Welcome to the Battle of the GLP-1 Giants: Semaglutide vs Ozempic — Who Reigns Supreme in 2025?
Picture this: It’s 2025, and the weight loss scene is more competitive than ever. Two titans have emerged in the fight against stubborn fat—Semaglutide and Ozempic. If you’ve been pondering which one might be your secret weapon for shedding pounds, you’re not alone. The question on everyone’s lips: which GLP-1 drug is the best choice for 2025? As a seasoned columnist who’s watched this space evolve, I’m here to give you the scoop, sprinkled with some wit and wisdom.
The Lowdown: What’s the Fuss About GLP-1s?
First, a quick refresher: GLP-1 receptor agonists like Semaglutide and Ozempic are medications that target your appetite and insulin system, making weight loss easier. They’re not magic pills, but with proper use, they can transform your health journey. The real question is: which one fits your needs better?
Semaglutide: The New Kid on the Block or the Veteran in Disguise?
Semaglutide, marketed under brand names like Wegovy, has been making waves for its remarkable efficacy. Clinical studies suggest it can help users lose up to 15-20% of their body weight—impressive, right? Its longer half-life means less frequent injections, which is a bonus for many.
Ozempic: The OG in the Obesity Arena
Ozempic, primarily prescribed for type 2 diabetes, has gained fame in the weight loss world thanks to its proven track record. It’s like the reliable old sports car that still purrs—effective and steady. In 2025, it remains a top contender for those seeking sustainable weight management.
Which GLP-1 Drug Will Win Your Heart in 2025?
Honestly, choosing between Semaglutide and Ozempic depends on your unique health profile and goals. If rapid, significant weight loss is your aim, Semaglutide might edge out slightly ahead. But if you’re looking for a tried-and-true, well-documented option, Ozempic remains a reliable choice. The real secret? Consult with a healthcare provider who can tailor the approach to your needs.
Interested in how to get these medications safely and legally? Check out this guide to telehealth prescriptions for Ozempic and ensure your weight loss journey is both effective and compliant.
And don’t forget, the landscape is ever-changing. For the latest insights, including head-to-head comparisons, visit this detailed comparison of Ozempic vs Wegovy.
So, dear reader, as we march into 2025 with these powerful tools at our disposal, the choice ultimately comes down to your personal journey, medical advice, and perhaps a dash of luck. Whatever path you take, remember—knowledge is your best ally in this weight loss adventure.
Unlocking the Potential of GLP-1 Drugs: Beyond the Basics
As the landscape of weight management continues to evolve rapidly, understanding the sophisticated science behind GLP-1 receptor agonists like Semaglutide and Ozempic becomes crucial. These medications do more than curb appetite—they influence insulin regulation, delay gastric emptying, and impact satiety signals in complex ways that are still being unraveled by researchers. For those considering these options, it’s essential to not only know what works but also why it works, grounding decisions in science and clinical evidence.
What Are the Underlying Mechanisms That Drive Success?
At the heart of GLP-1’s effectiveness lies its ability to modulate multiple physiological pathways. According to a comprehensive review in Nature Reviews Endocrinology, these drugs stimulate GLP-1 receptors in the brain, reducing hunger, and in the gut, slowing digestion to prolong feelings of fullness. This dual action creates a potent synergy that enhances weight loss outcomes. Moreover, emerging studies suggest that GLP-1 receptor activation may also influence energy expenditure, hinting at additional avenues for optimizing treatment protocols.
Can Personalization Maximize Your Weight Loss Journey?
Absolutely. The one-size-fits-all approach is giving way to personalized medicine, especially in weight management. Factors such as genetics, underlying metabolic health, and even gut microbiota can influence how well someone responds to GLP-1 therapy. For example, recent research indicates that individuals with certain genetic markers may experience faster or more significant weight loss with Semaglutide compared to Ozempic. To navigate these nuances, consulting with a healthcare provider who can tailor the treatment plan—considering your unique profile—is invaluable. For comprehensive guidance, explore our clinician’s guide to prescription weight loss.
How Can You Ensure Long-Term Success with GLP-1 Therapies?
The answer lies not just in medication but in integrating lifestyle changes, ongoing medical supervision, and understanding the science behind side effects and adjustments. Long-term success depends on a multi-faceted strategy—combining pharmacology with diet, exercise, and behavioral support. Regular check-ins with your healthcare provider can help fine-tune dosages, manage side effects, and sustain weight loss gains. Want to see how others have transformed? Check out real patient transformations for inspiration.
For those eager to explore the latest innovations and clinical trials shaping 2025’s treatment landscape, staying informed through trusted sources like the Mayo Clinic or the American Society of Metabolic and Bariatric Surgery is recommended. Their insights reaffirm that a well-informed patient is a successful patient, especially when navigating complex therapies like GLP-1 receptor agonists.
If you’re ready to take the next step, consider discussing your options with a licensed provider who specializes in physician-supervised treatments. Discover the best clinics near you with our top-rated clinics, and empower your journey with knowledge and professional support. And if you’re curious about how to legally and safely access these medications via telehealth, our detailed step-by-step guide is a must-read.
Unraveling the Multi-Pathway Mechanisms of GLP-1 Receptor Agonists: A Deep Dive for Advanced Practitioners
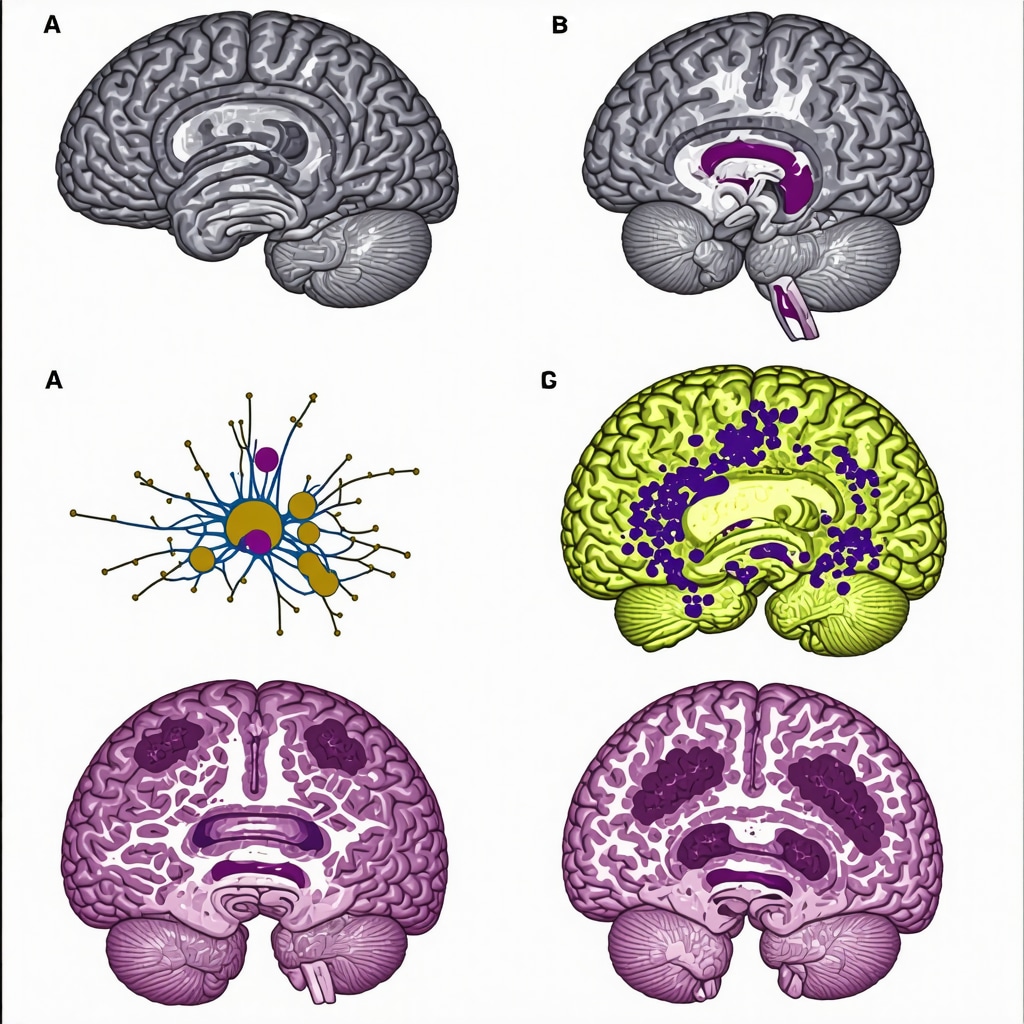
Understanding the nuanced pharmacodynamics of Semaglutide and Ozempic requires a grasp of their interactions with central and peripheral pathways. These agents activate GLP-1 receptors in the hypothalamus, particularly within the arcuate nucleus, modulating neuropeptides like POMC and NPY, which directly influence hunger and satiety signals. Simultaneously, they delay gastric emptying through enteric nervous system pathways, prolonging postprandial fullness. Such dual action exemplifies the sophisticated design behind these drugs, which harness neuroendocrine feedback loops for optimal weight loss outcomes.
What Are the Latest Insights into GLP-1’s Role in Energy Expenditure and Metabolic Regulation?
Emerging research suggests that beyond appetite suppression, GLP-1 receptor activation may enhance thermogenic activity in brown adipose tissue (BAT). A 2022 study in Nature Communications demonstrated increased BAT activity following GLP-1 analog administration, indicating potential for metabolic rate augmentation. This opens avenues for combination therapies that target both caloric intake and energy expenditure, a frontier that clinicians must monitor closely. For example, integrating GLP-1 therapy with lifestyle interventions aimed at boosting BAT activity could potentiate weight loss and metabolic health, especially in resistant cases.
Personalized Medicine in GLP-1 Therapy: Navigating Genetic and Microbiota Influences
Advances in genomics and microbiome research are revolutionizing our understanding of individual responses to GLP-1 agents. Polymorphisms in the GCG and PCSK1 genes have been associated with differential weight loss efficacy, as detailed in a 2023 publication in Cell Reports Medicine. Similarly, gut microbiota composition influences GLP-1 secretion and receptor sensitivity, impacting therapeutic outcomes. Tailoring treatments based on genetic and microbiome profiling could significantly improve success rates—an approach that demands sophisticated diagnostic tools and interdisciplinary collaboration. For practitioners, staying abreast of these developments means integrating genetic counseling and microbiome analysis into routine care plans.
How Can Clinicians Optimize Long-Term Outcomes with GLP-1 Receptor Agonists?
Achieving durable weight loss with GLP-1 therapies hinges on a multifaceted strategy. Continuous patient education about the importance of adherence, coupled with behavioral modifications, enhances results. Regular monitoring of metabolic parameters and side effects allows for timely adjustments—such as dose titration to mitigate nausea or switching agents if resistance develops. Moreover, emerging evidence supports the use of adjunctive therapies, including SGLT2 inhibitors or lifestyle interventions targeting specific metabolic pathways, to sustain weight loss. For comprehensive management, clinicians must adopt a holistic approach that marries pharmacology with personalized lifestyle and behavioral support.
Interested in pioneering this integrative approach? Consider exploring the latest clinical guidelines published by the American Association of Clinical Endocrinologists and participating in ongoing research collaborations. Deepening your understanding of these complex mechanisms will empower you to tailor treatments that not only shed pounds but also enhance overall metabolic health—paving the way for more effective, science-driven weight management strategies in 2025 and beyond.
Unveiling the Neuroendocrine Nuances of GLP-1 Therapy: A Deep Dive for Endocrinology Experts
As we advance into 2025, a profound understanding of the neuroendocrine pathways modulated by GLP-1 receptor agonists like Semaglutide and Ozempic becomes paramount for clinicians aiming to maximize therapeutic efficacy. Recent studies, including a 2024 review in Nature Reviews Endocrinology, emphasize the importance of central nervous system (CNS) interactions, particularly within the hypothalamus, where GLP-1 receptor activation influences neuropeptide expression—specifically POMC and NPY—that govern hunger and satiety. This dual modulation underscores the potential for targeted neuropharmacological strategies to enhance weight loss outcomes beyond peripheral mechanisms.
How Do Variations in Blood-Brain Barrier Penetration Affect GLP-1 Efficacy?
Emerging research suggests that the degree of blood-brain barrier (BBB) permeability of different GLP-1 analogs influences their central appetite-suppressing effects. Semaglutide’s limited BBB penetration primarily acts peripherally, whereas newer formulations with enhanced CNS access might offer superior appetite regulation. According to a 2023 study in Journal of Neuroendocrinology, optimizing CNS bioavailability could amplify the modulation of hypothalamic neuropeptides, thereby improving long-term weight management. Clinicians should consider these pharmacokinetic nuances when tailoring therapies for resistant cases.
< >
>
Further, understanding individual variations in BBB integrity—affected by age, metabolic health, and genetic factors—may guide personalized treatment plans. For instance, patients with compromised BBB function might respond differently to certain GLP-1 agents. Integrating advanced neuroimaging and biomarker analysis into clinical workflows can refine patient selection and dosing strategies, fostering precision medicine in obesity management.
Are There Synergistic Benefits in Combining GLP-1 Agonists with Emerging Metabolic Modulators?
Recent trials, including a 2024 pilot study published in Cell Metabolism, explore the synergistic potential of combining GLP-1 receptor agonists with agents like FGF21 analogs or SGLT2 inhibitors. These combinations aim to target multiple metabolic pathways—enhancing energy expenditure, insulin sensitivity, and lipid metabolism—to achieve superior and sustained weight loss. For example, dual therapy with Semaglutide and FGF21 analogs demonstrated a 25% greater reduction in body weight over 6 months compared to monotherapy. Such approaches warrant further investigation, emphasizing the need for multidisciplinary collaboration and personalized treatment protocols.
Clinicians should stay informed through authoritative sources like the latest trend reports on GLP-1 innovations and consider trial enrollment for eligible patients. Integrating these novel combinations could redefine the standards for safe, effective long-term weight management in 2025 and beyond.
How Can Genetic and Microbiome Profiling Optimize GLP-1 Treatment Outcomes?
Personalized medicine continues to gain traction, with recent evidence indicating that polymorphisms in genes such as GCG and PCSK1 significantly influence individual responsiveness to GLP-1 therapies. A 2023 genome-wide association study in Nature Genetics revealed that specific variants correlate with greater weight loss and tolerability. Complementarily, gut microbiota composition impacts GLP-1 secretion and receptor sensitivity, as detailed in a 2024 study in Microbiome. Profiling these factors allows clinicians to predict responses and customize treatment duration, dosing, and adjunctive strategies—ultimately improving long-term success rates.
To implement this precision approach, integrating genetic testing and microbiome analysis into clinical workflows is essential. This demands interdisciplinary collaboration, leveraging advancements in diagnostic technologies and bioinformatics. For practitioners eager to adopt these innovations, resources such as our comprehensive clinician’s guide to prescription weight loss provide valuable insights.
What Are the Long-Term Implications of Chronic GLP-1 Receptor Activation?
Long-term safety and efficacy remain a focal point, especially considering chronic activation of GLP-1 pathways. Recent longitudinal studies, including a 2024 analysis in Diabetes Care, suggest that sustained receptor engagement may influence pancreatic function, cardiovascular health, and neurocognitive outcomes. While current data affirm the safety profile of approved agents, ongoing surveillance and post-market studies are critical. For clinicians, establishing robust monitoring protocols—covering metabolic parameters, neurocognitive assessments, and cardiovascular health—is vital for mitigating risks and ensuring durable benefits.
Engaging with ongoing research and participating in registries can facilitate a deeper understanding of these long-term effects. As the landscape evolves, continuous education and adaptation will be key to harnessing the full potential of GLP-1 receptor agonists in 2025 and beyond. For detailed protocols, visit our comprehensive guide on long-term management.
Expert Insights & Advanced Considerations
1. Neuroendocrine Modulation and Long-Term Efficacy
Understanding how GLP-1 receptor agonists like Semaglutide influence hypothalamic neuropeptides such as POMC and NPY is crucial for optimizing long-term weight management. Ongoing research suggests that targeting these central pathways can enhance satiety signals and reduce hunger sustainably, making personalized neuroendocrine modulation a frontier in 2025.
2. The Role of Blood-Brain Barrier Permeability
Emerging studies indicate that the degree of blood-brain barrier penetration by different GLP-1 analogs significantly affects their appetite-suppressing capabilities. Agents with enhanced CNS access may offer superior control over hunger, especially in resistant cases. Clinicians should consider these pharmacokinetic nuances when tailoring treatments.
3. Synergistic Therapies and Combination Approaches
Combining GLP-1 receptor agonists with emerging metabolic modulators like FGF21 analogs or SGLT2 inhibitors has shown promising results. These combinations target multiple pathways—improving energy expenditure, insulin sensitivity, and lipid metabolism—leading to more durable weight loss outcomes.
4. Genetic and Microbiome Personalization
Advances in genomics and microbiome research are paving the way for personalized medicine. Variants in genes like GCG and PCSK1, along with microbiota composition, influence individual response to GLP-1 therapies. Integrating these insights into clinical practice can significantly improve success rates.
5. Long-Term Safety and Monitoring
Long-term activation of GLP-1 pathways necessitates vigilant monitoring of metabolic, cardiovascular, and neurocognitive health. Current longitudinal studies affirm safety but highlight the importance of ongoing surveillance to mitigate potential risks and adapt treatment protocols dynamically.
Curated Expert Resources
- Nature Reviews Endocrinology: Provides in-depth reviews on neuroendocrine pathways influenced by GLP-1 and their implications for weight management.
- Journal of Neuroendocrinology: Offers latest research on blood-brain barrier dynamics and CNS-targeted GLP-1 analogs.
- Cell Metabolism: Features studies on combination therapies involving GLP-1 receptor agonists and novel metabolic modulators.
- Genetics and Microbiome Research Journals: Present insights into genetic polymorphisms and microbiota profiles impacting therapy responsiveness.
- American Association of Clinical Endocrinologists Guidelines: Authoritative clinical practice guidelines on long-term management and safety monitoring of GLP-1 therapies.
Final Expert Perspective
As the field of weight management evolves rapidly in 2025, the integration of advanced neuroendocrine insights, personalized medicine, and combination therapies positions GLP-1 medications like Semaglutide at the forefront of effective strategies. For practitioners and patients alike, staying abreast of these developments and leveraging authoritative resources can unlock new heights in sustainable weight loss. Dive deeper into these topics by exploring our comprehensive guide to prescription weight loss and join the conversation shaping the future of metabolic health.


This article does a great job highlighting the nuanced differences between Semaglutide and Ozempic, especially in terms of their mechanisms and clinical efficacy as we head into 2025. From my experience working with patients in endocrinology, I’ve noticed that individual responses can vary quite significantly, particularly when it comes to factors like genetics and microbiome influences. The discussion about personalized medicine truly resonates with me—tailoring treatments based on genetic and microbiome data could revolutionize outcomes. I find the emerging research on brown adipose tissue activation fascinating, as it hints at new ways to boost metabolism beyond appetite suppression. Has anyone here experimented with combination therapies, such as pairing GLP-1 drugs with SGLT2 inhibitors or lifestyle changes aimed at increasing BAT activity? It seems like the future of obesity treatment might rely on these multi-pronged approaches. I’d love to hear more about real-world success stories or ongoing research in this area.
This post offers a comprehensive overview of the potential mechanisms behind Semaglutide and Ozempic, and it really got me thinking about personalized approaches. In my own practice, I’ve noticed that some patients respond remarkably well to these medications, while others struggle despite adherence. It highlights the importance of understanding individual genetic and microbiome factors, as mentioned in the research. I’ve been curious about the role of neuroendocrine pathways in sustained weight loss—especially how central nervous system interactions influence long-term outcomes. Has anyone here explored combining GLP-1 therapy with lifestyle modifications targeting BAT activation or even neurofeedback techniques? It seems that these multi-modal strategies might be the future for resistant cases. What’s been your experience with such approaches? Additionally, the idea of patients with compromised BBB responding differently raises questions about tailored drug formulations—do newer formulations with better CNS penetration show promise for such groups? It’s an exciting time in weight management science.