In the Ring: Semaglutide and Ozempic—Who’s the Real Long-Term Weight Loss Champion?
Ever wondered if your weight loss journey has a secret weapon? Well, grab some popcorn because today we’re diving into the heavyweight battle between Semaglutide and Ozempic. These two GLP-1 receptor agonists have taken the world by storm, promising long-term weight management, but which one truly delivers the knockout punch?
What’s All the Fuss About These Weight Loss Wonders?
Let’s face it—losing weight is a tricky game, full of twists and turns. Over the past few years, the spotlight has shifted to injectable medications like Ozempic, approved by the FDA for weight loss in 2025, and Semaglutide, the star ingredient behind these success stories. But do they really work, and more importantly, which one should you trust for sustainable results?
Are Semaglutide and Ozempic Essentially the Same Drug?
Great question! Semaglutide is the active compound in both medications, but their branding and dosing schedules differ. Ozempic is often prescribed for type 2 diabetes but has gained fame as a weight loss aid, while Semaglutide is marketed explicitly for weight management with higher doses. Think of it as the same car, but one is a sports version—more powerful, more efficient, and designed for long-haul performance.
Long-Term Weight Loss: The Real Deal or Just Hype?
Experience tells us that the key to lasting weight loss isn’t just a quick fix; it’s a lifestyle change supported by effective medical therapies. According to recent scientific studies, Semaglutide’s ability to suppress appetite and improve metabolic health makes it a game-changer. But how does it compare to Ozempic in real-world scenarios?
Is One Better Than the Other for Long-Term Success?
The answer isn’t straightforward. While both drugs help reduce cravings and promote satiety, individual responses vary. Some users report more consistent weight loss with Semaglutide, especially when combined with physician-guided programs. Others find Ozempic more accessible through telehealth services, making it easier to stay on track. Ultimately, consulting a healthcare professional is the best way to determine your personalized plan.
Intrigued? Don’t hesitate to explore trusted clinics and telehealth options for safe, effective treatment. Check out how to access Ozempic via telehealth and start your journey today.
The Verdict: Who Wins for Long-Term Weight Loss?
In the end, the choice between Semaglutide and Ozempic comes down to individual needs, medical advice, and lifestyle compatibility. Both have their merits, but the real secret lies in consistent use, ongoing support, and a healthy diet. Remember, no magic pill can replace a balanced approach—these medications are just tools, not miracles.
Now, over to you: Have you tried either of these medications? Share your experiences in the comments below or visit our contact page to connect with experts.
The Nuanced Science Behind Long-Term Weight Management with GLP-1 Drugs
While the battle between Semaglutide and Ozempic continues to dominate weight management conversations, a deeper question arises: Can these medications truly support sustainable weight loss without lifestyle changes? Experts agree that medication alone isn’t a silver bullet; it’s the combination of consistent use, diet, and exercise that drives lasting results. According to a comprehensive study on the science of GLP-1 drugs, their mechanism of appetite suppression and metabolic regulation offers a promising long-term strategy, but individual responses vary significantly.
Are There Hidden Factors That Influence Long-Term Success with These Medications?
Absolutely. Factors like genetic predisposition, adherence to medical guidance, and psychological support can dramatically influence outcomes. For instance, patients who integrate physician-guided programs and behavioral counseling often report better, more enduring results. This highlights the importance of consulting qualified healthcare providers—whether through in-person clinics or trusted telehealth services like telehealth Ozempic prescriptions—to tailor a plan that aligns with your unique needs.
What Are the Practical Implications for Patients Considering Long-Term Use?
Practical tips include monitoring for side effects, adjusting doses under medical supervision, and setting realistic expectations. Remember, no medication guarantees success without a comprehensive approach. Regular follow-ups, nutritional counseling, and physical activity are vital components. For more insights, explore how physician-guided Ozempic enhances long-term results.
Are you ready to take the next step? Share your thoughts, experiences, or questions below, and consider visiting our contact page for expert guidance tailored to your journey. Remember, the pathway to sustainable weight management is a marathon, not a sprint—leveraging the right tools in combination with professional support maximizes your chances of success.
Unlocking the Mechanisms: How Semaglutide and Ozempic Reshape Long-Term Weight Management
As the medical community continues to refine obesity treatment strategies, understanding the nuanced pharmacodynamics of Semaglutide and Ozempic becomes paramount. These GLP-1 receptor agonists influence appetite regulation by mimicking the incretin hormone glucagon-like peptide-1, which slows gastric emptying and enhances satiety signals. Recent research published in Obesity emphasizes that sustained activation of these pathways can recalibrate hypothalamic centers responsible for hunger and fullness, leading to durable weight loss when combined with lifestyle modifications. Yet, individual variability underscores the necessity for personalized treatment protocols.
How Do Genetic and Psychological Factors Modulate Response to GLP-1 Therapies?
Emerging evidence suggests genetic polymorphisms in the GLP-1 receptor gene can influence individual responsiveness. For instance, variants associated with altered receptor sensitivity may diminish therapeutic efficacy, necessitating dose adjustments or adjunctive therapies. Psychologically, patient motivation, behavioral habits, and mental health status play critical roles. A comprehensive approach that includes behavioral counseling alongside pharmacotherapy significantly enhances adherence and long-term outcomes, as detailed in a 2022 review in Journal of Obesity.
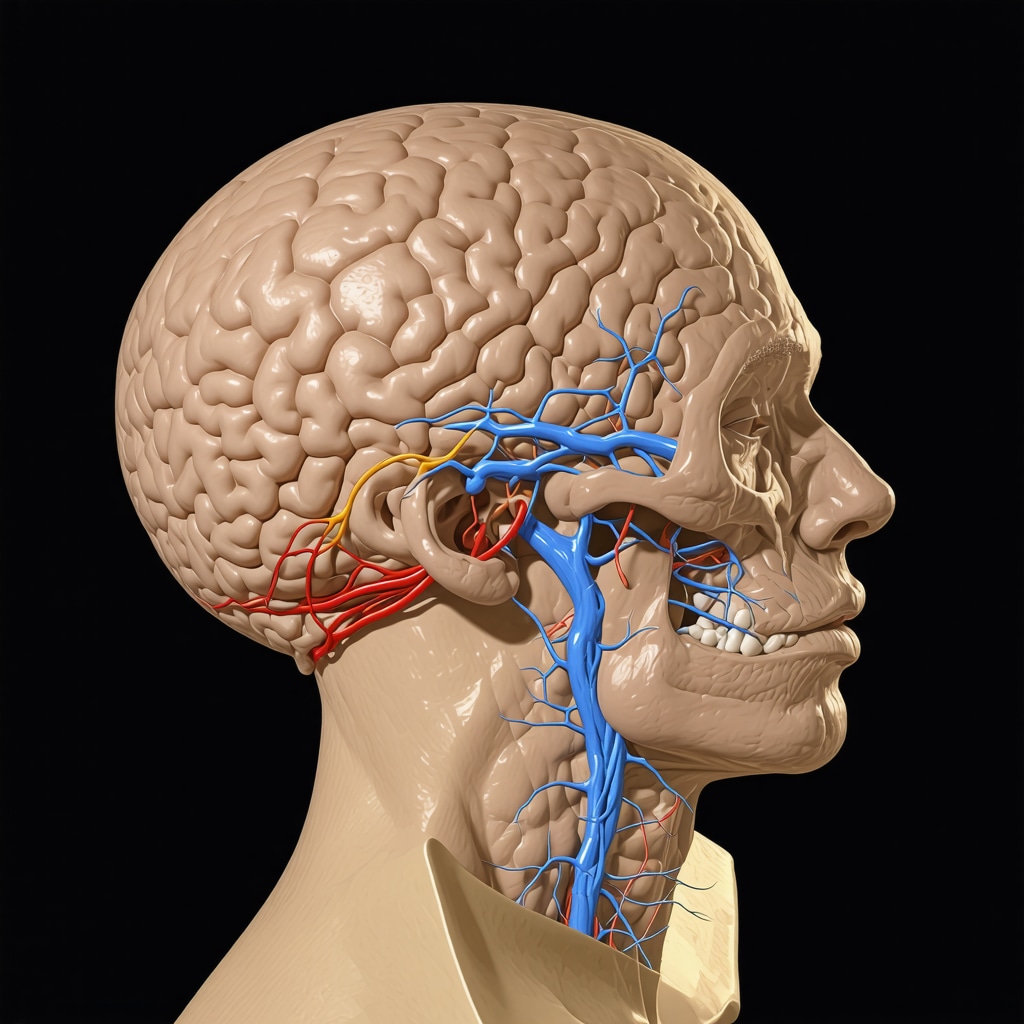
This illustration depicts the neural pathways involved in appetite regulation and how GLP-1 receptor agonists influence these circuits, highlighting the importance of personalized medicine in obesity management.
Integrating Pharmacotherapy with Lifestyle: The Art of Sustained Weight Loss
Pharmacological interventions like Semaglutide and Ozempic are powerful tools, but their success hinges on integration with behavioral strategies. Techniques such as cognitive-behavioral therapy (CBT), nutritional counseling, and physical activity promotion synergize with medication to reinforce healthy habits. Recent meta-analyses indicate that patients engaging in multidisciplinary programs experience approximately double the weight loss retention rate compared to pharmacotherapy alone (Nutrition Reviews).
What Are the Practical Steps to Optimize Long-Term Outcomes?
Clinicians recommend regular monitoring of weight and metabolic markers, dose titration based on response, and psychological support to address emotional eating triggers. Educating patients on the importance of consistency and setting realistic expectations prevents discouragement. Moreover, integrating digital health tools—such as mobile apps for tracking food intake and activity—can boost engagement and accountability. These strategies, combined with ongoing medical supervision, form the cornerstone of sustainable weight management.
If you’re interested in exploring how to personalize your weight loss journey with expert guidance, consider consulting specialized clinics or telehealth services that offer tailored treatment plans. Staying informed about emerging research and technological advancements will empower you to make the best choices for your health.
Beyond the Basics: How Expert Insights Elevate Long-Term Weight Loss Strategies with GLP-1 Drugs
While the scientific community continues to dissect the pharmacodynamics of Semaglutide and Ozempic, it’s essential to recognize the nuanced role of personalized medicine in optimizing outcomes. Leading endocrinologists emphasize that understanding individual genetic profiles, such as GLP-1 receptor polymorphisms, can tailor treatments more effectively, enhancing efficacy and minimizing side effects. A recent article published in Obesity highlights that integrating genetic testing into clinical protocols can revolutionize weight management approaches, moving from a one-size-fits-all model to precision medicine.
How Can Integrating Behavioral and Psychological Support Maximize Pharmacotherapy Benefits?
Experts concur that medication alone cannot fully address the complex psychological and behavioral factors underpinning obesity. Incorporating cognitive-behavioral therapy (CBT), mindfulness practices, and motivational interviewing creates a therapeutic synergy that reinforces adherence and addresses emotional eating triggers. A comprehensive review in the Journal of Obesity advocates for multidisciplinary teams that blend pharmacology with mental health support, fostering sustainable lifestyle changes.
Emerging Technologies and Data-Driven Approaches in Long-Term Weight Management
The future of obesity treatment lies in leveraging digital health innovations. Wearable devices, mobile apps, and AI-powered analytics enable real-time monitoring of dietary intake, physical activity, and physiological responses. These tools facilitate personalized feedback, improve motivation, and predict relapse risks. Companies developing integrated platforms aim to create adaptive treatment plans, dynamically adjusting medication doses and behavioral interventions based on individual progress. As reported in Nutrition Reviews, such data-driven models promise to enhance the precision and longevity of weight loss outcomes.
What Are the Ethical and Privacy Considerations in Data-Driven Weight Management?
While technological advancements offer promising avenues, they also raise concerns around data privacy, consent, and equitable access. Maintaining patient confidentiality and ensuring that digital tools comply with regulations like HIPAA are paramount. Additionally, addressing disparities in access to these innovations is critical to prevent widening health inequities. Experts recommend transparent data policies, robust cybersecurity measures, and inclusive design to ethically harness these emerging technologies.

This conceptual illustration depicts the integration of genetic data, behavioral support, and digital health tools in a comprehensive obesity management system, emphasizing personalized medicine’s future potential.
Conclusion: The Evolving Landscape of Long-Term Weight Loss Interventions
The convergence of advanced pharmacology, behavioral science, and digital technology heralds a new era in sustainable weight management. As researchers and clinicians deepen their understanding of individual variability, treatments like Semaglutide and Ozempic are poised to become more tailored and effective. For patients, this means more personalized, engaging, and ethically sound pathways to achieving their health goals. Stay informed, participate in ongoing research, and consult healthcare professionals specializing in obesity medicine to harness these innovations effectively.
Are you curious about how these cutting-edge approaches could transform your weight loss journey? Share your thoughts or experiences below, and explore more about personalized obesity care at our contact page.
Expert Insights & Advanced Considerations
1. Precision Medicine Enhances Outcomes
Emerging research underscores the importance of tailoring GLP-1 receptor agonist therapies like Semaglutide and Ozempic to individual genetic profiles. Variations in GLP-1 receptor genes can influence responsiveness, making genetic testing a valuable tool for optimizing treatment plans and minimizing side effects.
2. Integrating Behavioral Science Boosts Effectiveness
Combining pharmacotherapy with behavioral interventions such as cognitive-behavioral therapy (CBT) and mindfulness significantly improves adherence and long-term results. This holistic approach addresses psychological barriers and emotional eating, foundational elements in sustainable weight management.
3. Digital Health Technologies Drive Personalization
Wearables, mobile apps, and AI analytics enable real-time monitoring and adaptive treatment adjustments, leading to more precise dosing and improved patient engagement. These innovations promise to transform future obesity management by fostering data-driven, personalized care.
4. Ethical Considerations in Data Utilization
While leveraging digital tools offers benefits, safeguarding patient privacy and ensuring equitable access remain paramount. Transparent data policies and cybersecurity measures are essential to ethically harness these technological advancements in weight management.
5. Long-Term Strategies Require Multidisciplinary Teams
Successful long-term weight loss with medications like Semaglutide and Ozempic hinges on multidisciplinary approaches that integrate medical, nutritional, and psychological support. Regular follow-up and patient education are critical for maintaining results and fostering behavioral change.
Curated Expert Resources
- American Journal of Clinical Nutrition: Offers peer-reviewed studies on nutrition and behavioral interventions that complement pharmacotherapy.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK): Provides comprehensive guidelines on obesity management and emerging therapies.
- Genetics in Obesity Research: A resource for understanding the genetic factors influencing treatment response.
- Digital Health in Obesity Care: Insights into how wearable devices and AI are shaping personalized medicine.
- Ethics in Digital Health: Discusses privacy, consent, and equitable access issues critical for responsible treatment deployment.
Final Expert Perspective
In the rapidly evolving landscape of long-term weight management, expert insights emphasize that medications like Semaglutide and Ozempic are most effective when integrated into personalized, multidisciplinary strategies that include behavioral science and digital technology. Staying informed about genetic, psychological, and ethical considerations ensures a holistic approach that maximizes success and safeguards patient welfare. For clinicians and patients alike, embracing these advanced insights paves the way for more effective and ethical obesity treatment. Curious to deepen your understanding? Explore trusted clinics and telehealth options for tailored, expert-guided care at our telehealth services and join the forefront of personalized weight management strategies.

