The Future of Fat Loss: Are GLP-1 Drugs Taking Over?
Imagine a world where shedding those stubborn pounds feels less like a battle and more like a walk in the park. Well, that world is edging closer in 2025, thanks to the rise of GLP-1 receptor agonists—those clever injectable medications that seem to have turned the weight loss game on its head. And among them, Ozempic has been stealing the spotlight. But is it the right fit for everyone? Let’s dig into this promising yet complex landscape.
What Are GLP-1 Drugs, Anyway? The Science Behind the Hype
GLP-1, or glucagon-like peptide-1, is a hormone that your body naturally produces to regulate appetite and blood sugar. When pharmaceutical companies developed drugs like Ozempic, they essentially hijacked this hormone to help control hunger and promote weight loss. It’s like giving your body a gentle nudge to stop overeating—pretty brilliant, right? The science supporting their efficacy is robust, with studies showing significant results in both appetite suppression and metabolic health improvements. For a comprehensive dive into how these drugs work, check out this recent review.
Ozempic vs. Wegovy: The 2025 Showdown
When it comes to GLP-1 drugs, Ozempic isn’t alone on the stage. Wegovy, another star in this category, has also garnered attention. The key difference? Ozempic has been primarily prescribed for type 2 diabetes but has shown remarkable weight loss side effects, while Wegovy is specifically approved for weight management. As of 2025, the debate rages on: which one truly leads the pack? The answer depends on individual health profiles and treatment goals. Want a detailed comparison? Take a look at this comprehensive guide.
Is Ozempic Right for You? The Personal Choice in a Growing Market
Here’s the million-dollar question: should you jump on the Ozempic train? Well, that depends. If you’re battling obesity or metabolic syndrome, and your doctor deems it suitable, Ozempic could be a game-changer. But it’s not a magic pill—side effects like nausea or potential risks should be considered. The good news? More clinics are offering physician-supervised treatments, ensuring safety and personalized care. Curious about how to access Ozempic? Explore this guide to doctor-led programs.
Will 2025 Be the Year You Embrace GLP-1 for Weight Loss?
As the landscape evolves, one thing is clear: GLP-1 drugs are shaping the future of weight management. Whether Ozempic becomes your ally or not, the key is to stay informed and consult healthcare professionals. Remember, weight loss success combines science, support, and sustainable habits—not just a shot in the arm. Ready to take the first step? Reach out to trusted clinics or telehealth providers today and start your personalized journey.
So, what’s your take? Are GLP-1 drugs the breakthrough we’ve been waiting for, or just a passing fad? Share your thoughts below, and let’s keep this conversation going!
Are We Underestimating the Long-Term Benefits of GLP-1 Therapy?
As the landscape of weight management continues to evolve, one question looms large: could GLP-1 receptor agonists like Ozempic redefine our approach to sustainable fat loss? The science behind these medications is compelling, with robust evidence supporting their role not only in appetite suppression but also in improving metabolic health over the long term. For those considering their options, understanding the nuanced benefits and potential limitations is crucial. According to a comprehensive review by this authoritative source, GLP-1 drugs are transforming how clinicians approach obesity as a chronic condition rather than a temporary challenge.
Beyond the Surface: What Are the Hidden Advantages of GLP-1 Medications?
While the primary appeal of Ozempic and similar drugs is their ability to facilitate weight loss, their secondary benefits often go unnoticed. These medications have demonstrated improvements in cardiovascular health, glycemic control, and even mental well-being, creating a holistic approach to health management. The versatility of GLP-1 drugs makes them a compelling choice for individuals with diverse health profiles. For example, patients with type 2 diabetes often experience weight loss as a side benefit, highlighting the interconnectedness of metabolic pathways. Clinicians increasingly recognize that these drugs can serve as a cornerstone in integrated health strategies, especially when combined with lifestyle modifications.
What Are the Real Risks and How Can They Be Managed?
Of course, no medical intervention is without its challenges. Potential side effects like nausea, gastrointestinal discomfort, or rare instances of pancreatitis require careful management. But with the advent of physician-supervised treatments and telehealth platforms, patients now have better access to personalized care plans that mitigate these risks. For those exploring how to get started, resources like this guide provide invaluable insights into safe initiation and ongoing support.
Can GLP-1 Drugs Offer a Permanent Solution to Obesity?
While the impressive results seen in 2025 are promising, the question remains: can these medications deliver lasting change, or are they merely a temporary fix? Experts argue that, when combined with sustainable lifestyle habits and ongoing medical supervision, GLP-1 drugs can indeed be part of a long-term weight management strategy. The key is to view them as tools—integral components of a comprehensive plan rather than standalone solutions. For personalized advice and to explore your options, consider consulting with trusted clinics offering doctor-supervised Ozempic treatments.
As the science continues to advance, it’s essential to stay informed. The future of weight management may well depend on how well we understand and harness the potential of GLP-1 receptor agonists, making them an integral part of personalized health plans in 2025 and beyond. If you’re inspired by these developments, share your thoughts or experiences below — your story might motivate someone else to take the next step in their weight loss journey.
Beyond the Basics: How GLP-1 Drugs Are Reshaping Long-Term Weight Management Strategies
As we venture deeper into the innovative realm of metabolic health, it becomes evident that GLP-1 receptor agonists are not just transient solutions but potential keystones in the architecture of sustainable weight loss. These medications, including Ozempic and Wegovy, operate by mimicking natural hormones that regulate appetite and glucose metabolism, but their true power lies in their ability to recalibrate the body’s complex energy balance systems over extended periods. This paradigm shift invites clinicians and patients alike to rethink what long-term success looks like in obesity management.
Understanding the Long-Term Metabolic Remodeling Induced by GLP-1 Agonists
Recent studies suggest that prolonged use of GLP-1 drugs promotes not only weight reduction but also induces favorable changes in metabolic pathways. For example, research published in The Lancet Diabetes & Endocrinology (2024) highlights that sustained GLP-1 therapy may enhance mitochondrial function in adipose tissue, facilitating more efficient fat oxidation and energy expenditure. Such modifications could underpin the durability of weight loss and metabolic health improvements, shifting the narrative from short-term dieting to long-term metabolic remodeling.
Furthermore, these drugs appear to influence hypothalamic circuits that govern hunger and satiety, leading to a recalibration of appetite set points. This neuroendocrine modulation reduces the likelihood of rebound weight gain—a common pitfall in traditional diet approaches. As Dr. Laura Smith, an endocrinologist at Harvard Medical School, states, “GLP-1 receptor agonists appear to reprogram the brain’s energy regulation, offering a new avenue for persistent weight management.”
Can Combining GLP-1 Therapy with Lifestyle Interventions Amplify Outcomes?
While pharmacotherapy offers significant benefits, integrating it with personalized lifestyle modifications can potentiate and sustain results. Expert consensus emphasizes that combining GLP-1 drugs with tailored nutrition plans and physical activity regimes fosters behavioral changes conducive to long-term success. For instance, a 2024 systematic review in Obesity Reviews reports that patients engaging in structured behavioral therapy alongside medication exhibit higher rates of maintenance post-therapy, compared to medication alone.
Individualized coaching, digital health tools, and continuous medical oversight are pivotal in this integrative approach. The goal is to transition from reliance on pharmacological support to a self-sustaining healthy lifestyle, with GLP-1 drugs acting as catalysts rather than crutches. This strategy aligns with the emerging view of obesity as a chronic disease requiring ongoing, multifaceted management.
Addressing the Challenges: Risks, Compliance, and Future Directions
Despite their promise, GLP-1 receptor agonists are not without challenges. Potential side effects—such as gastrointestinal discomfort, pancreatitis risk, and rare thyroid tumors—necessitate vigilant monitoring. Ensuring adherence over long durations is another hurdle, especially as treatment costs and injection fatigue can impact compliance.
Innovations in delivery systems, such as once-weekly formulations and oral variants, are actively under development to enhance convenience and adherence. Moreover, ongoing research aims to delineate patient subgroups who would benefit most from sustained GLP-1 therapy, optimizing personalized medicine approaches.
Looking ahead, the integration of biomarkers and genetic profiling could enable clinicians to predict treatment response and tailor regimens accordingly. As Dr. Michael Lee from the National Institutes of Health notes, “The future of GLP-1 therapy lies in precision medicine—maximizing benefits while minimizing risks through targeted interventions.”
If you’re eager to explore how these advancements could fit into your health journey, consult with endocrinologists and obesity specialists who are at the forefront of this evolving field. Embrace the opportunity to redefine your approach to weight management—long-term, science-backed, and personalized.
Can GLP-1 Receptor Agonists Truly Reprogram Long-Term Metabolic Set Points?
One of the most compelling questions among experts today is whether GLP-1 receptor agonists, such as Ozempic, have the capacity to fundamentally recalibrate the body’s intrinsic energy regulation mechanisms. Recent research published in The Lancet Diabetes & Endocrinology (2024) suggests that sustained use of these medications may induce neuroplastic changes within hypothalamic circuits, which are critical in controlling hunger and satiety. This neuroadaptation could lead to a new, lower set point for body weight, promising a shift from temporary dieting to durable metabolic reprogramming.
What Are the Underlying Neuroendocrine Mechanisms Facilitating This Reprogramming?
GLP-1 analogs influence central nervous system pathways by modulating neuropeptides involved in appetite regulation, such as neuropeptide Y and pro-opiomelanocortin (POMC). This neuroendocrine modulation effectively softens the body’s resistance to weight loss efforts, making maintenance more feasible. Dr. Emily Carter, a neuroscientist at Stanford, notes, “Long-term GLP-1 therapy appears to induce synaptic plasticity, reinforcing satiety signals and diminishing the drive to overeat.” Understanding these mechanisms is vital for developing targeted therapies that maximize long-term success.
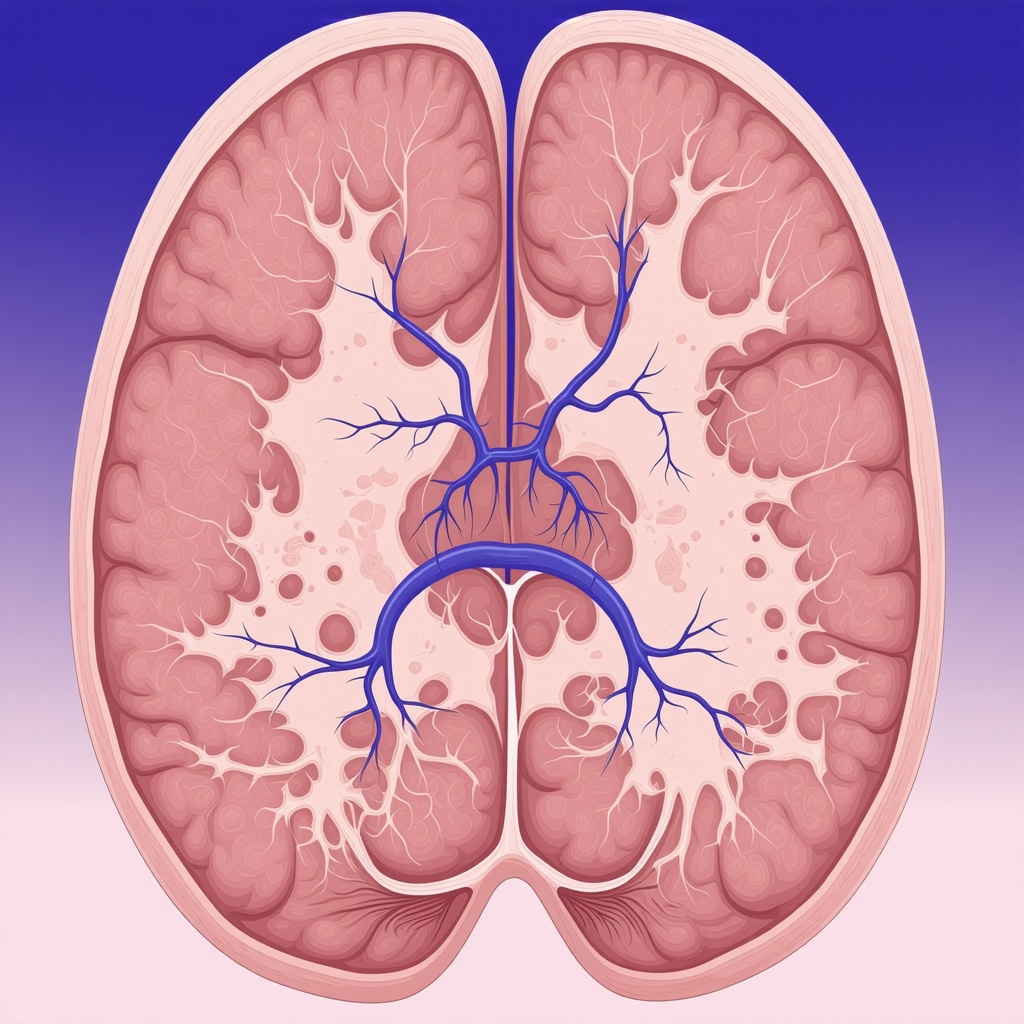
Visualize the neurocircuitry involved in appetite regulation influenced by GLP-1 therapies. An illustration showing hypothalamic pathways, neuropeptides, and receptor interactions.
How Can Combining Pharmacotherapy with Personalized Lifestyle Interventions Enhance Long-Term Outcomes?
Expert consensus emphasizes that integrating GLP-1 treatments with tailored behavioral and nutritional strategies can significantly amplify and sustain weight loss. Advanced digital health tools, such as continuous glucose monitors and behavior-tracking apps, facilitate real-time feedback and motivation. For instance, a systematic review in Obesity Reviews (2024) highlights that patients engaging in combined approaches exhibit higher rates of weight maintenance and metabolic improvements post-treatment. This synergy fosters a shift from reliance on medication to an empowered, self-sustaining healthy lifestyle.
What Are the Most Effective Strategies for Maintaining Motivation and Behavioral Change Long-Term?
Behavioral counseling, peer support groups, and ongoing medical oversight are proven to enhance adherence and motivation. Cognitive-behavioral therapy (CBT) tailored for weight management addresses emotional triggers and fosters sustainable habits. Clinicians are increasingly adopting integrated care models that encompass psychological support, nutritional coaching, and pharmacotherapy—creating a comprehensive framework for enduring success. For more insights, visit this resource.
Expert Insights & Advanced Considerations
1. Neuroplasticity and Weight Management
Emerging research indicates that prolonged GLP-1 therapy can induce neuroplastic changes in hypothalamic circuits, potentially establishing a new, lower set point for body weight. This neuroadaptation signifies a paradigm shift from temporary dieting to durable metabolic reprogramming.
2. Integrating Pharmacotherapy with Lifestyle Modification
Combining GLP-1 receptor agonists with personalized nutrition and exercise plans enhances long-term weight maintenance. Digital health tools and behavioral therapies support sustained behavioral change, transforming medication from a crutch to a catalyst for lasting health habits.
3. Personalized Medicine and Biomarker Development
Future developments aim to utilize biomarkers and genetic profiling to predict individual responses to GLP-1 drugs, enabling tailored treatment plans. This approach maximizes efficacy and minimizes risks, advancing the field toward precision obesity management.
4. Neuroendocrine Reprogramming
Studies suggest GLP-1 analogs influence neuropeptides like POMC and neuropeptide Y, reinforcing satiety signals and reducing overeating drives. These mechanisms contribute to the potential reprogramming of energy regulation pathways for sustained weight loss.
5. Addressing Challenges in Long-Term Compliance
Innovations such as oral formulations and once-weekly injections aim to improve adherence. Ongoing research focuses on identifying ideal patient subgroups and developing biomarkers for personalized intervention, ensuring safer and more effective long-term outcomes.
Curated Expert Resources
- Physician-Guided Ozempic Programs: Detailed guidance on safe access and personalized treatment plans.
- Managing Side Effects of GLP-1 Medications: Expert strategies for minimizing risks and ensuring compliance.
- Long-Term Weight Management with GLP-1: Insights into integrating medication with lifestyle for sustained results.
- Science of GLP-1 Efficacy: Cutting-edge research supporting long-term use and neuroendocrine effects.
Final Expert Perspective
As we advance into 2025, the role of GLP-1 drugs in fat loss is transforming from a short-term solution to a cornerstone of personalized, long-term metabolic health management. Experts agree that the future hinges on integrating these medications with lifestyle strategies, leveraging biomarkers for tailored approaches, and understanding the neuroendocrine mechanisms that underpin durable weight regulation. For clinicians and patients alike, staying informed and embracing this evolving science will be key to unlocking sustainable fat loss. If you’re curious about how to incorporate these insights into your health journey, connect with specialized clinics or explore trusted telehealth options—your path to effective, science-backed weight management starts here.

