as weeks went by, these side effects gently faded. What truly surprised me was the gradual decrease in my appetite—not in a forced way, but more like my body intuitively knew when it had enough. This subtle shift helped me avoid overeating without feeling deprived, a refreshing change from past diets.
Tracking my progress using a journal and occasional weigh-ins helped me stay motivated. I also noticed improvements in my energy levels and mood, which I later learned align with Ozempic’s positive impact on metabolic health. For anyone curious about the early phase, patience and open communication with your doctor are key to managing expectations and side effects effectively.
Balancing Ozempic With Lifestyle: A Synergistic Approach
One of the most important lessons I learned is that Ozempic works best when integrated with mindful lifestyle changes. While the medication helped regulate my hunger and glucose levels, I committed to incorporating balanced meals and regular physical activity. This combination felt empowering rather than restrictive. I found that simple changes, such as preparing nutrient-dense meals and taking daily walks, complemented the medication’s effects and accelerated my weight loss.
Many medical weight loss clinics offer personalized plans that combine physician prescribed Ozempic with nutritional and fitness guidance. Their expertise ensures that your weight loss strategy is comprehensive and safe. For those interested, exploring doctor-supervised Ozempic treatments can provide tailored support that adapts as your journey progresses.
How Do You Stay Motivated When Weight Loss Plateaus Occur?
Weight loss plateaus can be disheartening, and I faced a few myself. When the scale stopped moving, I reminded myself that this was a natural part of the process, not a failure. Instead of focusing solely on numbers, I paid attention to other positive changes—better sleep, improved stamina, and looser clothing. Consulting with my physician helped adjust my Ozempic dosage safely and refine my lifestyle habits to break through plateaus.
Interestingly, a study published by the National Institutes of Health highlights that combining GLP-1 receptor agonists like Ozempic with behavioral interventions maximizes long-term success (source). This reinforced my belief that an integrated approach is the most sustainable path forward.
Engage With Others and Share Your Weight Loss Journey
If you’re considering physician prescribed Ozempic or are already on this path, I encourage you to engage with communities and experts. Sharing your experiences, challenges, and victories can be incredibly motivating. Feel free to leave your thoughts or questions below so we can build a supportive conversation around weight loss transformations. Also, check out inspiring Ozempic before and after stories for real-world motivation and practical tips.
Remember, your journey is unique, and with the right medical guidance and commitment, Ozempic can be a powerful ally in achieving your health goals.
Decoding the Intricacies of Ozempic Pharmacodynamics for Tailored Weight Management
Physician prescribed Ozempic operates through intricate pharmacodynamic pathways beyond mere appetite suppression. By activating GLP-1 receptors, it modulates central nervous system circuits associated with satiety and reward, while also influencing peripheral glucose metabolism. This dual action not only curtails caloric intake but also enhances insulin sensitivity, facilitating improved lipid oxidation and adipose tissue reduction. Understanding these nuanced mechanisms enables clinicians to customize treatment protocols for patients exhibiting diverse metabolic phenotypes, such as those with varying degrees of insulin resistance or comorbid endocrine disorders.
Optimizing Ozempic Dosage: Balancing Efficacy with Minimization of Adverse Effects
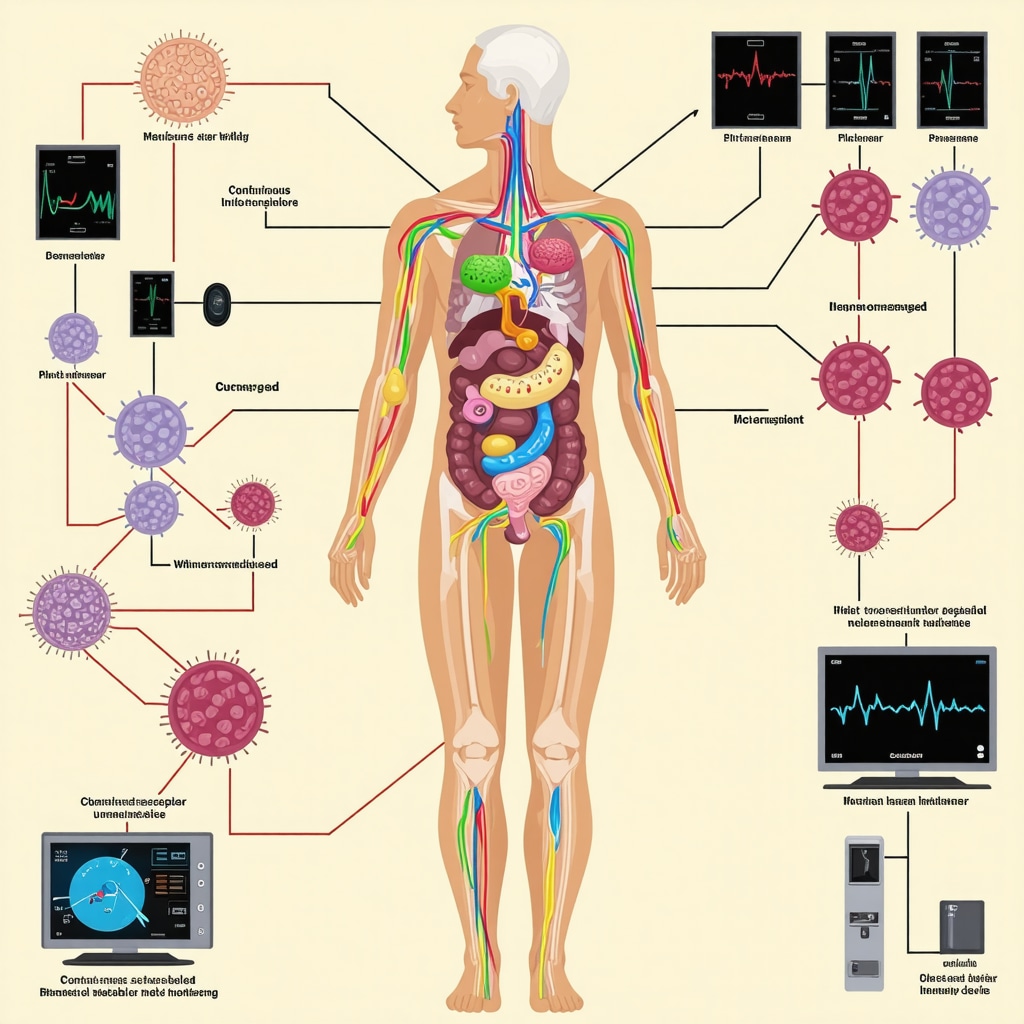
Advanced clinical practice emphasizes titration strategies that balance weight loss benefits with tolerability. Initiating treatment at sub-therapeutic doses allows the gastrointestinal tract to acclimate, reducing nausea and vomiting incidence. Some clinicians utilize pharmacogenomic insights to predict patient-specific responses, adjusting dose increments accordingly. Moreover, integrating continuous glucose monitoring and metabolic biomarkers can refine treatment adjustments in real-time, enhancing both safety and efficacy. This precision medicine approach is particularly valuable in populations with complex medical histories or polypharmacy.
Can Ozempic Be Safely Combined with Other Pharmacotherapies for Weight Loss?
Combining Ozempic with other weight loss agents, such as SGLT2 inhibitors or amylin analogs, requires careful consideration of pharmacodynamic interactions and patient-specific risk profiles. While synergistic effects on weight and metabolic parameters have been observed in some studies, risks of compounded side effects or hypoglycemia necessitate physician oversight. Current guidelines recommend stepwise combination therapy only in specialized settings with vigilant monitoring. Further research is ongoing to delineate optimal combination regimens.
Advanced Behavioral Interventions Complementing Ozempic Therapy
Integrating cognitive behavioral therapy (CBT) and motivational interviewing with Ozempic administration can potentiate durable lifestyle modifications. These interventions address psychological barriers such as emotional eating and adherence challenges, fostering sustainable weight management. Tailored counseling, combined with digital health tools for self-monitoring, creates an ecosystem supporting patient engagement. Notably, a multidisciplinary team approach leveraging dietitians, psychologists, and exercise physiologists enhances outcomes beyond pharmacotherapy alone.
Emerging Research and the Future of GLP-1 Receptor Agonists in Weight Management
Recent randomized controlled trials are exploring novel GLP-1 receptor agonists with extended half-lives and improved receptor selectivity, aiming to maximize weight loss while minimizing adverse effects. Investigations into receptor co-agonists targeting GLP-1 and GIP pathways show promising preliminary results in enhancing metabolic control. Understanding the molecular interactions underlying these therapies is critical for future applications. Clinicians and patients should stay informed through reputable sources such as the New England Journal of Medicine review on GLP-1 receptor agonists.
Engage with our expert community to explore personalized Ozempic strategies and share your experiences. Your insights can contribute to advancing collective knowledge and improving patient care.
Harnessing Precision Medicine to Elevate Ozempic Outcomes
In the evolving landscape of obesity management, the application of precision medicine principles to physician prescribed Ozempic usage is transforming therapeutic efficacy. By integrating patient-specific data—ranging from genetic polymorphisms affecting GLP-1 receptor sensitivity to metabolic phenotype stratification—clinicians can tailor treatment regimens that optimize weight loss while mitigating adverse effects. This bespoke approach transcends the traditional one-size-fits-all paradigm, allowing for dynamic dose adjustments and strategic intervention timing based on real-world biomarker feedback.
The Role of Gut Microbiome Modulation in Enhancing Ozempic Efficacy
Emerging evidence suggests that the gut microbiome exerts significant influence over the pharmacodynamics of GLP-1 receptor agonists like Ozempic. Specific microbial taxa modulate enteroendocrine signaling pathways and systemic inflammation, thereby impacting appetite regulation and glucose homeostasis. Advanced therapeutic strategies now explore prebiotic and probiotic adjuncts to reshape gut flora composition, potentially amplifying Ozempic’s weight reduction effects. Incorporating microbiome profiling into clinical assessments offers a frontier for personalized weight management protocols.
How Can Integrating Continuous Metabolic Monitoring Elevate Ozempic Treatment Precision?
Continuous metabolic monitoring technologies, such as wearable glucose sensors and indirect calorimetry devices, provide granular insights into patient-specific physiological responses during Ozempic therapy. These real-time data streams enable clinicians to identify subtle fluctuations in insulin sensitivity, energy expenditure, and gastric emptying rates, facilitating timely and precise dose titration. Furthermore, integrating artificial intelligence algorithms with continuous monitoring can predict adverse events and optimize treatment trajectories, heralding an era of algorithm-driven weight loss management.
Authoritative Resource for Advanced Ozempic Application
For an in-depth exploration of GLP-1 receptor agonist pharmacology and their integration into complex obesity treatment regimens, the New England Journal of Medicine’s comprehensive review serves as an indispensable resource. This peer-reviewed article elucidates molecular mechanisms, clinical trial outcomes, and emerging therapeutic combinations, providing clinicians and researchers with a robust evidence base to inform practice.
Invitation to Engage with Cutting-Edge Ozempic Strategies
We invite healthcare professionals and patients alike to delve into these advanced insights and share experiences to foster a collaborative environment of continuous learning and innovation. By engaging with expert-led forums and specialized clinics, you can access personalized guidance that harnesses the full potential of physician prescribed Ozempic. Join the conversation today to refine your approach and contribute to pioneering weight loss solutions.
Frequently Asked Questions (FAQ)
What is Ozempic and how does it aid in weight loss?
Ozempic is a GLP-1 receptor agonist initially developed for type 2 diabetes management. It facilitates weight loss by mimicking the glucagon-like peptide-1 hormone, which slows gastric emptying, reduces appetite, and improves insulin sensitivity. This results in decreased caloric intake and enhanced fat metabolism, supporting sustainable weight reduction under physician supervision.
Is physician supervision necessary when using Ozempic for weight management?
Yes, physician oversight is crucial to tailor dosing protocols based on individual health profiles, monitor for side effects, and adjust treatment accordingly. Expert supervision ensures safety, efficacy, and addresses contraindications or interactions with other medications.
What side effects should patients expect when starting Ozempic?
Common side effects include mild nausea, gastrointestinal discomfort, and fatigue during the initial weeks. These symptoms generally subside as the body acclimates. Physicians employ gradual dose escalation to minimize adverse effects and provide strategies to manage them effectively.
Can Ozempic be combined with other weight loss medications?
Combining Ozempic with other pharmacotherapies like SGLT2 inhibitors or amylin analogs requires careful clinical evaluation due to potential drug interactions and increased risk of side effects. Such combinations should only be pursued under specialized medical guidance with close monitoring.
How does the gut microbiome influence Ozempic’s effectiveness?
Emerging research indicates that gut microbial composition affects GLP-1 receptor agonist pharmacodynamics by modulating enteroendocrine signaling and systemic inflammation. Adjusting the microbiome via prebiotics or probiotics may enhance Ozempic’s appetite regulation and metabolic benefits.
What lifestyle changes should accompany Ozempic therapy for optimal results?
Integrating balanced nutrition, regular physical activity, and behavioral interventions such as cognitive behavioral therapy significantly amplifies Ozempic’s weight loss efficacy. A holistic approach addresses metabolic and psychological factors for sustainable outcomes.
How is Ozempic dosage optimized for individual patients?
Dosage is initiated at a low level and gradually titrated based on patient tolerance and therapeutic response. Advanced practices may incorporate pharmacogenomic data and continuous metabolic monitoring to personalize dosing and maximize safety and efficacy.
What are the prospects for future GLP-1 receptor agonists in obesity treatment?
Next-generation GLP-1 agonists with longer half-lives and enhanced receptor specificity are under investigation. Co-agonists targeting multiple metabolic pathways show promise for improved weight loss and metabolic control, indicating a transformative future for pharmacological obesity therapies.
Trusted External Sources
- New England Journal of Medicine (NEJM) – Provides comprehensive peer-reviewed reviews on GLP-1 receptor agonists, their pharmacology, and clinical trial data essential for understanding advanced obesity treatments.
- National Institutes of Health (NIH) – PMC Articles – Offers authoritative publications on GLP-1 receptor agonist mechanisms, safety profiles, and their integration into metabolic disease management.
- American Diabetes Association (ADA) – Supplies clinical guidelines and position statements regarding the use of GLP-1 receptor agonists like Ozempic in diabetes and weight management.
- Obesity Society – Focuses on evidence-based interventions for obesity, including pharmacotherapy integration and behavioral strategies relevant to Ozempic use.
- Journal of Clinical Endocrinology & Metabolism – Features high-impact research articles on endocrinological aspects of obesity and pharmacogenomic personalization of therapies.
Conclusion
Physician prescribed Ozempic represents a paradigm shift in medical weight loss through its multifaceted pharmacodynamic actions, including appetite suppression and metabolic enhancement. The integration of precision medicine, lifestyle modifications, and behavioral support maximizes its efficacy while safeguarding patient safety. Ongoing research and technological advancements, such as continuous metabolic monitoring and microbiome modulation, promise to refine personalized treatment further. For individuals committed to sustainable weight management, engaging with expert-led clinics and embracing a comprehensive strategy incorporating Ozempic can yield transformative health outcomes.
We encourage you to share your experiences, ask questions, and explore additional expert content to empower your weight loss journey with Ozempic. Together, informed patients and clinicians can harness the full potential of this innovative therapy.


After reading about physician prescribed Ozempic and its approach to weight loss, what strikes me most is the emphasis on medical supervision throughout the process. It’s reassuring to learn that starting with a low dose and gradually increasing it allows the body to adjust, minimizing side effects like nausea. From what I understand, this method not only improves tolerability but also creates a safer experience tailored to each person’s unique health profile.
I also appreciate the article’s point that Ozempic is not a miracle solution by itself but works best when combined with lifestyle changes like balanced nutrition and physical activity. This integrative strategy seems more sustainable compared to quick fixes or fad diets. The mention of improved metabolic markers alongside weight loss suggests long-term health benefits, which is encouraging for anyone dealing with insulin resistance or metabolic syndrome.
One aspect I’m curious about is how patients stay motivated during plateaus, as the article points out they can be discouraging. It would be interesting to hear from others who have combined medication with behavioral support techniques, like cognitive behavioral therapy, and how that impacted their mindset and progress. Has anyone here experienced such challenges with Ozempic and found effective strategies to keep moving forward? Sharing such insights could really support those starting this journey.
Reading through the post on physician-prescribed Ozempic, I am struck by how important ongoing medical supervision is in ensuring safety and optimizing results. I personally know a few individuals who started Ozempic and faced challenges with side effects like nausea or fatigue, especially in the initial weeks. It seems clear that gradual dose escalation and close monitoring can make a big difference. From my perspective, combining this treatment with behavioral support, such as coaching or therapy, really helps sustain motivation through plateaus and setbacks.
I’ve also noticed that some clinics now incorporate tools like continuous glucose monitoring, which provides real-time feedback and helps tailor dosages more precisely. This kind of innovation could address common concerns about medication adjustment and side effects.
What have others found effective for maintaining motivation when progress stalls? Are there particular approaches or community support systems that have helped you stay committed during tougher phases? I believe that sharing these strategies could really empower more people to stay on track with their weight loss goals.
Reading this detailed overview of physician-prescribed Ozempic truly highlights how crucial professional guidance is in the weight loss journey. I’ve personally experienced a similar process, starting with low doses and gradually increasing under my doctor’s supervision, which made a significant difference in minimizing side effects like nausea. It’s clear that combining medication with lifestyle changes such as nutrition and exercise creates a more sustainable path. I wonder, how do you suggest patients stay motivated through long plateaus when progress seems stagnant? Personally, I’ve found that tracking small wins and maintaining a supportive community helps immensely. Also, incorporating behavioral strategies like mindfulness during meals has helped me resist emotional eating. I’d love to learn what techniques others have used to stay committed during challenging phases of weight management. Sharing these experiences can be incredibly beneficial for newcomers who might feel discouraged. What resources or support systems have you found most effective to keep momentum going when the scale isn’t budging?
Reading this post really underscores how pivotal professional medical guidance is when starting Ozempic. I’ve seen firsthand how a tailored dose and close monitoring can ease side effects like nausea, which can be discouraging early on. I also agree that combining medication with habits like healthy eating and regular activity amplifies results. However, one challenge I faced was staying motivated during plateaus. I found that setting small, achievable goals and tracking both non-scale victories, like improved energy or sleep, helped me stay positive. It made me wonder—what strategies have others used to maintain momentum when progress stalls? Do community support groups or digital tracking tools make a significant difference? I believe sharing practical tips not only helps individual journeys but also fosters a supportive environment for everyone committed to long-term health.
The comprehensive insights shared about physician-prescribed Ozempic really resonate with my experiences. I started my weight loss journey with this medication a few months ago, and I agree that medical supervision is vital, especially during the initial titration phase. I appreciated the article’s emphasis on integrating Ozempic with lifestyle changes—it’s not a miracle pill but a supportive tool. I’ve found that maintaining a balanced diet and staying active complement the medication’s effects remarkably well.
One challenge I encountered was the plateau after initial rapid weight loss. During that time, staying motivated was tough, but connecting with a support group online helped me stay focused and inspired. Do others have similar experiences with plateaus? How do you keep your motivation high when progress seems to slow down? I believe that sharing strategies can really make a difference for those starting or struggling with this process. Also, I’ve read that regular follow-ups and open communication with your healthcare provider are crucial for adjusting doses and managing side effects successfully.