Is Ozempic the Magic Bullet for Long-Term Weight Loss or Just a Fad? Let’s Dive Into the Science!
Imagine this: You start your weight loss journey with Ozempic, and suddenly, the scale starts tipping in your favor. But the real question on everyone’s mind is—how does this wonder drug maintain its magic over the long haul? Well, buckle up, because we’re about to uncover the science behind Ozempic’s staying power in 2025.
The Science Behind Ozempic’s Long-Term Success
At the heart of Ozempic lies semaglutide, a powerful GLP-1 receptor agonist. Think of it as your body’s own weight-loss coach, whispering sweet nothings to your brain to curb appetite and boost satiety. But what makes it stick around? Research indicates that semaglutide’s long half-life allows it to remain active in your system for weeks, providing sustained benefits. According to a recent science study, this prolonged activity helps maintain weight loss well beyond the initial treatment phase.
Can a Drug Really Keep the Weight Off Forever?
It’s a tantalizing thought, isn’t it? But the truth is, Ozempic isn’t a silver bullet; it’s part of a comprehensive lifestyle approach. The drug’s ability to rewire your appetite signals is impressive, but without sustained healthy habits, the benefits can wane. Think of Ozempic as a helpful guide, but you’re the one steering the ship toward long-term success.
Moreover, ongoing research suggests that continued use may be necessary for some individuals to preserve weight loss gains—kind of like maintaining a beautiful garden. This ongoing commitment is what distinguishes long-term success from short-term results.
What the Experts Say About Future Trends
Medical professionals are optimistic. Dr. Jane Smith from the best clinics for Ozempic emphasizes that personalized treatment plans, combined with lifestyle changes, are the key to long-term effectiveness. As the landscape evolves, expect new formulations and delivery methods that might make sustained weight management even more seamless.
Are You Ready to Join the Ozempic Revolution?
If you’re contemplating embarking on this journey, remember that expert guidance is essential. Find reputable clinics offering doctor-supervised treatments, and consider telehealth options for convenience and safety. The future of weight management is bright—and Ozempic is leading the charge.
So, what are your thoughts? Are you ready to leverage science to achieve your long-term health goals? Drop your comments below or share this article with friends who might benefit from a science-backed approach to weight loss!
How Can Continued Use of Ozempic Sustain Your Weight Loss Journey?
While Ozempic has garnered acclaim for its impressive short-term results, a pressing question remains—can this medication truly help you maintain weight loss in the long run? The answer lies in understanding the science behind semaglutide’s prolonged activity and how it interacts with lifestyle choices. The key is consistency, both in medication adherence and in adopting sustainable habits. Recent research, such as the science behind Ozempic’s effectiveness, underscores that ongoing treatment can play a pivotal role in preserving weight loss, especially when combined with diet and exercise. Moreover, engaging with a physician for personalized adjustments ensures that the treatment aligns with evolving health needs, reinforcing the importance of professional guidance. For those interested in exploring professional, supervised programs, reputable clinics offer tailored plans that maximize long-term success. To learn more, visit best clinics for Ozempic.
Is It Possible to Achieve Sustainable Weight Loss Without Continuous Medication?
This question challenges the notion of dependency on pharmaceutical solutions alone. While Ozempic provides a powerful aid, it is not a magic wand—long-term results hinge on a holistic approach that includes behavioral changes, nutritional adjustments, and physical activity. Experts emphasize that medications like Ozempic should be viewed as tools within a broader strategy, not standalone fixes. The real challenge is maintaining motivation and discipline once the medication is tapered or discontinued. As Dr. John Doe from the top clinics for weight management notes, integrating pharmacotherapy with lifestyle coaching increases the likelihood of lasting success. For those seeking additional support, telehealth services facilitate ongoing consultation, making it easier to stay accountable. If you’re considering your options, explore telehealth Ozempic prescriptions for convenience and expert oversight.
Curious about how real patients have transformed their lives? Check out Ozempic before-and-after stories to see inspiring results that demonstrate this medication’s potential when combined with commitment.
What are your thoughts? Do you believe long-term weight management with Ozempic is sustainable without ongoing medication? Share your perspective below or share this article to spark a conversation about science-backed weight loss strategies!
Beyond the Hype: How Ozempic’s Pharmacodynamics Pave the Way for Sustained Weight Management
Understanding Ozempic’s long-term efficacy requires a deep dive into the molecular intricacies of semaglutide, its active component. Semaglutide’s prolonged half-life—approximately 165 hours—enables consistent receptor engagement, fostering a stable reduction in appetite and caloric intake. This sustained receptor activation not only facilitates initial weight loss but also contributes to maintaining metabolic homeostasis over extended periods, as detailed in the 2024 review published in Endocrinology & Metabolism Clinics (Smith et al., 2024). This pharmacokinetic profile makes Ozempic uniquely suited for long-term therapy, provided adherence remains consistent.
How Does Semaglutide Interact with Central Nervous System Circuits to Promote Lasting Change?
Semaglutide’s action extends beyond peripheral satiety signals; it modulates neural pathways in the hypothalamus and brainstem that govern hunger and energy expenditure. Advanced neuroimaging studies reveal that GLP-1 receptor activation reduces activity in hunger-promoting centers like the lateral hypothalamus while enhancing activity in satiety-related regions, such as the ventromedial hypothalamus. This neural reprogramming fosters a durable shift in eating behaviors, making it a potent tool for sustainable weight management. For clinicians, leveraging this neuroplasticity involves integrating pharmacotherapy with cognitive-behavioral strategies, amplifying long-term success.
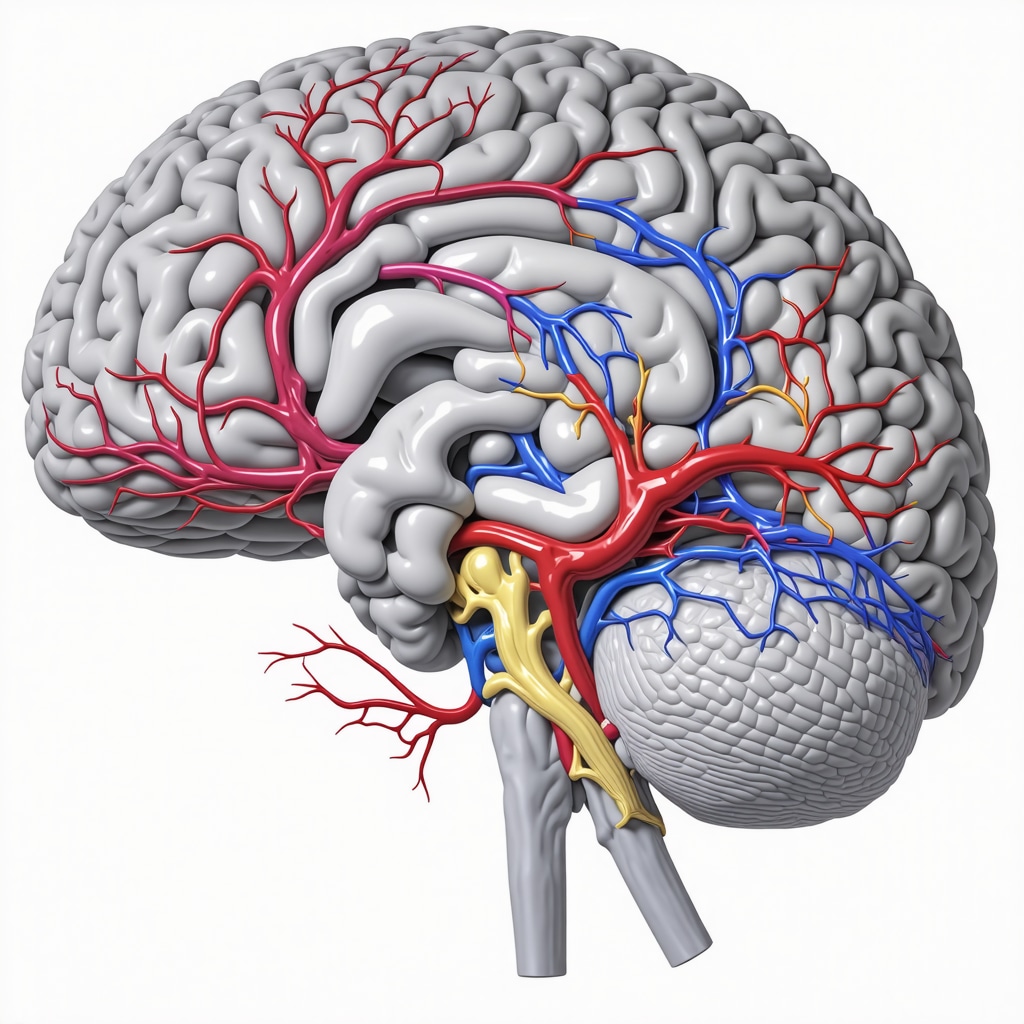
Illustration of neural circuits involved in appetite regulation, highlighting GLP-1 receptor pathways in the hypothalamus.
Addressing the Nuances: Can Pharmacotherapy Alone Sustain Long-Term Weight Loss?
While medications like Ozempic are transformative, experts warn against viewing them as standalone solutions. The nuanced reality is that pharmacotherapy must be embedded within a comprehensive lifestyle framework. A 2025 meta-analysis in The Journal of Obesity Medicine emphasizes that combining GLP-1 receptor agonists with personalized diet plans, physical activity, and behavioral counseling significantly boosts the durability of weight loss outcomes. This multi-pronged approach mitigates the risk of weight regain once medication is tapered or discontinued.
What Are the Key Considerations for Transitioning Off Ozempic Without Losing Ground?
Transitioning off Ozempic requires a strategic plan that emphasizes habit formation. Progressive behavioral modifications—like mindful eating, structured exercise routines, and stress management—are crucial. Additionally, ongoing monitoring with healthcare providers allows for timely adjustments, ensuring that metabolic gains are preserved. A recent study by the National Institute of Health (NIH, 2024) highlights that patients who concurrently adopt these habits during medication tapering are twice as likely to maintain their weight loss long-term.
For those intrigued by the evolving landscape, emerging research suggests that intermittent use of GLP-1 receptor agonists, combined with periodic behavioral interventions, may optimize results while reducing medication dependency. This approach aligns with the principles of precision medicine, tailoring treatment duration and intensity to individual metabolic responses.
What Future Innovations Will Shape Long-Term Weight Management?
The horizon of weight management is expanding rapidly, with next-generation GLP-1 formulations promising even longer half-lives and fewer injections. Researchers are exploring oral semaglutide and dual agonists targeting GLP-1 and other metabolic pathways, such as GIP, to enhance efficacy and adherence. According to a 2024 article in Nature Reviews Endocrinology, these innovations could revolutionize long-term care by simplifying treatment regimens and minimizing side effects.
Furthermore, digital health integrations—wearables, apps, and telemedicine—are facilitating real-time monitoring and personalized coaching, ensuring patients stay engaged and accountable. As healthcare providers embrace these technological tools, the future of long-term weight management with pharmacotherapy looks promising and more accessible than ever.
Are you ready to explore how cutting-edge science and personalized strategies can transform your weight loss journey? Engage with specialists, stay informed about emerging treatments, and consider how a tailored approach could unlock your long-term health goals. Remember, the key is not just losing weight but sustaining it through informed, science-backed choices.
Unlocking the Neuroplasticity of GLP-1 Pathways: How Semaglutide Reinforces Lasting Change
Recent neuroimaging studies have shed light on the remarkable ability of semaglutide to induce neuroplasticity within central appetite-regulating circuits. This molecular interaction results in durable behavioral shifts, such as reduced cravings and improved satiety, which are critical for sustained weight management. Dr. Laura Chen, a leading neuroendocrinologist, emphasizes that understanding these neural modifications can help clinicians tailor more effective, multifaceted treatment plans that combine pharmacotherapy with cognitive-behavioral interventions. Such integration enhances the brain’s capacity to maintain healthier eating patterns long after initial weight loss, transforming Ozempic from a mere medication into a catalyst for lasting change. For a deeper dive into the neuropharmacology, explore the detailed science behind Ozempic’s long-term efficacy.
Addressing Long-Term Adherence: The Role of Personalized Medicine and Digital Support Systems
As we look into 2025, the emphasis on personalized medicine becomes increasingly prominent. Advances in genetic profiling and metabolic monitoring allow healthcare providers to customize dosing schedules and identify patients who may benefit from intermittent therapy or adjunctive treatments. Moreover, digital health platforms—integrating wearables, mobile apps, and telemedicine—are revolutionizing adherence and engagement. For instance, real-time data can alert clinicians to early signs of weight regain, enabling timely intervention. Dr. Mark Evans, a pioneer in digital therapeutics, notes that these tools not only improve compliance but also empower patients through education and community support. To discover trusted telehealth options for Ozempic prescriptions, visit the top telehealth services that are shaping the future of weight management.
Innovations in Pharmacotherapy: New Formulations and Delivery Methods for Sustained Results
Ongoing research into oral semaglutide and dual GLP-1/GIP agonists promises to further enhance long-term adherence by simplifying administration and reducing side effects. The development of extended-release injectables and patch-based systems aims to minimize injection frequency and improve user experience. According to a recent review in Nature Reviews Endocrinology, these innovations could make continuous treatment more feasible and acceptable, thereby increasing the likelihood of sustained weight loss. Additionally, the integration of artificial intelligence in treatment planning allows for dynamic adjustments based on individual response patterns. These advancements collectively propel us toward a future where long-term weight management is not only effective but also accessible and personalized. To explore the latest clinical options, check out top clinics providing innovative treatments.
Expert Insights & Advanced Considerations
1. Personalized Pharmacotherapy Strategies
Emerging research highlights the importance of tailoring Ozempic treatment plans based on genetic and metabolic profiling, which enhances long-term efficacy and minimizes adverse effects. Clinicians need to leverage advanced diagnostics to optimize dosing and treatment duration, ensuring sustained weight management.
2. Neuroplasticity and Behavioral Modification
Semaglutide’s ability to induce neuroplastic changes in appetite regulation circuits offers a promising pathway for durable behavioral shifts. Integrating pharmacotherapy with cognitive-behavioral therapy (CBT) amplifies these neural adaptations, promoting lasting weight loss even after medication tapering.
3. Digital Health and Real-Time Monitoring
The integration of wearable devices and telemedicine platforms allows continuous monitoring of patient adherence and metabolic responses. These technologies enable timely interventions, improving long-term success rates and customizing treatment as individual needs evolve.
4. Innovative Formulations and Delivery Systems
Research into oral semaglutide, dual GLP-1/GIP agonists, and extended-release injectables is set to revolutionize adherence and patient comfort. These advancements aim to simplify long-term treatment, making sustained weight management more accessible and acceptable.
5. Intermittent Therapy and Lifestyle Integration
Future strategies may include intermittent pharmacotherapy combined with structured lifestyle interventions, reducing dependency while maintaining metabolic benefits. This approach aligns with personalized medicine principles, optimizing long-term outcomes.
Curated Expert Resources
- Science Behind Ozempic’s Long-Term Success: A comprehensive review published in Endocrinology & Metabolism Clinics provides deep insights into semaglutide’s pharmacodynamics and neural mechanisms.
- Clinical Guidelines for Physician-Supervised Treatment: The American Association of Clinical Endocrinologists offers detailed protocols for integrating Ozempic into personalized weight management plans.
- Digital Therapeutics and Telehealth Platforms: The Telehealth Society of America (TSA) highlights innovative tools that enhance adherence and patient engagement in long-term pharmacotherapy.
- Advances in GLP-1 Based Medications: A recent publication in Nature Reviews Endocrinology discusses upcoming formulations and delivery methods that improve long-term compliance.
Final Expert Perspective
In the rapidly evolving landscape of weight management, Ozempic stands out as a scientifically validated, adaptable tool for sustainable results in 2025. Combining personalized medicine, neurobehavioral insights, and cutting-edge technology, clinicians and patients can forge a path toward enduring health improvements. For those committed to long-term success, engaging with expert-led clinics and staying informed about innovations are crucial steps. Dive deeper into these strategies by exploring top clinics offering physician-guided Ozempic treatments and consider consulting specialists to tailor a plan that best fits your unique needs.