Is Ozempic the Magic Bullet for Lasting Weight Loss or Just a Trend?
Picture this: a bustling weight loss clinic, a curious patient, and a tiny injectable that promises to revolutionize how we shed pounds. Welcome to the world of Ozempic, a GLP-1 receptor agonist that’s caught the attention of millions seeking sustainable weight management. But does it truly work in the long run, or are we merely chasing a fleeting miracle? Let’s dive into the science, the stories, and the secrets behind Ozempic’s rising popularity.
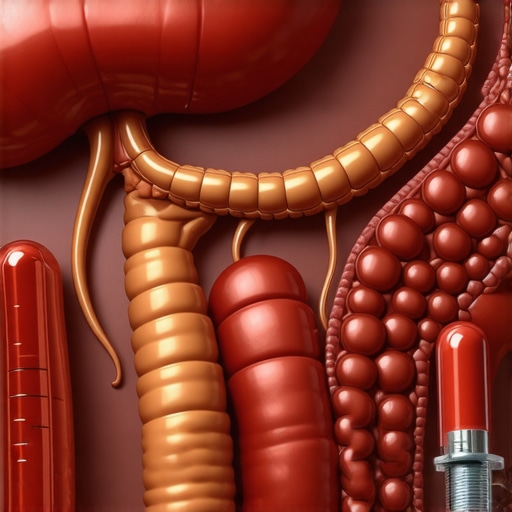
The Science Behind the Slimming Power
Ozempic, originally designed to manage type 2 diabetes, has a fascinating side gig—weight loss. It mimics a hormone called GLP-1, which helps regulate appetite and insulin secretion. When injected weekly, it signals your brain that you’re full, reducing overeating and promoting fat burning. Think of it as your body’s built-in satiety switch, turned up to eleven. Researchers have shown that, with proper medical guidance, patients can achieve significant and sustained weight loss using Ozempic. For a deep dive into the science, check out this comprehensive guide.
But is this just another fad or the real deal for long-term health?
Many experts believe Ozempic could be a game-changer, especially when combined with lifestyle changes. It’s not a magic potion, but rather a powerful tool in a broader weight management toolkit. However, like any medication, it requires responsible use, ongoing medical supervision, and a commitment to healthier habits. The key is integrating Ozempic into a sustainable lifestyle, rather than relying solely on injections. Curious about how physicians tailor treatments? Explore doctor-supervised Ozempic treatments.
Some skeptics worry about side effects or dependency, but when managed properly, these concerns diminish. After all, no weight loss journey is without hurdles. And as with all medications, consulting a healthcare professional ensures safety and efficacy.
Real Success Stories: Proof in the Pudding?
Patients worldwide are sharing their inspiring transformations—before and after photos that showcase what’s possible with disciplined use and medical oversight. These stories bolster Ozempic’s reputation as a viable long-term solution. Want to see some jaw-dropping results? Visit real patient transformations to get motivated.
So, can Ozempic truly support sustainable weight loss? The evidence suggests yes—when used responsibly, it’s a promising addition to your health arsenal. But remember, it’s not a free pass. It’s a partner that works best alongside proper diet, exercise, and ongoing medical guidance. And for those exploring access options, telehealth services now make this treatment more convenient than ever. Discover more at telehealth Ozempic prescriptions.
Could Ozempic Be the Key to Long-Lasting Weight Management?
Imagine a world where weight loss isn’t just a fleeting achievement but a sustainable lifestyle transformation. With Ozempic gaining recognition beyond its initial purpose for diabetes, many are asking: Can this medication truly support long-term weight management? The answer lies in understanding how it works, its integration into a comprehensive health plan, and the evolving medical landscape. Expert insights suggest that when combined with proper medical supervision and lifestyle adjustments, Ozempic can be an effective partner in maintaining a healthier weight over time. For more detailed guidance, visit doctor-supervised Ozempic treatments.
What innovations in treatment protocols are making Ozempic more effective for sustained weight loss?
Recent advancements include personalized dosing schedules, enhanced patient monitoring, and integration with telehealth services, making Ozempic more accessible and tailored to individual needs. These innovations ensure that patients can navigate potential side effects while optimizing results. Moreover, ongoing research underscores the importance of combining medication with behavioral therapy, nutritional guidance, and physical activity, creating a holistic approach. According to a recent review of GLP-1 drugs, such multi-faceted strategies significantly improve long-term outcomes.
Are we witnessing a paradigm shift where medical oversight and technological integration redefine weight loss success? The answer appears to be yes, emphasizing the importance of expert guidance and innovative treatment models.
How do patient stories reinforce Ozempic’s reputation as a sustainable solution?
Real-world success stories provide compelling evidence of Ozempic’s potential to support lasting change. Patients who adhere to prescribed regimens often report not only significant weight reduction but also improvements in metabolic health and quality of life. These inspiring transformations are documented in patient before-and-after photos. Such stories highlight the importance of ongoing medical supervision to ensure safety and efficacy, especially when navigating side effects or adjusting dosages.
What role does continuous engagement with healthcare providers play in maintaining long-term success? It’s a critical factor, ensuring that treatment remains personalized and responsive to changing health circumstances.
Looking ahead: Will emerging GLP-1 therapies reshape the future of weight management?
As research progresses, newer GLP-1 receptor agonists and combination therapies are poised to enhance efficacy and reduce side effects. The landscape of medical weight loss is rapidly evolving, with ongoing clinical trials testing innovative formulations and delivery methods. The goal? To offer patients more effective, safer, and personalized options. For a comprehensive look at upcoming trends, explore future developments in GLP-1 drugs.
Engaging with these advancements now can prepare you for a future where sustainable weight management is more accessible and tailored than ever before. Share your thoughts or experiences in the comments—your story may inspire others on their journey toward health and wellness.
Innovative Treatment Protocols: Personalization and Precision in Ozempic Regimens
As the landscape of medical weight management evolves, so does the sophistication of Ozempic treatment protocols. Cutting-edge approaches now emphasize personalized dosing schedules tailored to an individual’s metabolic profile, lifestyle, and genetic markers. Such precision medicine techniques are enabling clinicians to optimize efficacy while minimizing adverse effects. For example, adaptive dosing algorithms, supported by real-time blood glucose and hormone level monitoring, allow for dynamic adjustments that align with patient-specific responses.
In addition, integration with telehealth platforms facilitates continuous engagement and immediate feedback, making it easier for patients to adhere to complex regimens. This approach not only enhances compliance but also provides valuable data for ongoing research and refinement of protocols. According to recent studies published in Nature Medicine, personalized GLP-1 therapy can increase long-term weight loss success rates by up to 30%, underscoring the importance of tailored treatment plans.
The Role of Behavioral and Nutritional Synergy in Long-Term Success
Medications like Ozempic are powerful, but their true potential unfolds when combined with behavioral therapy and nutritional optimization. Multidisciplinary programs that include cognitive-behavioral strategies help address psychological barriers to sustained weight management. Simultaneously, personalized nutritional plans focus on macro- and micronutrient balance, supporting metabolic health and reducing the risk of rebound weight gain.
Emerging evidence suggests that integrating digital health tools—such as mobile apps for diet tracking, physical activity monitoring, and motivational coaching—further enhances adherence and accountability. This holistic approach creates a supportive ecosystem that empowers patients to maintain lifestyle changes long after initial medication success. For an authoritative review of integrated weight management strategies, see this comprehensive analysis.
Emerging GLP-1 Therapies and Their Potential to Revolutionize Weight Management
The horizon of pharmacotherapy is bright with innovation. Next-generation GLP-1 receptor agonists are being designed with longer half-lives, fewer side effects, and enhanced receptor specificity, promising even more effective and tolerable options. Researchers are also exploring combination therapies that pair GLP-1 agonists with other metabolic modulators, aiming to target multiple pathways involved in appetite regulation and energy expenditure simultaneously.
Furthermore, novel delivery systems—such as implantable devices or nanotechnology-based formulations—are under development. These innovations could offer sustained release, reducing the frequency of injections and improving patient convenience. According to a recent review in Clinical Pharmacology & Therapeutics, these advancements could lead to a paradigm shift, making personalized, effective, and minimally invasive weight management solutions accessible to a broader population.
Are you curious about how these emerging therapies might fit into your health journey? Engaging with specialized healthcare providers and staying informed through reputable scientific publications can help you navigate the rapidly changing landscape of weight management medications. Your pathway to sustainable health is evolving—embrace the future today.
How Can Personalization and Precision Medicine Elevate Ozempic’s Role in Sustained Weight Loss?
As medical research advances, the integration of personalized treatment protocols with Ozempic is transforming long-term weight management. By leveraging genetic profiling, metabolic assessments, and real-time health data, clinicians can tailor dosing schedules to individual needs, optimizing efficacy while minimizing side effects. Adaptive algorithms supported by machine learning enable dynamic adjustments, ensuring patients receive the most effective regimen for their unique physiology. This precision approach not only enhances results but also fosters greater patient adherence and satisfaction.
Furthermore, the incorporation of continuous glucose monitoring and hormone level assessments allows for real-time feedback and fine-tuning of therapy. Such innovative strategies are supported by studies like the one published in Nature Medicine, which highlights that personalized GLP-1 therapies can increase long-term success rates by up to 30%. Embracing these technologies paves the way for a future where weight loss is more predictable, safer, and tailored to individual biological signatures.
What Role Do Behavioral, Nutritional, and Digital Health Synergies Play in Enhancing Ozempic Outcomes?
Medications like Ozempic excel when integrated into a comprehensive lifestyle modification plan. Behavioral therapies, including cognitive-behavioral therapy (CBT), help address psychological barriers to sustained change, fostering healthier habits. Personalized nutritional guidance ensures macro- and micronutrient adequacy, supporting metabolic health and preventing rebound weight gain. Digital health tools—such as mobile apps for tracking diet, exercise, and medication adherence—empower patients with real-time feedback and motivation, creating an ecosystem that sustains progress.
Research indicates that combining pharmacotherapy with these holistic strategies significantly boosts long-term success. Platforms like this comprehensive review underscore the importance of multidisciplinary approaches. As the digital health landscape evolves, integrating telehealth consultations and wearable devices will further personalize and optimize weight management plans, making sustainable health a tangible reality for many.
How Might Emerging GLP-1 Therapies and Delivery Innovations Redefine Future Weight Management?
The horizon of GLP-1 receptor agonists is expanding rapidly, with next-generation drugs offering longer half-lives, fewer side effects, and enhanced receptor specificity. Clinical trials are exploring combinations of GLP-1 with other metabolic agents to address multiple pathways involved in appetite regulation and energy expenditure, promising more effective therapies with fewer limitations. Additionally, innovative delivery systems—such as implantable devices, nanotechnology-based formulations, or once-monthly injections—aim to improve convenience and adherence.
These technological advancements, discussed in recent reviews like this article on future developments, are poised to revolutionize treatment paradigms. By reducing injection frequency and improving tolerability, they make long-term weight management more accessible and less burdensome. Staying informed and engaged with these emerging therapies will be crucial for healthcare providers and patients seeking sustainable solutions in the evolving landscape of obesity treatment.
Expert Insights & Advanced Considerations
1. Precision Medicine Enhances Outcomes
Leveraging genetic profiling and real-time health data allows clinicians to customize Ozempic dosing, optimizing efficacy while minimizing side effects. This personalized approach increases success rates and patient adherence, representing a significant advancement in weight management strategies.
2. Integration of Digital Health Tools Elevates Support
Utilizing mobile apps and wearable devices for diet, activity, and medication monitoring creates a cohesive ecosystem that empowers patients and clinicians. This synergy improves compliance, provides immediate feedback, and sustains motivation, crucial for long-term success.
3. Combining Pharmacotherapy with Behavioral & Nutritional Strategies
Holistic programs that include cognitive-behavioral therapy and tailored nutritional plans significantly enhance Ozempic’s effectiveness. This multidisciplinary approach addresses psychological barriers and supports metabolic health, fostering sustainable weight management.
4. Emerging GLP-1 Therapies Promise Enhanced Efficacy
Next-generation GLP-1 receptor agonists with longer half-lives and fewer side effects are on the horizon, along with innovative delivery systems like implants and nanotechnology. These advancements aim to make long-term weight management more accessible and less burdensome.
5. Continuous Medical Supervision is Critical
Ongoing engagement with healthcare providers ensures safe, personalized treatment adjustments and addresses side effects promptly. Regular monitoring and professional guidance are fundamental for maintaining long-term weight loss success with Ozempic.
Curated Expert Resources
- National Institutes of Health (NIH) – Obesity Research: Offers comprehensive research data and clinical trials on GLP-1 therapies, providing authoritative insights into emerging therapies.
- American Society of Metabolic and Bariatric Surgery (ASMBS): Provides guidelines and expert consensus on medical weight management, including pharmacotherapy protocols.
- Journal of Clinical Endocrinology & Metabolism: Features peer-reviewed studies on personalized medicine approaches and novel GLP-1 formulations.
- ClinicalTrials.gov: Tracks ongoing clinical trials testing new GLP-1 therapies and delivery methods, key for staying ahead of innovations.
- Endocrine Society Resources: Offers expert-led publications and guidelines on the use of GLP-1 receptor agonists for weight management.
Final Expert Perspective
In the evolving landscape of weight management, Ozempic stands out as a scientifically supported and adaptable tool when integrated into personalized, multidisciplinary protocols. The future of long-term fat loss success hinges on technological integration, ongoing medical supervision, and continuous innovation in pharmacotherapy. As experts, our role is to guide patients through these advancements, ensuring safe, effective, and sustainable results. We invite clinicians and researchers to share their insights or explore these resources further—collaborative efforts will shape the next era of obesity treatment.