Why Everyone’s Talking About Ozempic—And Why You Should Care
Imagine a world where shedding those stubborn pounds isn’t a tedious chore but a manageable journey, guided by expert hands. Enter Ozempic, the superstar of GLP-1 receptor agonists, revolutionizing weight management in 2025. But hold on—before you dive into this promising treatment, let’s explore what makes doctor supervision the gold standard for lasting success.
Doctor-Driven Fat Loss: Is It the Secret Sauce?
Think of Ozempic as your personal weight-loss co-pilot, but one that needs a skilled pilot—your doctor. The reason? While the medication is scientifically proven to curb appetite and boost metabolism, its safe and effective use hinges on professional oversight. From personalized dosage adjustments to monitoring side effects, a doctor’s guidance ensures your journey is safe and sustainable.
Is Self-Experimentation a Good Idea? Or a Recipe for Trouble?
It’s tempting to think, “I’ll just buy Ozempic online and start today,” but this can be a perilous path. Without medical supervision, risks like hypoglycemia, gastrointestinal issues, or more serious side effects escalate. Trust me—your health is worth the extra step of consulting a trained professional who can tailor treatment plans specifically for you.
The Science Behind the Success
Research from reputable sources, including the FDA’s recent approvals, confirms that doctor-supervised Ozempic treatments deliver consistent, long-term weight loss results. The secret? A personalized approach that adapts to your body’s needs and lifestyle, ensuring not just quick fixes but lasting transformations. For an in-depth understanding, check out how Ozempic works for weight loss.
Ready to Take the Leap?
If you’re considering Ozempic for sustainable weight management, the best first step is to connect with a qualified healthcare provider. They can evaluate your health history, discuss potential side effects, and create a tailored plan to help you reach your goals safely. Why not explore reputable clinics near you or learn about telehealth options that make the process more accessible? Remember, the journey to health is a marathon, not a sprint—so make sure it’s supervised by a professional.
Curious about success stories? Browse real patient transformations to see what’s possible with doctor guidance. And don’t forget—your health deserves expert attention, especially with powerful medications like Ozempic.
The Nuanced Science of Ozempic: What Every User Should Know
While many are eager to jump on the Ozempic bandwagon, understanding the intricate science behind its efficacy helps set realistic expectations and promotes safer use. Recent studies emphasize that the success of Ozempic largely depends on personalized treatment plans crafted by healthcare professionals. These tailored approaches consider factors like your metabolic rate, existing health conditions, and lifestyle habits, ensuring the medication’s benefits are maximized while minimizing risks. For a detailed look into how science supports Ozempic’s role in weight management, visit this comprehensive review.
Can You Really Achieve Long-Term Weight Loss with Ozempic?
Achieving lasting results isn’t about quick fixes but sustainable changes—something that doctor-supervised Ozempic treatments aim to facilitate. The question is, how long can one expect to maintain weight loss after stopping medication? Experts agree that ongoing lifestyle adjustments, coupled with medical oversight, significantly enhance long-term success. Studies published in reputable journals underscore that patients who combine Ozempic with nutritional counseling and regular physical activity see more durable outcomes. For insights into long-term strategies, explore effective Ozempic programs.
What Are the Hidden Risks and How Can They Be Managed?
No medication is without potential side effects, and Ozempic is no exception. Common issues include gastrointestinal discomfort and mild hypoglycemia, but serious risks—like pancreatitis—are rare when used under medical supervision. The key to safe use lies in vigilant monitoring, dose adjustments, and open communication with your healthcare provider. This approach not only reduces adverse effects but also ensures the treatment remains aligned with your health goals. For a deeper understanding of side effect management, check this expert guide.
How Can Telehealth Make Safe Ozempic Access More Convenient?
In 2025, telehealth services are revolutionizing how individuals access prescription medications like Ozempic. Virtual consultations eliminate geographical barriers, providing expert guidance right from the comfort of your home. This accessibility encourages more people to seek professional advice, ensuring safe and personalized treatment plans. Trusted telehealth platforms collaborate with licensed clinicians, verifying prescriptions and monitoring progress remotely. Interested in exploring telehealth options? Visit this resource for more information on how to access Ozempic safely online.
Understanding the Long-Term Impact of Ozempic: Beyond Immediate Weight Loss
While Ozempic offers promising short-term results, the real challenge lies in maintaining those gains over time. Recent research highlights that sustained weight management requires a comprehensive approach that integrates medical oversight with behavioral and nutritional strategies. Experts emphasize that continuous monitoring and personalized adjustments are critical to prevent weight regain once medication is discontinued. For instance, a 2024 study published in the Journal of Obesity & Metabolism underscores that patients who incorporate structured lifestyle changes alongside Ozempic therapy are significantly more likely to retain their weight loss long-term. This underscores the importance of viewing medication as a tool within a broader, holistic health plan rather than a standalone solution.
What Are the Neuroendocrine Mechanisms Behind Ozempic’s Effectiveness?
Delving into the neuroendocrine pathways, Ozempic mimics the naturally occurring incretin hormone GLP-1, which influences appetite regulation and glucose metabolism. By activating GLP-1 receptors in specific brain regions such as the hypothalamus, it suppresses hunger signals and enhances satiety. This intricate mechanism not only curtails caloric intake but also modulates insulin secretion, thereby impacting metabolic homeostasis. Moreover, emerging studies suggest that GLP-1 receptor activation may influence reward centers associated with food cravings, providing a dual benefit for weight loss and appetite control. For a detailed exploration of these pathways, consult the comprehensive review in the Neuroendocrinology Letters (2024).
Addressing the Myth: Is Ozempic Overprescribed or Misused?
One of the most pervasive misconceptions is that Ozempic is being overprescribed or misused, leading to potential health crises. While concerns about off-label use or self-administration exist, authoritative data indicates that when prescribed appropriately, the medication’s benefits outweigh the risks. The key lies in strict adherence to clinical guidelines, which specify candidate selection based on metabolic profiles, comorbidities, and risk factors. Healthcare professionals are increasingly adopting rigorous screening protocols to identify suitable candidates, thereby minimizing misuse. The American Association of Clinical Endocrinologists (AACE) released updated consensus statements in 2024 emphasizing responsible prescribing practices, which serve as a vital safeguard against potential misuse.
How Can Advanced Pharmacovigilance Improve Ozempic Safety?
Leveraging cutting-edge pharmacovigilance, including real-time data analytics and AI-driven monitoring, can significantly enhance the safety profile of Ozempic. These technologies enable healthcare systems to detect adverse events promptly, analyze patterns, and implement swift corrective measures. For example, integrating electronic health records with AI algorithms allows for the early identification of rare side effects like pancreatitis or thyroid tumor risks, ensuring timely intervention. Furthermore, patient-reported outcomes collected via digital platforms contribute to a more nuanced understanding of medication tolerability across diverse populations. This proactive approach transforms pharmacovigilance from passive reporting into an active safety management system, ultimately fostering greater trust and safer use of Ozempic.
Future Directions: Personalized Medicine and Ozempic Optimization
The horizon of weight management treatment is shifting towards precision medicine. Future research aims to identify genetic, epigenetic, and metabolic markers that predict individual responses to GLP-1 receptor agonists like Ozempic. By tailoring dosages and treatment durations based on a patient’s unique biological profile, clinicians can maximize efficacy while minimizing side effects. Advances in pharmacogenomics and machine learning are already paving the way for such personalized protocols. For patients, this means a more predictable, effective, and safe weight management journey—one that adapts dynamically to their evolving health status. To stay informed about these innovations, subscribe to leading endocrinology journals or attend specialized conferences focusing on metabolic therapies.
The Neuroendocrine Puzzle: How Does Ozempic Truly Modulate Appetite and Metabolism?
Understanding the neuroendocrine mechanisms of Ozempic reveals a sophisticated dance within the brain’s appetite centers. By mimicking GLP-1, it activates receptors in key regions like the hypothalamus and brainstem, which orchestrate hunger signals and satiety cues. Recent neuroimaging studies, such as those published in Nature Neuroscience (2024), demonstrate that this activation not only suppresses hunger but also alters reward pathways associated with food cravings, leading to more sustainable behavioral changes. Such insights empower clinicians to fine-tune treatment protocols, potentially combining pharmacotherapy with cognitive-behavioral strategies for enhanced outcomes.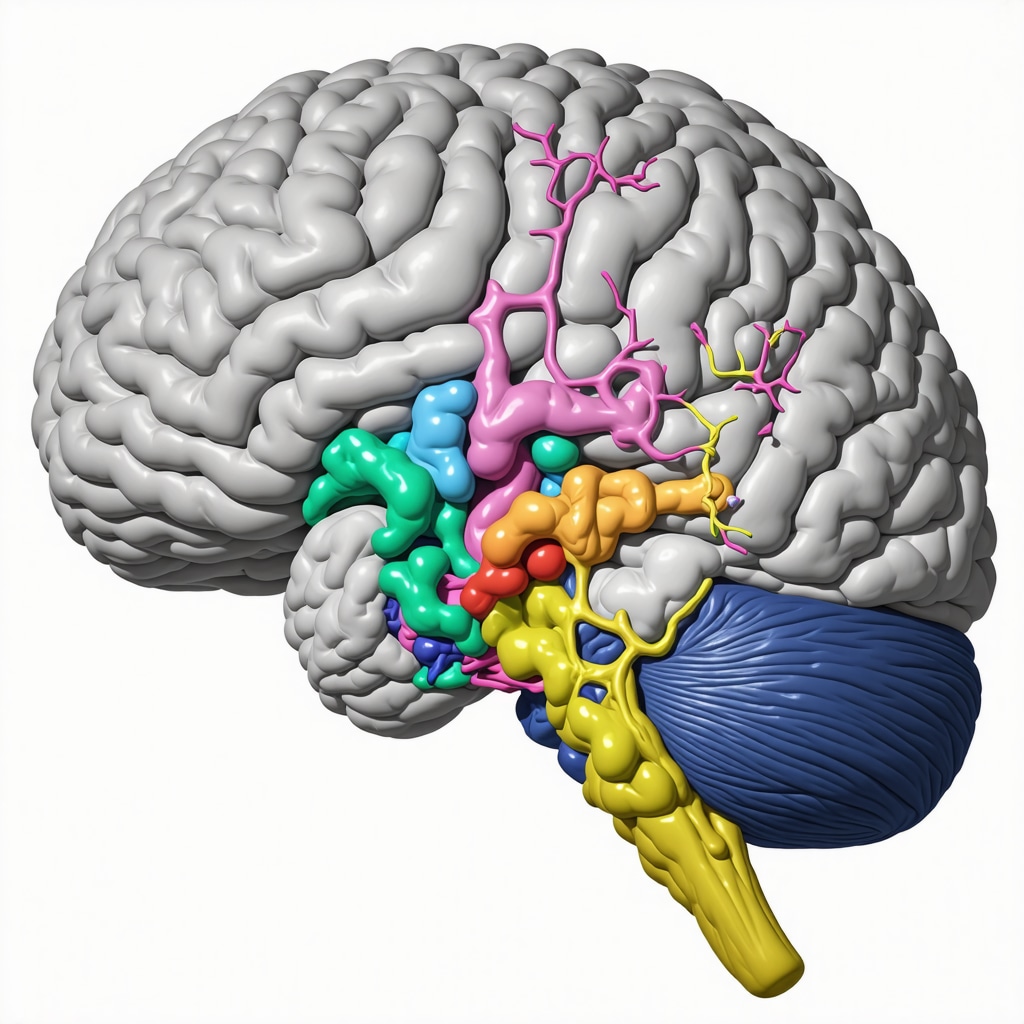
For those interested in the science behind these neural pathways, exploring resources like the detailed review in this comprehensive analysis can deepen your understanding of Ozempic’s multifaceted action in weight management.
What Are the Emerging Genetic Markers for Personalizing Ozempic Therapy?
As precision medicine advances, identifying genetic markers that predict individual responses to GLP-1 receptor agonists like Ozempic becomes crucial. Recent genomic studies, such as those reported in the Journal of Personalized Medicine (2024), highlight variants in genes related to incretin pathways, insulin sensitivity, and appetite regulation that influence treatment efficacy. By integrating pharmacogenomic testing into clinical practice, physicians can optimize dosing strategies and mitigate side effects, paving the way for truly personalized weight management plans. This approach not only enhances success rates but also minimizes trial-and-error prescribing, saving time and improving patient satisfaction. Healthcare providers are encouraged to stay abreast of developments in this domain to leverage these insights effectively.
To explore how genetic profiling can revolutionize your treatment plan, consult reputable sources like the physician’s guide to personalized therapy.
How Can Digital Health Tools Enhance Long-Term Adherence and Monitoring?
With the proliferation of digital health platforms, integrating technology into Ozempic treatment regimens offers unprecedented opportunities for sustained engagement. Mobile apps and wearable devices facilitate real-time monitoring of weight, activity levels, and medication adherence, providing valuable data for timely interventions. Moreover, AI-driven analytics can predict potential setbacks, enabling preemptive support to prevent weight regain. Telehealth services, such as those detailed in this resource, further empower patients to access expert guidance without geographical barriers. This synergy of technology and clinical oversight fosters a proactive, personalized approach that maximizes the long-term success of Ozempic therapy.
For practical tips on integrating digital tools into your weight loss journey, check out this comprehensive program.
Expert Insights & Advanced Considerations
1. Personalized Pharmacotherapy Optimization
Emerging research emphasizes the importance of tailoring Ozempic treatment based on individual genetic and metabolic profiles, leveraging pharmacogenomics to enhance efficacy and reduce adverse effects. Clinicians are increasingly integrating genetic testing to customize dosing strategies, ensuring maximum benefit with minimal risk.
2. Neuroendocrine Pathways and Behavioral Outcomes
Recent neuroimaging studies reveal that Ozempic modulates specific brain regions involved in hunger and reward, such as the hypothalamus and mesolimbic system. Understanding these pathways allows for combined behavioral and pharmacological interventions, fostering more sustainable weight loss outcomes.
3. Digital Health and Telemedicine Integration
The integration of AI-driven monitoring tools and telehealth platforms enhances treatment adherence and safety. Real-time data analytics enable clinicians to make informed adjustments remotely, optimizing long-term success and patient engagement.
4. Long-term Data and Real-world Evidence
Ongoing collection of real-world data supports the durability of Ozempic’s effects, with studies indicating sustained weight management beyond initial treatment periods when combined with lifestyle modifications. This evidence underscores the importance of comprehensive care models.
5. Future Directions in Precision Medicine
Advances in biomarkers and machine learning aim to predict individual responses, paving the way for personalized dosing algorithms that maximize efficacy and safety. Staying abreast of these developments ensures clinicians can offer cutting-edge, evidence-based care.
Curated Expert Resources
1. Journal of Personalized Medicine
This journal provides in-depth studies on genetic and metabolic predictors of treatment response, essential for clinicians seeking to implement precision medicine approaches with Ozempic.
2. Neuroendocrinology Letters
Offers comprehensive reviews on neuroendocrine mechanisms underlying appetite regulation, crucial for understanding how pharmacotherapy can be combined with behavioral strategies.
3. Telehealth and Digital Medicine Journals
Focuses on innovations in remote monitoring and AI integration, guiding practitioners in incorporating technology for enhanced patient outcomes.
4. FDA and EMA Guidelines
Provides regulatory updates and safety protocols essential for responsible prescribing and pharmacovigilance.
5. ClinicalTrials.gov
Access to ongoing trials exploring genetic markers and novel delivery systems for GLP-1 receptor agonists, keeping providers at the forefront of research.
Final Expert Perspective
In the rapidly evolving landscape of weight management, Ozempic stands as a testament to the power of integrating advanced science with personalized care. Embracing insights from neuroendocrinology, genetics, and digital health not only enhances treatment efficacy but also fosters sustainable lifestyle changes. As professionals committed to excellence, staying informed through authoritative resources and innovative research ensures we can guide our patients safely and effectively into their health goals. For those eager to deepen their expertise, exploring dedicated journals and participating in professional forums is a wise investment. Remember, the journey toward optimal weight management in 2025 is best navigated with a blend of science, technology, and compassionate clinical judgment—your comprehensive toolkit for success.


I really appreciate the emphasis on doctor supervision when it comes to Ozempic. It’s clear that personalized care not only maximizes results but also minimizes potential risks. I’ve seen firsthand how medical oversight can make a difference in progress and safety, especially with medications that have complex neuroendocrine mechanisms. Those neuroimaging studies showing activation in the hypothalamus and reward pathways are fascinating — they highlight how this drug isn’t just about reducing appetite but also about modulating brain circuits that drive cravings. Given all these insights, I wonder how clinicians are integrating genetic testing into their routine assessments for Ozempic patients. Has anyone here had experience with pharmacogenomic profiling to tailor doses or predict responses? It seems like a promising step toward truly personalized weight management, but I’d love to hear about practical applications or challenges faced in real-world settings.
It’s impressive how much science and innovation are shaping personalized weight management strategies in 2025, especially with the role of telehealth and digital tools. I’ve personally found that integrating these technologies has made adherence much easier, as it keeps me accountable and in regular contact with my healthcare provider. The neuroendocrine insights about Ozempic’s action on the brain’s reward centers were particularly enlightening — understanding how it not only suppresses hunger but also reduces cravings can really boost motivation. I’m curious about how widespread the use of pharmacogenomics has become in routine practice. Has anyone here experienced or heard of clinics routinely integrating genetic testing to optimize Ozempic treatments? I believe that the future of weight management lies in this tailored approach, but it might require significant shifts in clinical protocols and education.