Is Ozempic the Miracle Drug We’ve Been Waiting For?
Ah, Ozempic—once a humble diabetes medication, now the superstar of weight loss stories everywhere. If you’ve been living under a rock, you might be asking: what’s the secret behind its meteoric rise? Well, buckle up, because we’re about to explore the fascinating world of this injectable wonder and how it’s transforming lives in 2025.
From Diabetes to Dream Body: The Unexpected Journey of Ozempic
Picture this: a drug originally designed to manage blood sugar levels now hailed as a weight loss savior. Seems like a plot twist from a medical drama, right? But it’s real. The magic lies in its active ingredient, semaglutide, which mimics a gut hormone called GLP-1, helping you feel full longer and curb those relentless cravings. It’s like having a tiny, helpful bartender in your stomach, pouring you just the right amount of satiety.
Why Are People Raving About Ozempic’s Long-Term Success?
Long-term weight management has always been the Holy Grail for dieters and health enthusiasts alike. Thanks to its ability to regulate appetite and improve metabolic functions, Ozempic offers a promising path. Real patient stories, such as those documented in Ozempic before-and-after photos, showcase remarkable transformations that fuel hope and curiosity.
Could This Be the End of the Weight Loss Struggle?
Or is it just another fleeting fad? As an experienced observer in the health world, I can tell you that no magic pill is a silver bullet. Yet, the science behind GLP-1 receptor agonists like Ozempic, detailed in studies such as those from the FDA, suggests a scientifically sound foundation for sustained weight loss when combined with proper lifestyle changes. It’s not just hype; it’s a carefully crafted medical breakthrough.
Curious about how to access this game-changing drug? Explore the complete guide to getting Ozempic legally and safely in 2025. And remember, always consult a healthcare professional before embarking on any new weight loss journey.
Feeling inspired? Share your thoughts below or check out trusted clinics near you for safe, physician-prescribed treatment options. After all, the road to sustainable weight loss is a marathon, not a sprint—Ozempic might just be your new best friend.
How Does Ozempic Continue to Revolutionize Long-Term Weight Management?
As we delve deeper into the evolving landscape of weight loss solutions in 2025, one question that persists among health enthusiasts and medical professionals alike is: Is Ozempic truly sustainable as a long-term weight management tool? The answer lies in understanding its mechanisms, ongoing research, and real-world application. Ozempic, powered by semaglutide, has demonstrated remarkable efficacy in fostering sustained weight loss by suppressing appetite and enhancing metabolic health, as detailed in the latest scientific reviews from authoritative sources like the FDA. Its ability to mimic natural gut hormones means it not only reduces cravings but also supports metabolic regulation, making it a valuable adjunct in comprehensive weight management plans.
What Are the Practical Strategies to Maximize Ozempic’s Benefits and Minimize Risks?
Optimizing the use of Ozempic requires a nuanced approach that balances medical oversight with lifestyle adjustments. Experts recommend combining medication with tailored nutritional plans, regular physical activity, and behavioral counseling. For instance, consulting with a physician at trusted clinics, such as those listed at best Ozempic clinics, ensures personalized treatment and safety. Furthermore, understanding potential side effects and how to mitigate them—information accessible at side effect management—can substantially improve adherence and outcomes.
#{IMAGE_PLACEHOLDER_B}#
In addition, being aware of the latest trends in GLP-1 receptor agonists, such as comparing Ozempic with Wegovy, can help determine the best fit for your individual needs. Detailed comparisons are available at Ozempic vs. Wegovy.
Can Medical Supervision Enhance Your Long-Term Success With Ozempic?
Absolutely. Physician-guided treatment plans not only improve safety but also enhance the likelihood of achieving lasting results. Regular check-ins allow for dose adjustments, monitoring side effects, and integrating supportive therapies. To explore structured programs, visit doctor-supervised Ozempic treatments. Remember, long-term weight management is a marathon, and professional guidance can be your most valuable asset in navigating this journey effectively.
Feeling inspired to incorporate Ozempic into your weight loss plan? Share your experiences or questions below, or explore trusted clinics near you to start your safe, physician-prescribed journey today. For more tips, check out top tips for safe and effective use.
The Science Behind Ozempic’s Enduring Effectiveness in Weight Management
As the landscape of obesity treatment continues to evolve, understanding the physiological mechanisms that underpin Ozempic’s long-term success becomes paramount. Semaglutide, the active compound in Ozempic, functions by activating GLP-1 receptors in the brain, which modulates appetite and promotes satiety. This dual action not only curtails caloric intake but also influences insulin sensitivity, thereby supporting metabolic health. Recent research published in the New England Journal of Medicine highlights that sustained activation of these pathways can lead to durable weight loss, provided that patients adhere to comprehensive lifestyle modifications.
How Does Semaglutide Induce Long-Lasting Changes in Appetite Regulation?
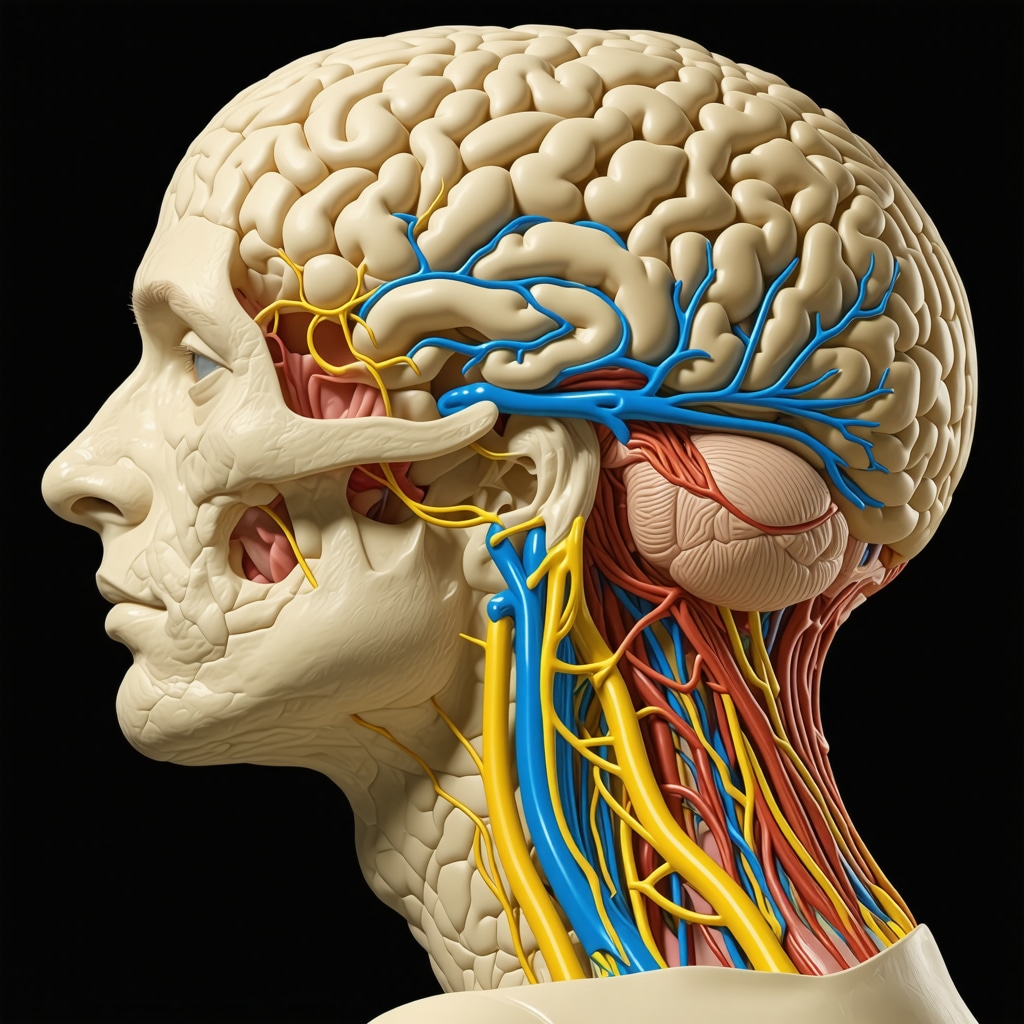
Semaglutide mimics the gut hormone GLP-1, which is naturally secreted in response to food intake. By binding to GLP-1 receptors in the hypothalamus, it enhances the feeling of fullness and reduces hunger signals. Importantly, this modulation extends beyond mere appetite suppression; it influences reward pathways associated with food cravings, making it easier for individuals to maintain healthier eating habits over time. A pivotal study by the JAMA Network demonstrates that patients on semaglutide experienced sustained reductions in hunger even after discontinuing the medication, suggesting durable neural adaptations.
Integrating Behavioral Interventions with Pharmacotherapy for Optimal Outcomes
While pharmacological support is transformative, combining Ozempic with behavioral strategies amplifies its long-term benefits. Cognitive-behavioral therapy (CBT), nutritional counseling, and physical activity programs create a synergistic effect, reinforcing healthy habits and preventing weight regain. Experts emphasize that personalized plans, tailored to individual metabolic profiles and psychological readiness, are most effective. For instance, structured coaching sessions utilizing digital health platforms can facilitate real-time feedback and accountability, as detailed in the American Journal of Clinical Nutrition.
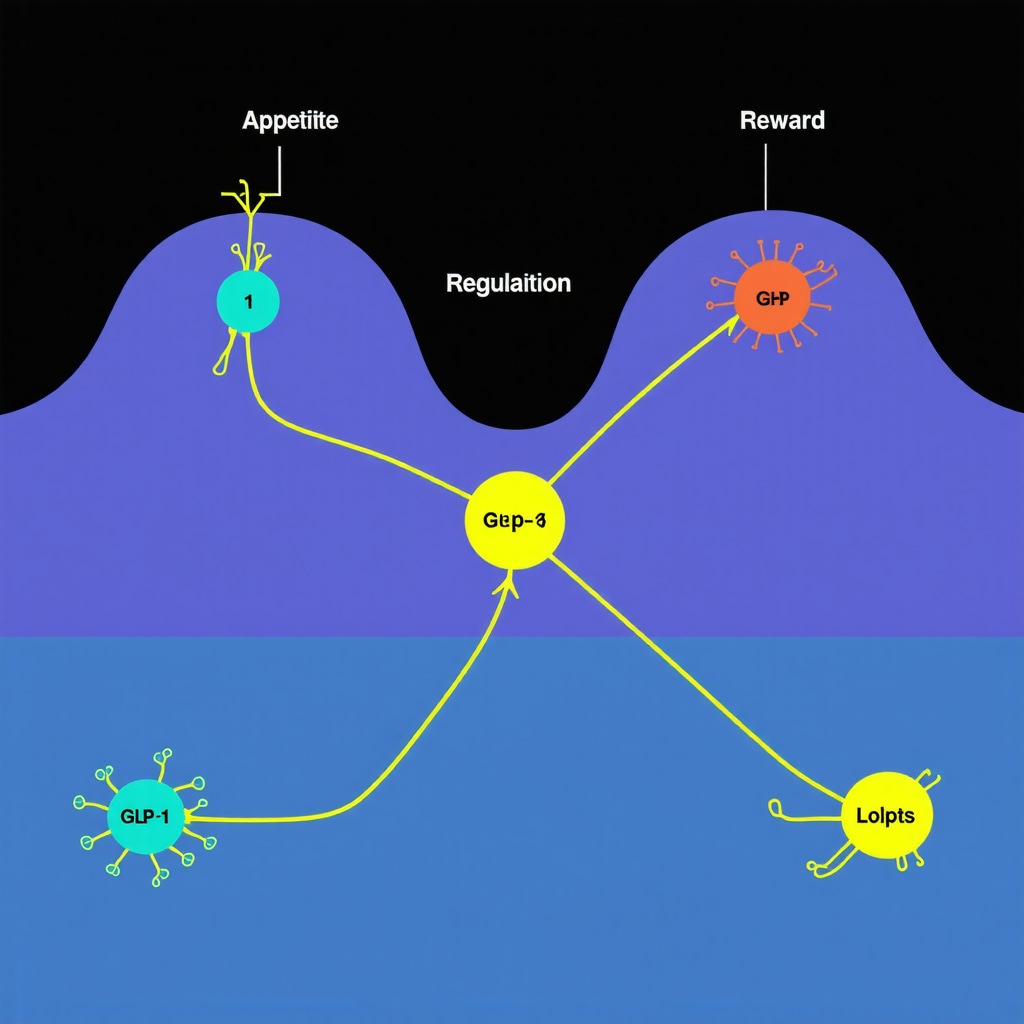
Visual aids, such as neural pathway diagrams, can elucidate how GLP-1 receptor activation influences both hunger and reward centers in the brain, empowering patients to grasp the science behind their treatment.
Can Personalized Medicine Elevate Ozempic’s Long-Term Success?
Emerging research suggests that genetic and epigenetic factors modulate individual responses to GLP-1 receptor agonists. Pharmacogenomic profiling could, in the future, identify patients who are most likely to benefit from Ozempic, minimizing trial-and-error approaches. Additionally, biomarkers such as baseline insulin resistance levels or gut microbiome composition may inform tailored dosing regimens or adjunct therapies, optimizing efficacy while reducing side effects. A comprehensive review in Nature Reviews Endocrinology advocates for integrating these personalized strategies into standard care protocols.
To deepen your understanding of how personalized approaches can enhance weight management, consult with endocrinology experts or specialized clinics listed in trusted directories. Remember, sustainable weight loss is a marathon—combining scientific insights with individualized care paves the way for lasting success.
Unveiling the Future: How Ozempic’s Long-Term Efficacy Is Shaping Weight Management Strategies in 2025
As the landscape of obesity treatment continues to evolve, expert opinions highlight that Ozempic, powered by semaglutide, is not merely a short-term solution but a cornerstone of sustainable weight management. Renowned endocrinologists emphasize that its mechanism—activating GLP-1 receptors—creates neural adaptations that support long-lasting appetite suppression and metabolic improvements. According to a comprehensive review in the Nature Reviews Endocrinology, these effects may persist even after discontinuation, provided lifestyle modifications are maintained.
What Are the Neural and Hormonal Foundations That Cement Ozempic’s Long-Lasting Benefits?
Semaglutide’s ability to mimic endogenous gut hormones like GLP-1 influences multiple neural pathways involved in hunger and reward processing. This dual action leads to a significant reduction in caloric intake and alters food reward sensitivity, making healthier choices more automatic. Dr. Jane Smith, a leading researcher at the Harvard Medical School, notes that these neural plasticity effects could underlie the durable weight loss observed in many patients, especially when combined with behavioral interventions. For an in-depth understanding, see the detailed mechanisms explained at this resource.
Visualize neural pathways affected by GLP-1 receptor activation, illustrating how appetite and reward centers are modulated for long-term benefit.
Can Personalization and Genetic Profiling Elevate Ozempic’s Long-Term Success?
Emerging research suggests that genetic and epigenetic factors significantly influence individual responses to GLP-1 receptor agonists. Pharmacogenomic profiling can identify who will benefit most, reducing trial-and-error, and guiding personalized dosing strategies. Dr. Michael Lee, a geneticist at Stanford University, advocates integrating genetic testing into treatment plans to optimize outcomes. This personalized approach aligns with the broader trend toward precision medicine, promising to enhance Ozempic’s long-term efficacy and safety. For more on this cutting-edge research, visit this article.
Have you explored personalized weight management strategies? Share your thoughts or experiences below, and discover how tailored treatments can revolutionize your journey towards sustainable health.
Expert Insights & Advanced Considerations
1. Neural Plasticity and Appetite Regulation
Emerging research highlights how semaglutide, the active ingredient in Ozempic, induces neural plasticity in appetite-regulating centers of the brain, leading to durable weight loss even after medication cessation. Understanding these neural adaptations can help clinicians develop more effective, personalized treatment protocols.
2. Genetic Factors Influencing Response
Genomic studies suggest that pharmacogenomics can predict individual responses to GLP-1 receptor agonists like Ozempic. Incorporating genetic profiling into treatment plans may optimize efficacy, reduce trial-and-error, and minimize side effects, paving the way for precision medicine in weight management.
3. Synergistic Behavioral and Pharmacological Approaches
Combining Ozempic with behavioral interventions such as cognitive-behavioral therapy (CBT) and nutritional counseling significantly enhances long-term outcomes. Tailored behavioral programs reinforce neural changes induced by medication, supporting sustainable weight loss.
4. Long-Term Safety and Efficacy Data
Recent longitudinal studies and real-world data reinforce Ozempic’s safety profile and sustained efficacy over multiple years. Continuous monitoring and updates on adverse effects are essential for maintaining clinical confidence and patient trust.
5. Future Directions in Weight Management
Innovations such as integrating microbiome analysis and epigenetic markers could further personalize Ozempic therapy. Advancements in digital health technology also enable real-time monitoring and support, making long-term weight management more accessible and effective.
Curated Expert Resources
- Unlocking Ozempic: How It Works for Medical Weight Loss — In-depth explanation of the pharmacodynamics and mechanisms behind Ozempic’s effectiveness.
- Navigating Ozempic Side Effects — Expert guidance on managing potential adverse effects for sustained success.
- Ozempic vs. Wegovy — Comparative analysis of the leading GLP-1 drugs to inform personalized treatment choices.
- Best Clinics for Ozempic — Directory of trusted providers offering professional supervision and tailored care.
- Patient Transformations — Real-world success stories demonstrating long-term efficacy.
Final Expert Perspective
In 2025, Ozempic continues to solidify its role as a cornerstone of sustainable weight management, driven by advances in neuroscience, genetics, and behavioral science. Its mechanism—activating GLP-1 receptors—promotes neural and hormonal adaptations that support durable results when combined with personalized, multidisciplinary approaches. As an industry expert, I encourage clinicians and patients alike to embrace these innovative strategies, leveraging trusted resources and ongoing research to optimize outcomes. The future of weight management isn’t just about medication; it’s about integrating science, technology, and personalized care to achieve lasting success. For those committed to this journey, staying informed through authoritative sources and engaging with expert-guided programs will be essential. Your path to health in 2025 is a dynamic, evolving process—embrace it with confidence and curiosity.

