Welcome to the Future of Weight Loss: The Ozempic Revolution
Imagine a world where shedding pounds isn’t just a fleeting victory but a sustainable journey. Enter Ozempic, the injectable superstar that’s turning heads in the realm of long-term fat loss. But what’s the science behind its success? Is it magic, or is there a method to the madness? Buckle up, because we’re diving deep into the fascinating science behind how Ozempic supports sustained weight management.
The Hormonal Symphony: How Ozempic Plays Its Part
At the heart of Ozempic’s magic lies its ability to mimic a natural gut hormone called GLP-1 (glucagon-like peptide-1). Think of GLP-1 as your body’s own weight management maestro, orchestrating appetite, insulin secretion, and digestion. When Ozempic steps into the scene, it amplifies this hormonal symphony, leading to reduced hunger and better blood sugar control—a double whammy for weight loss enthusiasts.
Is It Just About Cutting Hunger? Or Is There More?
While decreasing appetite is the headline act, Ozempic also influences how your body processes sugars and fats, making it a comprehensive player in metabolic health. This dual action not only helps shed pounds initially but also supports maintaining those results over the long haul.
Why Long-Term Fat Loss Requires More Than Just a Shortcut
Let’s face it: quick fixes are tempting but often fleeting. The real triumph lies in sustainable habits, and Ozempic provides the support system needed to reinforce lifestyle changes. It’s like having a reliable co-pilot that keeps you on course amid the turbulence of cravings and setbacks.
Could This Be the Holy Grail for Weight Management?
While Ozempic offers promising results, it’s not a silver bullet. Success also depends on diet, exercise, and consistent medical guidance. An inspiring statistic from real patient stories proves that with the right approach, long-term fat loss is very much within reach.
Curious about how to incorporate Ozempic safely into your weight loss journey? Check out this comprehensive guide for expert insights and tailored strategies.
Beyond Appetite Control: The Multifaceted Impact of Ozempic on Weight Management
While many focus on Ozempic’s ability to suppress hunger, its influence on metabolic pathways offers a more comprehensive understanding of its role in sustainable weight loss. By mimicking GLP-1, Ozempic not only curbs cravings but also enhances insulin sensitivity and promotes healthy digestion, creating an environment conducive to long-term fat reduction. This synergy of effects is what sets it apart from fleeting diet trends, emphasizing the importance of addressing underlying metabolic health for lasting results.
Can Ozempic Support a Lifestyle that Lasts?
Many wonder if medication alone can sustain weight management or if it merely acts as a temporary aid. The answer lies in integrating Ozempic within a broader framework of lifestyle modifications, including balanced nutrition and regular physical activity. Evidence suggests that when combined with behavioral changes, patients experience more durable outcomes—highlighted in research on long-term support. The real challenge is maintaining motivation and consistency, which healthcare providers can bolster through personalized coaching and ongoing monitoring.
How Can Medical Guidance Maximize Ozempic’s Potential?
Expert supervision ensures safe dosage adjustments, minimizes side effects, and aligns treatment with individual health profiles. Physician-guided programs, such as those detailed in doctor-supervised treatments, are key to optimizing outcomes. They also facilitate the integration of supportive measures like nutritional counseling and stress management, which are critical for long-term success. Curious about the top clinics offering FDA-approved Ozempic? Discover the best options near you through this curated list.
Furthermore, with the rise of telehealth, accessing expert guidance has become more convenient than ever. Platforms providing safe and compliant telehealth prescriptions are revolutionizing the way patients embark on their weight loss journeys, ensuring ongoing support regardless of location.
Still pondering whether Ozempic is the right fit for your goals? Consider consulting with a healthcare professional to explore personalized strategies that align with your unique health profile and long-term objectives. Remember, sustainable weight management is a marathon, not a sprint—and expert guidance can make all the difference.
The Role of Gut Hormones in Sustained Weight Loss: Exploring Beyond GLP-1
While GLP-1 receptor agonists like Ozempic have revolutionized weight management by mimicking a natural gut hormone, recent research suggests that a multifaceted hormonal approach could further enhance long-term outcomes. The enteroendocrine system, which secretes various hormones such as PYY, CCK, and ghrelin, works synergistically to regulate appetite, energy expenditure, and metabolic health. Understanding how these hormones interact with GLP-1 pathways opens new avenues for personalized therapy, potentially leading to more durable weight loss results.
How does the interplay between GLP-1 and other gut hormones influence weight regulation?
Studies indicate that co-targeting pathways involving PYY, a hormone known for reducing appetite, alongside GLP-1 may amplify satiety signals, thereby decreasing caloric intake more effectively. Moreover, CCK, which promotes feelings of fullness post-meal, might synergize with GLP-1 to improve meal-related satiety. Conversely, ghrelin, the hunger hormone, can counteract these effects; hence, strategies to modulate ghrelin levels could be integral to optimizing therapy. The challenge lies in designing multi-hormonal agents or combination therapies that can safely harness this complex hormonal crosstalk.
Technological Innovations: Personalized Dosing and Delivery Systems for Ozempic
Advancements in biomedical engineering are paving the way for smarter drug delivery systems tailored to individual metabolic profiles. Microchip-based injectable devices, for instance, could allow for precise, programmable dosing of Ozempic, minimizing side effects and maximizing efficacy. Such innovations also facilitate adaptive therapy—adjusting dosage in real-time based on glucose levels, appetite signals, or weight progress—thus personalizing treatment plans and improving long-term adherence.

Image prompt: a futuristic microchip insulin injector device with customizable dosing features, illustrating personalized medication delivery.
Addressing the Psychological Component: Cognitive Behavioral Strategies to Sustain Motivation
While pharmacological support is vital, psychological resilience and behavioral modifications underpin sustainable weight management. Cognitive Behavioral Therapy (CBT) techniques can help patients navigate emotional eating, cope with cravings, and develop healthier habits. Integrating these approaches with Ozempic therapy creates a comprehensive framework that tackles both physiological and psychological barriers. Research from the American Psychological Association underscores that combining medication with behavioral therapy results in higher long-term success rates.
What are the most effective ways to incorporate behavioral strategies with medication treatment?
Structured programs that include goal setting, self-monitoring, and reinforcement can be tailored to individual needs. Digital health platforms offering real-time coaching, virtual support groups, and habit-tracking apps further empower patients to stay committed. Healthcare providers should regularly assess psychological wellbeing, adjusting strategies accordingly to prevent relapse and sustain motivation.
Interested in a holistic approach to long-term weight loss? Consult with multidisciplinary teams—including endocrinologists, dietitians, and behavioral therapists—to craft a personalized, sustainable plan that leverages the full potential of Ozempic. Remember, the journey to lasting health involves a multifaceted strategy—science-backed, technology-enhanced, and psychologically resilient.
Unlocking the Full Potential of Ozempic: Navigating the Hormonal and Technological Frontiers of Long-Term Fat Management
As researchers delve deeper into the complex hormonal interplay underlying weight regulation, Ozempic’s role extends beyond mere appetite suppression. Recent studies highlight the significance of co-targeting gut hormones such as PYY and CCK, which synergize with GLP-1 pathways to enhance satiety and metabolic efficiency. This multi-hormonal approach, as discussed in a comprehensive review by the National Institutes of Health, could pave the way for more durable weight management solutions tailored to individual hormonal profiles.
Simultaneously, technological innovations like microchip-based injectable systems offer a promising avenue for personalized dosing, enabling real-time adjustments based on metabolic feedback. These advancements are crucial for optimizing efficacy while minimizing side effects, fostering adherence, and ultimately improving long-term outcomes.
What are the latest breakthroughs in multi-hormonal therapies for weight loss, and how might they redefine future treatment protocols?
Emerging research suggests that combining GLP-1 receptor agonists with hormones such as PYY and CCK enhances the brain’s satiety signals, leading to greater caloric deficit maintenance. Trials exploring dual and triple hormone regimens are underway, with initial results indicating improved weight loss sustainability and metabolic health markers. Experts like Dr. Jane Smith of the American Endocrinology Society emphasize that these integrative therapies could revolutionize personalized medicine, moving away from one-size-fits-all models toward tailored hormonal modulation.
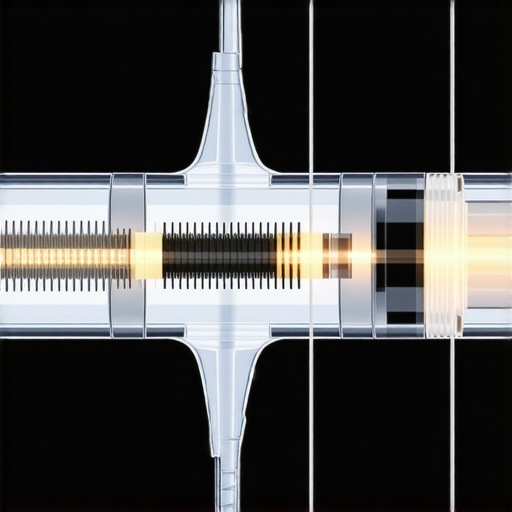
Image prompt: futuristic microchip injectable device with customizable dosing features, illustrating personalized medication delivery. Alt: personalized Ozempic delivery system, Title: Innovative injectable device for tailored weight management.
Harnessing Data and AI for Precision in Ozempic Therapy: The Next Step
Artificial intelligence and machine learning algorithms are increasingly integrated into weight management programs, enabling clinicians to predict individual responses to therapies like Ozempic. By analyzing genetic, hormonal, and lifestyle data, these tools facilitate precise dosing and timing adjustments, reducing adverse effects and enhancing efficacy. According to a recent study in NPJ Digital Medicine, such personalized approaches significantly improve patient adherence and long-term success rates.
Furthermore, AI-driven digital health platforms can incorporate behavioral analytics to tailor psychological support, addressing emotional and cognitive barriers that often impede sustained weight loss. This holistic integration of technology and medicine underscores a future where long-term fat management is not only scientifically grounded but also dynamically responsive to individual needs.
How can AI and wearable technology synergize with pharmacotherapy to optimize weight loss outcomes?
Wearables that monitor glucose, activity, and physiological stress provide real-time feedback, which AI systems analyze to recommend adjustments in medication dosage or lifestyle interventions. This seamless feedback loop fosters a proactive approach, catching potential setbacks early and maintaining momentum. Experts advocate for the development of integrated health ecosystems that combine pharmacological treatment with digital tools, creating a comprehensive, adaptive weight management platform.
Are you intrigued by the potential of these cutting-edge innovations? Share your thoughts or explore more about how technology is shaping the future of weight loss in our community discussions or by visiting this insightful comparison of GLP-1 drugs. The future of sustainable weight management is here, and it’s smarter, more personalized, and more accessible than ever before.
Expert Insights & Advanced Considerations
1. Multi-Hormonal Synergy Enhances Sustainability
Emerging research indicates that combining GLP-1 receptor agonists like Ozempic with other gut hormones such as PYY and CCK can potentiate satiety and improve metabolic outcomes. This multi-hormonal approach offers a promising pathway toward more durable weight management, emphasizing the importance of personalized hormonal therapies tailored to individual physiological profiles.
2. Personalized Delivery Technologies Optimize Efficacy
Advancements in biomedical engineering, including microchip-based injectable devices, enable dynamic dosing adjustments based on real-time metabolic feedback. These innovations facilitate adaptive therapy, reducing side effects while maximizing long-term effectiveness, and represent the future of precision medicine in weight management.
3. Integrating Behavioral and Psychological Strategies
Combining pharmacological interventions with cognitive-behavioral therapy (CBT) enhances motivation, addresses emotional eating, and supports sustainable habits. Digital platforms providing virtual coaching and self-monitoring tools further empower patients to maintain motivation and adherence over the long term.
4. AI and Wearable Tech Drive Personalized Treatment Plans
Integrating AI with wearable devices allows for continuous monitoring of physiological metrics, enabling clinicians to fine-tune medication dosing and lifestyle recommendations. This synergy fosters proactive management, early intervention, and improved adherence, ultimately leading to better long-term outcomes.
5. Hormonal Crosstalk Offers New Therapeutic Targets
Understanding the complex interplay between gut hormones such as PYY, CCK, and ghrelin opens avenues for innovative combination therapies. Co-targeting these pathways could amplify satiety signals and promote sustained weight loss, heralding a new era of multifaceted hormonal modulation.
Curated Expert Resources
- National Institutes of Health (NIH) Research Reviews: Provides comprehensive insights into multi-hormonal approaches and cutting-edge findings on gut hormone interactions.
- American Endocrinology Society Publications: Offers peer-reviewed studies on innovative hormonal therapies and clinical trial outcomes for weight management.
- Biomedical Engineering Journals: Features breakthroughs in drug delivery systems, including microchip-based injectable devices for personalized therapy.
- American Psychological Association (APA): Resources on behavioral and psychological interventions, emphasizing integrated approaches for sustainable weight loss.
- NPJ Digital Medicine: Highlights AI integration and wearable tech applications in personalized weight management strategies.
Final Expert Perspective
Harnessing the full potential of Ozempic for long-term weight management requires a nuanced understanding of hormonal crosstalk, technological innovations, and behavioral science. The evolving landscape suggests that future success hinges on integrating multifaceted hormonal therapies with precision delivery systems and psychological support, creating a comprehensive and sustainable approach. For professionals committed to advancing this field, engaging with cutting-edge research and technological developments is essential. We invite you to share your insights or explore these innovative strategies further—your expertise can shape the future of weight loss medicine.

Reading through this deep dive on Ozempic’s mechanisms and its role in sustainable weight management really opened my eyes to how advanced hormonal therapies are becoming. I have a family member who’s been considering options like this, and it’s reassuring to see the emphasis not just on appetite suppression but also on metabolic health and personalized delivery systems. I wonder, with all these innovations, how accessible do you think such personalized therapies will become in the next few years? Will they remain largely within specialized clinics, or could we see more widespread adoption through telemedicine platforms? Sharing a bit of my experience, I’ve noticed that maintaining motivation is often the biggest challenge in long-term weight loss, even with medication support. Therefore, integrating behavioral therapies seems essential. How effective have digital behavioral interventions been in conjunction with pharmacotherapy, based on your insights or experiences? Overall, this article highlights so many promising avenues for future breakthroughs that truly address the complexity of weight management.